Holyoke Medical Center Works to Raise Its Profile in the Community
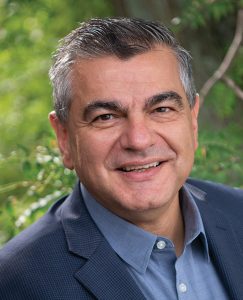
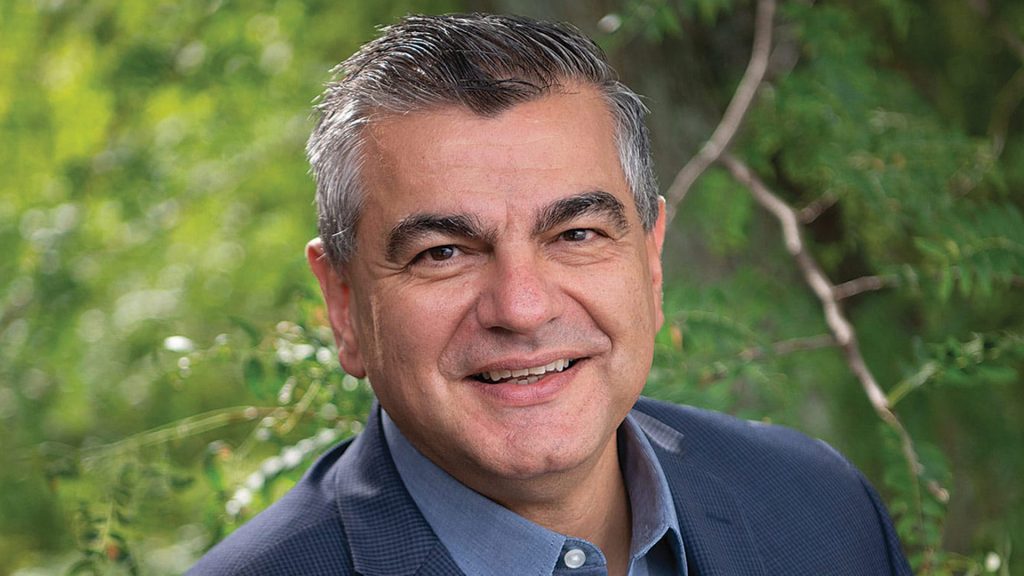
Spiros Hatiras says Holyoke Medical Center isn’t changing what it is and what it does — it’s just doing a better job of communicating it.
He goes on to note that he was a five-pack-a-day smoker and had long battled chronic obstructive pulmonary disease (COPD). His life changed, he implied, when a hospitalist at Holyoke Medical Center intervened.
“She just said, ‘you can fix this.’ You just felt like someone cared,” Morris said into the camera. “If it wasn’t for Holyoke Medical Center, I wouldn’t be going on tour with the Stones this fall.”
And with that 30-second message, now airing on several area television stations, Morris became part of an ambitious new marketing campaign launched by HMC this fall. This spot, like all the others, ends with another voice saying, “Holyoke Medical Center: experience the new standard in patient care.”
It’s not exactly a new standard, in the sense that the staff at HMC has always been caring and compassionate, said Spiros Hatiras, the system’s president and CEO. But it is new in the sense that many from this region, including some living in Holyoke and adjacent communities, are not familiar with the hospital.
This simple fact convinced Hatiras, who took the helm at the medical center 14 months ago, and others at HMC that they had to become more aggressive, and pointed, in their branding efforts.
“We’re not necessarily changing who we are — we’re just doing a better job of communicating it,” said Hatiras, who prefers the phrase ‘brand definition’ to ‘rebranding’ to describe what the system has undertaken. “The basic elements are still here — we are a solid, quality provider, and we’re a hospital of a size that is conducive to personalized care because it’s not very big and intimidating and confusing; we’re located in a great area, and we’re easily accessible. And at the same time, we’re big enough to have the services that most people would need.”
Elaborating, Hatiras said the basic goal of the campaign is to drive home the point that, in most cases, people in the Greater Holyoke area don’t have to drive past HMC on their way to Springfield, or anywhere else, to get the kind of quality care they want and need.
“There’s absolutely no reason, in my mind, why a resident of Holyoke, Chicopee, South Hadley, or Easthampton needs to go far away to another provider to receive the kind of care they can get here,” he explained. “Ultimately, what this campaign is aiming to do is let people know of the things we do and do well and what they can expect here, and keep people in the community.”
The marketing campaign includes a new logo (see page 29), television spots such as Morris’s, print ads (many of them in Spanish), billboards, banners within the hospital, and a revamped website. It’s all part of a multi-faceted initiative to raise HMC’s profile and increase volume, which also includes $2 million in upgrades to the Emergency Department and a new strategic plan.
 Overall, the system’s efforts are focused on putting out a new, stronger message, and then making sure it can back up those words ‘new standard in patient care,’ said Hatiras.
Overall, the system’s efforts are focused on putting out a new, stronger message, and then making sure it can back up those words ‘new standard in patient care,’ said Hatiras.
As for that logo, Hatiras told BusinessWest that it says different things to different people. To him, it speaks of both the region — through the use of the colors blue and green, representing water (Holyoke’s canals and the Connecticut River) and nearby mountains, respectively — and also a new beginning through its use of yellow.
“It’s a like a dawn, a new beginning, a bright day — that kind of feel,” he said. “That’s what we wanted to communicate.”
For this issue, BusinessWest takes an indepth look at this new beginning and the many forces that will shape it.
Ad Infinitum
“I’ve always looked at my patients, and cared for my patients, with the thought that that could be my mother, or that could be my grandmother, and I’ve always treated them as if they were mine, and I’ve treated them as I would want my family to be treated. I love being a nurse.”
That’s another of the 30-second spots airing on area television stations. It stars Lorimar Crus, a registered nurse who has been at HMC for three years. The sentiments she expresses reflect those of the system as a whole, said Hatiras, and sum up nicely both the message that is being sent through these various marketing vehicles, and the current focus of the system.
“While we’re not reinventing ourselves, I will say that we’re enhancing what we do and we’re focusing more on the experience that people have here,” he explained. “On the quality side, we do very well; we’re rated very highly. So what we’re really focusing on are those other qualities of the patient experience, or what people sometimes call the ‘softer skills’ — are we treating people with respect? Are we treating them with compassion? Are we treating people with empathy? Do we really care for people when they come in on a deeper human level?”
Hatiras said the work to revamp the system’s marketing efforts began almost immediately after he arrived last summer, because it was apparent that something needed to be done.
“We started talking about rebranding right away — at least started to think about how we needed to do significantly better in terms of communicating who we are, what we do, and what we do best,” he told BusinessWest, adding that these initiatives are being undertaken simultaneously with efforts to enhance (that’s a word Hatiras would use repeatedly) a culture of caring and compassion.
He said a market survey revealed that HMC’s primary problem wasn’t that people had a negative opinion of it, but that they didn’t have much of an opinion at all. Meanwhile, there was confusion, or ignorance, about the system.
“There were gaps in what people knew about us and about what we did; we still get confused with Holyoke Health Center, and frankly, there were people who didn’t know if we delivered babies here,” he went on, adding that the base of knowledge was broader in Holyoke, but much less so in surrounding communities such as Chicopee and South Hadley.
Hatiras believes HMC’s prior marketing efforts fell short for many reasons. For starters, there wasn’t enough of them, he said, adding that there was a also a lack of cohesion among messages sent by the medical center and its affiliates, River Valley Counseling Center, Holyoke VNA & Hospice Life Care, and Western Mass. Physician Associates, with each entity having its own logo, type style, and marketing strategy.
“No one could ever put it all together — no one really quite understood that the VNA was part of our system and River Valley was part of our system,” said Hatiras. “If your ads don’t all have a certain feel and look, they don’t resonate … if there’s nothing that ties it all together with the whole, it doesn’t make an impact.”
Part of the new branding initiative is broader outreach, especially to the Hispanic community, said Hatiras, adding that ads in Spanish are only a part of this effort.
For example, HMC was the lead sponsor of Holyoke’s annual Puerto Rican Parade in July. The hospital did not have much involvement with the event previously, he noted, and, ironically, Baystate Health was lead sponsor in recent years.
Care Package
But more aggressive marketing and greater outreach are only part of the equation, said Hatiras, returning to that phrase ‘softer skills’ and a recognized need to raise HMC’s game still higher.
“Even these have been core qualities of Holyoke Medical Center,” he said, referring to compassion, respect, and empathy. “What we’re doing now is putting a very significant internal focus on enhancing these qualities and making sure that we develop them further.”
The medical center is working with Pensacola, Fla.-based Studer Group, which, according to its website, “works to bring structure and focus to healthcare organizations through the creation of cultures in which people hold themselves accountable and help set them up to be able to execute quickly.”
HMC has ben working with the company for nearly a year now, and will continue to do so for at least three years, said Hatiras, adding that it takes time to make the kinds of fundamental changes the system is undertaking.
And there are several points of focus within this initiative, said Hatiras, listing everything from private rooms for all patients to revamped food service to valet parking for visitors. A common theme is to provide patients with a greater sense of control over their care.
“We started with some simple things, such as patient amenities,” he explained, “so that when people come here they feel safe, they feel they get treated the right way, and it’s a comfortable environment for them and their families.
“We’re converting all our rooms into private rooms so that there’s space for the family to visit and privacy, and we’ve revamped our food service so that people have choices in what they’re going to eat,” he went on. “When they get admitted, people have very little control over things, in general, and giving them the ability to have control is very important.”
Beyond these initiatives, HMC is also focusing on how the team administering care relates to patients and families.
“Studies have shown that, if physicians take the time to pull up a chair and sit next to the patient at eye level and communicate with them at that level, the interaction is much more meaningful, they get better information out of the patient, and the patient feels they’ll be listened to and understood a lot better than if someone stands at the foot of their bed,” he told BusinessWest. “By giving them that feeling of empathy, compassion, and respect, they heal better and faster.
“It’s just hard science — healing takes good medicine, and it takes good care,” he went on. “But it also takes that human touch, the compassion, the feeling of reducing the patient’s anxiety and making them feel safe.”
One priority for HMC is improving the environment in its Emergency Department, Hatiras noted, adding that the hospital was recently awarded $3.9 million by the Mass. Health Policy Commission to undertake renovations to the ER, and will launch a capital campaign to raise the balance of the projected $6-7 million project.
“The physical environment is very limiting and uninviting,” he said of the current emergency room. “It was built for 15,000, maybe 18,000 visits a year, and we’re doing 45,000.”
Brand Definition
Once the rebranding effort and other initiatives have gained traction, Hatiras said, HMC will conduct another market survey to see if attitudes, and overall awareness of the system and its services, have changed.
He suspects that they will change, and that verification will come in the numbers involving inpatient volume and, overall, the number of people driving elsewhere to receive care.
“The proof is in the pudding,” he said, adding that, while inpatient volume is down across the state, Holyoke’s rate of decline has been greater than in other areas. Reversing this outmigration, as he called it, will require a system-wide focus on not merely branding, but enhancing the patient experience.
And that’s what the system means by a ‘new standard in patient care.’
George O’Brien can be reached at [email protected]

















































 I will argue that all is not well with our healthcare system, and that the average U.S. hospital is facing tremendous challenges now and for the foreseeable future.
I will argue that all is not well with our healthcare system, and that the average U.S. hospital is facing tremendous challenges now and for the foreseeable future.