The Eyes Have It
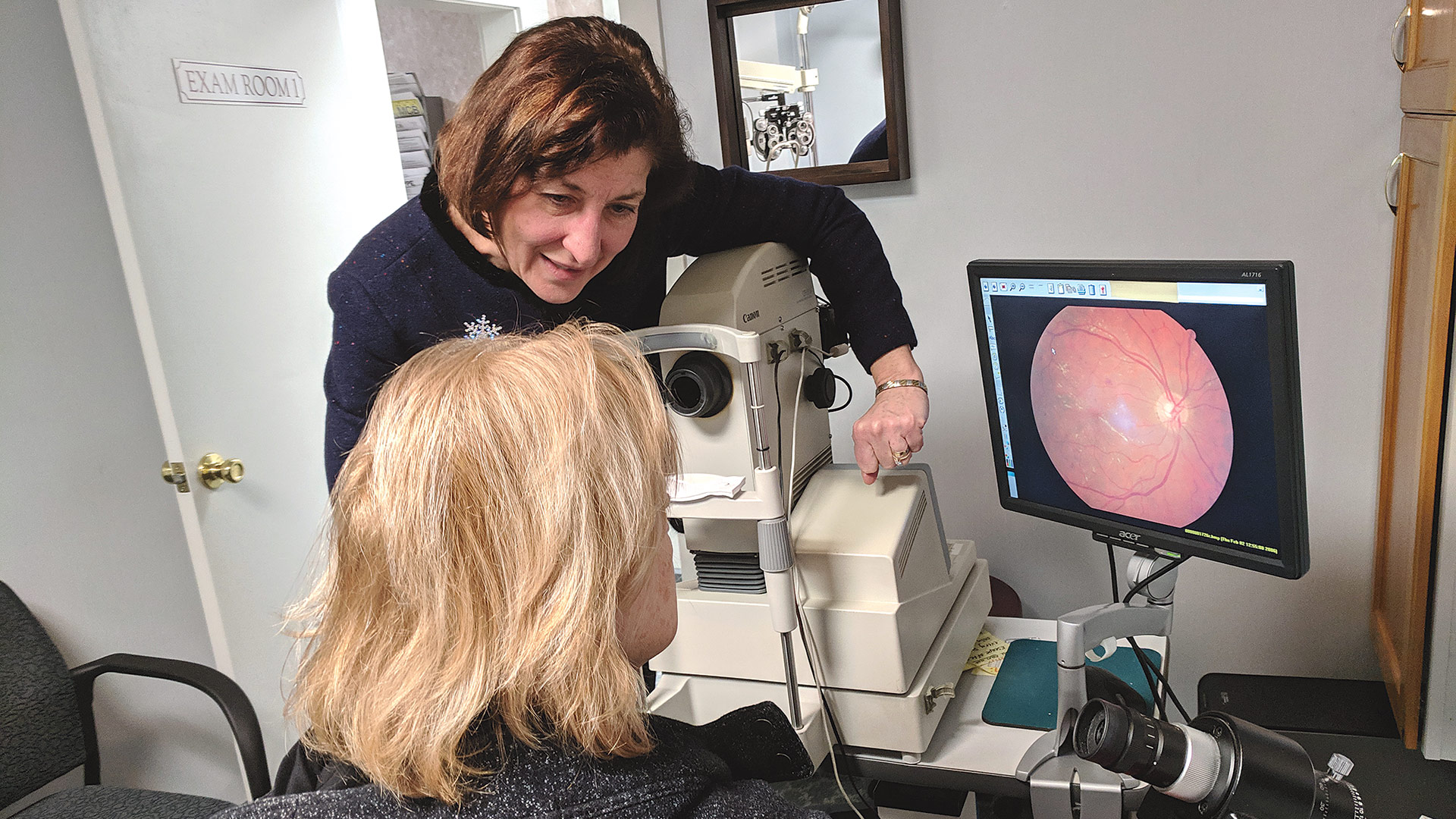
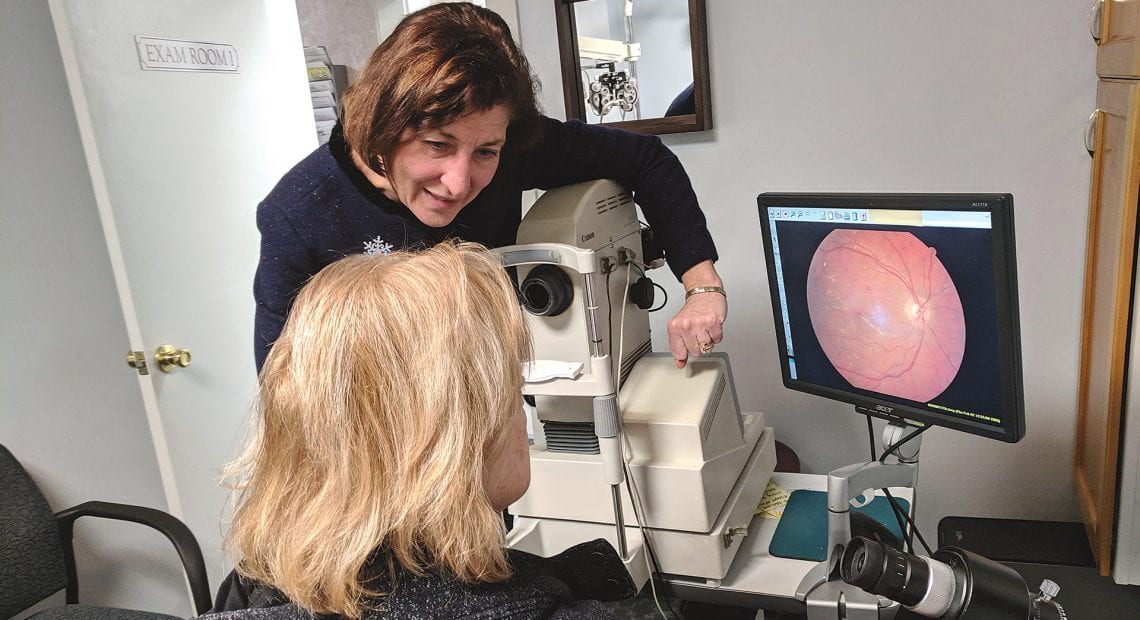
Dr. Camille Guzek-Latka shows a patient an image of her eye and any signs of disease that might be present.
When people think of diabetes, they might think of complications like cardiac disease, but they may not consider what elevated blood-sugar levels can do to their eyes over time. In truth, regular vision exams are a must for diabetics, who are at higher risk of certain conditions, including diabetic retinopathy, that can seriously damage one’s vision. Like diabetes itself, the key to minimizing the risk is often simply diligent lifestyle management.
It’s no secret that diabetes is a growing problem in the U.S., with more than 30 million Americans suffering from this condition that affects blood-sugar levels and leads to a host of complications, from heart disease and stroke to kidney disease, foot ulcers, and eye damage.
It’s that last one that often catches people off guard, said Dr. David Momnie of Chicopee Eyecare.
“A few red flags do go up when we examine patients with diabetes,” he said, explaining that a diabetic eye exam always includes a careful examination of the retina through a dilated pupil, looking for a condition known as diabetic retinopathy (more on that later).
“We also carefully examine the iris for tiny vessels that don’t belong there. We call this condition neovascularization. And we also also look for changes in the lens of the eye, called cataract, and for signs of glaucoma, as both of these conditions occur more frequently in people with diabetes.”
According to the American Diabetes Assoc., about one-fourth of people with diabetes are undiagnosed, which is problematic on many levels, one of which is that diabetics need to have their eyes checked more often — at least once a year — than the general population.
“What’s alarming to us is seeing more young adults and people in their 20s and 30s with type 2 diabetes. The culprit is invariably weight. It’s a global phenomenon as people are spending more time indoors and less time being physically active.”
And, as noted, it’s a condition that’s becoming more prevalent. In Massachusetts alone, diabetes incidence has risen from 3.9% of all residents 25 years ago to about 9% today.
The day BusinessWest visited Chicopee Eyecare early in the afternoon, Dr. Camille Guzek-Latka said she had already seen four patients that day with diabetes — unsurprising because, as a practice that has been around for decades, many patients are older.
“People are living longer, so it’s not surprising to see more people in their 70s, 80s and even 90s diagnosed with diabetes,” Momnie said. “But what’s alarming to us is seeing more young adults and people in their 20s and 30s with type 2 diabetes. The culprit is invariably weight. It’s a global phenomenon as people are spending more time indoors and less time being physically active.”
Yet, not all overweight people develop diabetes, he added, so there are obviously other factors involved — in some cases, there are genetic reasons why the beta cells of the pancreas stop producing enough insulin.
Dr. David Momnie says a key part of seeing diabetic patients is educating them about lifestyle factors that go into their eye health.
“Since the likelihood of developing complications of diabetes like cardiovascular, kidney, and eye problems increase over time,” he added, “young people developing diabetes are more likely to have these problems down the road.”
But with early detection, Guzek-Latka said, patients have a good chance of holding off many of the complications, including eye damage, because they can get a head start on controlling their blood sugar with medications and lifestyle changes.
“We tend to spend a little more time with our diabetic patients,” Momnie added, “because we need to have a frank discussion about lifestyle changes like weight control, a well-balanced diet, and quitting smoking.”
I Can’t See Clearly Now
When diabetes does cause eye damage, it’s often in the form of a disease called diabetic retinopathy, which is caused when too much sugar circulating in the blood damages the tiny retinal blood vessels in the retina, which is like the film of a camera.
“Elevated glucose levels cause damage to blood vessels. The most vulnerable vessels, the ones that show the earliest damage, are the smallest ones that lie farthest from the heart, such as those that supply the fingers, toes, kidneys, and eyes,” said Dr. Andrew Lam, an ophthalmologist at New England Retina Consultants, as well as an attending surgeon at Baystate Medical Center.
Diabetic retinopathy, he explained, is the leading cause of blindness in adults aged 20 to 74. “Treating this condition can be one of the most fulfilling, and frustrating, conditions that a retinal specialist encounters.”
“Elevated glucose levels cause damage to blood vessels. The most vulnerable vessels, the ones that show the earliest damage, are the smallest ones that lie farthest from the heart, such as those that supply the fingers, toes, kidneys, and eyes.”
The two most common eye problems that result from diabetic retinopathy are vitreous hemorrhage and macular edema. Vitreous hemorrhage, or bleeding in the eye, typically results from the formation of neovascular blood vessels in the retina.
“The growth of these vessels is actually the eye’s natural response to the lack of normal blood supply in diabetic eyes, but they are bad because they are apt to leak and bleed,” Lam said, noting that doctors can try to stop the proliferation of neovascular vessels with a laser treatment, and sometimes with injections of a medicine called Avastin.
“But when major bleeding in the eye does occur, it can severely affect a patient’s vision — sometimes taking away almost all the vision,” he went on. “The good news is that our techniques performing vitrectomy surgery to remove the blood are very good, and some of our most grateful patients are those whose vision has been restored after a vitreous hemorrhage has been cleared.”
Diabetic macular edema can be a more frustrating condition to treat, Lam said. This occurs from leaking blood vessels causing swelling in the macula of the eye, the part of the retina responsible for detailed central vision. This in turn causes vision loss and distortion.

Dr. Andrew Lam says diabetic retinopathy is the leading cause of blindness in adults aged 20 to 74 — and it’s increasing in prevalence.
“If we can reduce or eliminate the edema, the patient’s vision often improves, but this is sometimes hard to do,” he explained, noting that weapons in the battle can include eye injections with medicines such as Avastin, Eylea, or steroids, or even laser treatments.
“But the problem is that these treatments don’t always work that well, or for very long,” he went on. “Some patients respond quickly and do well, but others have persistent macular edema and blurry vision, even after repeated treatments.”
Guzek-Latka noted that 7.7 million people in the U.S. had diabetic retinopathy in 2010, a number projected to double to 14.6 million by 2050. Because diabetic retinopathy is progressive and does not cause symptoms until vision loss occurs, she stressed that annual exams are recommended, with more frequent follow-ups if retinopathy is detected. Her practice sends reports on ocular health to the patient’s primary-care physician and schedules appointments with a retinal specialist, like Lam, when necessary.
“One of our problems is that we cannot cure the underlying disease: diabetes,” Lam said. “Still, we fight diabetic retinopathy as diligently and as well as we can. I tell my patients to consider this a life-long battle that requires constant vigilance and sometimes many treatments over time. They must also strive to maintain the best blood-sugar control they can.”
Indeed, he noted, diabetic retinopathy can be managed — and sometimes vision loss can be regained — with treatments, but there is no cure because there is no cure for diabetes itself.
“Early detection, monitoring, and treatment of diabetic retinopathy certainly improve the chance that a patient will enjoy good vision throughout their lifetime,” he continued. “It is important that all diabetics have at least an annual eye exam to detect early signs of retinopathy before it becomes vision-threatening.”
Momnie and his team often use a digital retinal camera to take a picture of any diabetic retinopathy that they find, especially if it’s progressing — and not just because it’s beneficial to them in diagnosing and treating it.
“We also want to get the patient involved in managing their diabetes,” he said. “Seeing the actual damage to their retina is often an incentive to better manage their blood sugars.”
Guzek-Latka agreed. “I find it helpful to show people these pictures because, if you show a person a picture of what’s going on for them, it’s like night and day. It’s a powerful tool not only to document what they’ve got, but to educate them.”
Another instrument for tracking people with diabetic retinopathy is an OCT, which stands for optical coherence tomography, which is a scan that produces a cross-section image of the retina, so they can tell if there is any macular edema. “Any time a diabetic patient has reduced vision, we need to rule out diabetic macular edema, and the OCT gives us that information.”
Early Detection Is Key
Lam said there are many other possible manifestations of diabetes in the eye, including cataracts, neovascular glaucoma, tractional retinal detachment, and optic nerve swelling. These are treated in various ways, sometimes surgically. As the only retina practice in Western Mass., he noted, New England Retina Consultants sees many patients with diabetic retinopathy every day.
Momnie stressed that diabetic eye conditions don’t always present with dramatic symptoms at first. “There are some potentially blinding eye conditions that can develop in people with diabetes without symptoms like blurred vision. And yet, these conditions are treatable if caught early enough.”
Tight blood-glucose control is the key to significantly reducing the incidence and severity of diabetic eye disease, he went on, adding that people with diabetes should discuss with their primary-care physician how to keep their levels in an acceptable range.
Like diabetes itself, some people are at increased risk for developing diabetic eye disease, including women with diabetes who are pregnant, people who have had diabetes for a long time, and cigarette smokers those who simply don’t have their blood sugars under control. African-Americans and Hispanics are also at a greater risk of developing diabetic retinopathy.
Eye appointments for diabetic patients can run slightly over the expected time, Momnie told BusinessWest, but it’s not the exam itself that takes longer. “It’s the time we spend talking to the patient at the end of the exam. We want to discuss prevention with lifestyle changes and the importance of knowing certain numbers like their hemoglobin A1C.”
The A1C is a three-month average of a diabetic’s blood sugar; a reading between 5.7 and 6.4 typically indicates prediabetes, and higher indicates diabetes. “We don’t like to see it above 7.0,” Momnie said. “Generally, the lower the A1C, the better.”
As part of lifestyle changes, Momnie discusses with patients what is known as the glycemic index of carbohydrates, which ranks carb-laden foods by how quickly they break down into simple sugars in the body. Carbohydrates with a lower glycemic index, like oatmeal and whole-wheat pasta, take longer to break down, and are better than foods like potatoes and bread, which have a higher glycemic index. It’s all part of a series of decisions diabetics need to make, he said, to keep their numbers down and complications — like eye damage — at bay.
“Early detection, optimal glucose control, appropriate follow-up care, and timely treatment of diabetic eye disease are key to guarding against loss of vision,” Guzek-Latka said, adding that, occasionally, she will look at someone’s eyes and detect diabetic retinopathy, and then begin asking about other symptoms, and it turns out the patient wasn’t aware they were diabetic. Once they know, however, they can do something about it.
“If you know, you have so much control over what you can do,” she said. “But there are so many people that don’t know they have it that are walking around. If we can catch some of those and steer them in the right direction, that’s a big deal for that individual.”
Joseph Bednar can be reached at [email protected]