Vision 2020
 Few industries change as rapidly — and as dramatically — as the broad, multifaceted realm of healthcare. From oncologists’ use of cancer fingerprinting and gene therapy to facial transplants for accident victims; from cutting-edge protocols to save the lives of stroke and heart-surgery patients to a dizzying array of new treatments to improve vision … the list is seemingly endless, making it impossible to paint a full picture of where healthcare has come in the past decade.
Few industries change as rapidly — and as dramatically — as the broad, multifaceted realm of healthcare. From oncologists’ use of cancer fingerprinting and gene therapy to facial transplants for accident victims; from cutting-edge protocols to save the lives of stroke and heart-surgery patients to a dizzying array of new treatments to improve vision … the list is seemingly endless, making it impossible to paint a full picture of where healthcare has come in the past decade.
But we at BusinessWest wanted to try anyway — and, at the same time, look ahead at what the next decade might bring. So, appropriately, here at the dawn of 2020, we invited a wide range of healthcare professionals to tell us what has been the most notable evolution in their field of practice in the past 10 years, and what they expect — or hope — will be the most significant development to come in the next decade.
The answers were candid, thoughtful, sometimes surprising, but mostly hopeful. Despite the many challenges healthcare faces in these times of advancing technology, growing cost concerns, and demographic shifts, the main thread is still innovation — smart people working on solutions that help more people access better care. After all, healthcare is, at its core, about improving people’s lives, even when they seek it out during their direst moments.
Innovation and promise. That’s what we believe a new decade will bring to all corners of the healthcare world — that is, if these leaders, and countless others like them, have anything to say about it.
Administration
Joanne Marqusee
President and CEO, Cooley Dickinson Health Care

Joanne Marqusee
The most significant recent development in healthcare administration has been a recognition of the role patients play in their own healthcare. “Crossing the Quality Chasm: A New Health System for the 21st Century,” published in 2001 by the Institute for Healthcare Improvement, called for a massive redesign of the American healthcare system. Specifically, it provided “Six Aims for Improvement,” five of which focused on safety, effectiveness, timeliness, efficiency, and equity. Not talked about as much, the sixth aim was to make healthcare ‘patient-centered.’
While we still have a ways to go to truly be patient-centered, we have witnessed a sea change in the past decade in this regard. Patients are increasingly active participants in their care, questioning their doctors and other providers to ensure that they understand their options, using electronic medical records to engage in their care, and speaking out about what they want from treatment or forgoing treatment at the end of life. The best healthcare providers — both organizations and individuals — embrace these changes, welcoming patients as more than recipients of care, but rather active partners in their own care and decision making.
My hope for the most significant development over the next decade has to do with providing universal healthcare coverage while controlling healthcare costs. While we almost have universal coverage in Massachusetts, too much of the nation does not. A hotly debated topic, universal healthcare has many benefits, including increasing access to preventive and routine medical care, improving health outcomes, and decreasing health inequalities.
Surgical Technology
Dr. Nicholas Jabbour
Chairman, Department of Surgery, Baystate Medical Center

Dr. Nicholas Jabbour
The most significant development in surgery over the past decade has been the move toward less invasive surgical approaches made possible through advanced technology. These approaches include robotic and minimally invasive surgery, including intraluminal surgery in areas such as gastroenterology, cardiology, and neurosurgery — for exemple, the passage of an inflatable catheter along the channel inside of a blood vessel to enable the insertion of a heart valve instead of making a large opening in the chest. As a result, we have seen a big shift from inpatient to outpatient surgery with shorter hospital stays and improved post-op recovery.
In the next decade, we foresee these innovations in less invasive surgery will be enhanced by better computing and software integration. This interaction will include the merging of radiological and potentially pathological information — which is currently available in a digital format — with real-time visualization of anatomical structure during surgery. This will offer surgeons the opportunity to improve the accuracy and speed of a surgical procedure while minimizing the risks.
The next decade will also see major innovation in the area of transplantation with the development of tissues or whole organs through bio-engineering manipulation of animal or a patient’s own cells. The integration of this bio-engineering manipulation with currently available technology, such as 3D printing and 3D imaging, will provide patients with the needed tissue or organ — including valves, bone grafts, hernia mesh, skin, livers, and kidneys — in a timely manner. This development will revolutionize the field of transplantation and surgery in general.
Behavioral Health
Karin Jeffers
President & CEO, Clinical & Support Options Inc.

Karin Jeffers
Over the past 10 years, we’ve seen a growing adoption within the behavioral-health and medical fields of holistic treatment models. While the two disciplines were once treated as different animals, the entire health field is now moving to treat both the body and the mind — together. The next 10 years are likely to bring these two fields even closer.
Today, you’re seeing behavioral-health clinicians being hired into physical health practices. Likewise, physical health providers are cross-training to better understand behavioral issues. Whereas, a decade ago, a behavioral-health client might be assigned a therapist or a psychiatrist, they are now gaining access to more robust set of supports, including nursing, case management, recovery coaching, and peer support from those with lived experience. Government mandates and payment model changes are forcing outcomes-based integration, too. Pediatricians, for example, must now do behavioral-health screenings of all youth under 21. In the mental-health space, you’re seeing clinicians ask about weight, exercise, and other physical factors.
We’re seeing significant movement on both the state and federal levels to value outcomes over volume. It’s reflected in the criteria set by the Excellence in Mental Health Act for certified community behavioral-health clinics, a designation CSO has earned, and in the work we have done with the Substance Abuse and Mental Health Services Administration. Our ability to tailor programs, like our grant-funded work at the Friends of the Homeless shelter in Springfield, has literally saved lives among those experiencing homelessness and co-occurring conditions, like substance-use disorders.
In the coming years, we hope to see integrated care models become even more mainstream. Things appear headed in the right direction, but government action establishing payment reform within the behavioral-health field needs to be taken — and the integrated models need to be appropriately funded. Such changes would affirm overall health and wellness to include both physical and behavioral health.
Weight Management
Dr. Yannis Raftopoulos
Director, Holyoke Medical Center Weight Management Program

Dr. Yannis Raftopoulos
Weight management is a rapidly evolving field, and I am fortunate to be part of it. One of the most significant innovations this field has experienced in the last 10 years was the development of a new gastric balloon. Packaged in a small capsule and swallowed with water, the Elipse balloon provides satiety while requiring no procedure or anesthesia for its placement and removal. Together with its excellent safety profile, the Elipse balloon is the least invasive and yet effective weight-loss modality available today. Elipse is manufactured in Massachusetts by Allurion Technologies.
I had the opportunity to be an investigator in the European trial which led to the Elipse market approval in the European Union in 2016. Recently, Holyoke Medical Center was among 10 U.S. sites in which an FDA-regulated trial was conducted. The trial was completed successfully, and Allurion has submitted data requesting FDA approval to market Elipse in the U.S. The balloon’s use in Europe shows that patients can lose more than one-fifth of their initial weight.
A New England Journal of Medicine study reported that 107.7 million children and 603.7 million adults, among 195 countries, were obese in 2015. High body-mass index accounted for 4 million deaths and contributed to 120 million disability-adjusted life-years. Obesity is a chronic disease, and its management requires long-term guidance and close patient-physician communication. Successful collaborations between existing best practices with technology innovations that will allow delivery of effective weight-management care on a massive and global scale could be the most significant evolution in the field in the next 10 years.
Cancer Care
Dr. Hong-Yiou Lin
Radiation Oncologist, Mercy Medical Center

Dr. Hong-Yiou Lin
The advent of new medical oncology drugs has improved control of microscopic and, to a lesser extent, macroscopic disease, allowing local treatments, such as surgery or radiotherapy, to increase survival. To cure cancer, we need to eliminate cancer cells where they started, as well as any microscopic cells traveling through the body. The idea of using immunotherapy to fight cancer has been around for decades, but bringing this idea to the clinic has been hampered by the cleverness of cancer cells knowing how to evade detection by our immune system. Recently FDA-approved immunotherapy either takes away that ‘invisibility cloak’ or wakes up our dormant immune cells to start fighting cancer.
The biggest development in oncology in the next 10 years will be personalized precision medicine, which allows the oncology team to tailor treatment to each patient’s unique cancer biology and life circumstances. Meanwhile, improvements in cancer diagnosis will come from novel PET radiotracers and new MRI sequences that allow for more accurate staging and identification of the best site to biopsy. Pathologists will use novel tools such as genome sequencing to supplement traditional microscopy to subclassify the specific type of cancer within a certain diagnosis instead of grouping into broad categories.
Surgical, medical, and radiation oncologists can then use the above information to decide on the best sequencing between surgery, systemic therapy, and radiotherapy to minimize side effects and maximize cure. Medical oncologists will be able to offer more drugs that target new mutations, overcome drug resistance, increase specificity to a mutation, or better fine-tune immunotherapy, targeting only cancer cells by enlisting gene modification as well as natural killer cells. Radiation oncologists will have new radiomic and genomic tools to personalize the radiation dose and volume, and when to offer radiotherapy.
In short, over the next 10 years, cancer care will continue to move away from the traditional one-size-fits-all model toward a more personalized approach.
Allergy and Immunology
Dr. Jonathan Bayuk
Medical Director, Allergy & Immunology Associates of New England

Dr. Jonathan Bayuk
There have been incredible and exciting advances in allergy and immunology in the last two years. However, the unmet needs of allergic and autoimmune-disease-afflicted patients has grown dramatically in the last 20 years. In response to the increasing prevalence and acuity of allergic diseases and autoimmune diseases, the world has launched products to help address these very severe patients. These medications are indicated for many conditions and work very well. They are generally safe, but are very expensive. These medicines are different than traditional pharmaceutical drugs as they are not chemicals, but biologically derived medicines designed to augment or modify the immune response. As such, they are call biologic medications.
In the field of allergy and immunology, we can now dramatically treat and potentially cure many diseases that in the past were very challenging to manage. The biologic medicines that we have now treat asthma, eczema, allergic disease, and hives. The patient selection is based on severity of their condition, and these medicines are only for moderately to severely affected people. If, as a medical profession, we were to place as many people as possible on these therapies, the cost would be astronomical and not sustainable.
However, is it fair to deny any of these patients access to these treatments who truly need them? I would argue that choice is a very difficult one to make, and as physicians, our primary goal is healing at whatever cost. As a nation, we have a dilemma. Can we afford the medicines we have or not? It is unclear that any serious legislative body is willing to tackle that question. For now, the use of these medicines is changing lives dramatically, and it is an exciting time to be able to use these newer tools to help our patients live better lives.
Eye Care
Dr. David Momnie
Owner, Chicopee Eye Care

Dr. David Momnie
What are the most significant advancements in eye care in the last decade? It depends on whom you ask. Retinal ophthalmologists would probably say it’s the treatment of wet macular degeneration, a leading cause of blindness, with anti-VEGF injections. Cataract surgeons would most likely cite small-incision surgery and new lens implants that often leave patients with 20/20 vision. Glaucoma specialists might tell you it’s the development of MIGS, or minimally invasive glaucoma surgery. These operations to lower the pressure in the eye use miniature devices and significantly reduce the complication rate.
Primary-care optometrists and ophthalmologists would no doubt talk about the advances in optical coherence tomography, a remarkable instrument using light waves that gives cross-sectional pictures of the retina. The technique is painless and non-invasive and is becoming the gold standard in eye care because it has revolutionized the diagnosis and treatment of glaucoma and macular degeneration. For optometrists specializing in contact lenses, using newly designed scleral lenses to restore vision in people with a corneal disease called keratoconus has been a major development. There are many other specialists in eye care, including LASIK surgeons, that have seen remarkable changes in technology.
What will the next decade bring? Artificial intelligence (AI) is becoming more accurate for screening, diagnosing, and treating eye conditions. AI systems can increasingly distinguish normal from abnormal pictures of the retina. Where there is a shortage of ophthalmologists and optometrists, AI screenings combined with telemedicine, providing remote care using communications technology, may be able to find and treat more people who are falling between the cracks of our healthcare system. The term 20/20 is the most common designation in eye care, and the year 2020 will probably usher in another decade of remarkable developments in our field.
Information Technology
Teresa Grogan
Chief Information Officer, VertitechIT

Teresa Grogan
From the perspective of technology that enables healthcare, the biggest game changer of the last decade has been the iPhone — and now, essentially any smartphone.
Steve Jobs introduced the first iPhone in 2007 (a little over a decade ago), and physicians embraced it quickly. It started as a simple tool for doctors (applications like the PDR, or Physicians’ Desk Reference) for looking up drug interactions. Today, it’s a portable EMR, a virtual visit facilitator, and a remote-monitoring device for many healthcare providers, as many patients have embraced — and insisted on — this technology to improve access to care. As the cost decreases and cellular bandwidth improves, the rapid growth of the IoMT (Internet of Medical Things) will place smartphones at the center of the next wave of healthcare technology breakthroughs.
Looking forward, I’d like to see complete elimination of passwords to access electronic information. While there has been some movement toward this with ‘tap and go’ badges and fingerprint readers, a single standard is needed that would work regardless of the software program used. I hope there are greater strides in the creation, deployment, and adoption of other biometric technologies, like iris, face, or voice recognition, so that a healthcare professional could walk into a patient room — or into a hospital — and the computer systems would know his or her identity in immediate and secure fashion. If access to the data needed by a healthcare provider were as easy as turning on a light switch, the improvements in quality of life and efficiency in work for that provider would translate to improved patient outcomes.
Cardiovascular Care
Dr. Aaron Kugelmass
Vice President and Medical Director, Heart and Vascular Program, Baystate Health

Dr. Aaron Kugelmass
We have seen many improvements in cardiovascular care over the last 10 years, but the development, approval for clinical use, and dissemination of transcutaneous aortic valve replacement (TAVR) stands out as the most dramatic. This new technique allows cardiologists and cardiac surgeons, working together, to replace the aortic valve without opening a patient’s chest or utilizing heart-lung bypass, which has been the standard for decades. This less invasive approach is typically performed under X-ray guidance and involves accessing a blood vessel in the leg and guiding a catheter to the heart.
The TAVR procedure was first approved for clinical use in November 2011. It was initially limited to very sick patients, who were not candidates for traditional surgery because of the risk it posed to them. TAVR allowed patients who otherwise could not receive life-saving valve surgery to have their valves replaced with improvement in longevity. With time and experience, the procedure was approved for lower-risk patients as well, and more recently has been approved for the majority of patients, including those with low operative risk. TAVR has been shown to be equivalent or safer than traditional aortic valve-replacement surgery, and is quickly becoming the procedure of choice for most patients who require an aortic valve replacement. Since the procedure typically does not require open-heart surgery, recovery time is much shorter, with some patients going home within a day or two.
In the next 10 years, we expect that similar less-invasive procedures with shorter recovery time will be developed for other heart-valve conditions in patients who otherwise could not receive therapy.
Memory Care
Beth Cardillo
Certified Dementia Practitioner and Executive Director, Armbrook Village

Beth Cardillo
During the last 10 years, neuroscientists have been researching the causes of Alzheimer’s disease. There has been much discussion about which comes first — the amyloid plaque or the fibrillary tangles that develop in the brain, which are roadblocks to cognition, thus causing the difficulties with Alzheimer’s and other related dementia. That question has not been answered yet. Researchers were able to isolate the APOE gene, which is a mutant gene that is found in familial Alzheimer’s disease, helping us to better diagnose it. We have also better understood how diet, exercising both body and brain, and lifestyle contribute to the disease. Currently there are 101 types of dementia, with Alzheimer’s accounting for 75% of cases.
The next 10 years will result in more preventive actions. One major action will be to help people avoid developing type 2 diabetes, which may be labeled the next cause of Alzheimer’s (this type of Alzheimer’s is already being called type 3 diabetes). There has been a major link between sugar in the hippocampus and Alzheimer’s disease. Though there is no cure yet for Alzheimer’s, we are finding more information based on genetics, diet, and PET scans, which can show shrinkage in the brain.
Every year, researchers are more hopeful that a new drug will be developed to eradicate the disease. The last new drug from Biogen was looking hopeful in clinical trials, but that turned out to be not the case. Prevention continues to be at the forefront, as well as participating in clinical trials. More people who do not have dementia or mild cognitive impairment are desperately needed for clinical trials so comparisons of the brain can be made.
Nursing Education
Ellen Furman
Director of Nursing, American International College

Ellen Furman
As in all healthcare, the one thing that can be ascertained is constant change. The same can be said in nursing education today. No longer is the instructor-led lecture method of teaching considered best practice in education, but rather the shift to using class time to apply learned concepts. One way this is done is through the ‘flipped classroom.’ Using this educational modality, students study the concepts being taught preceding the class, followed by class time where students apply these concepts in an interactive activity, thereby developing students’ abilities to think critically, reason, and make healthcare judgements based upon the application of knowledge.
Another change in nursing education is an expanded focus away from pure inpatient (hospital-based) clinical education to outpatient (community-based) clinical education. While hospital-based education remains essential, the realization that most healthcare provided is in outpatient settings has broadened the clinical experiences required to prepare the graduate registered nurse for care provision.
Additionally, with healthcare as complex as it is, nursing students are being taught to be prepared for entry into practice. Education regarding the use of evidence-based practice, how to apply for the licensure examination, preparation to be successful on the National Certification Licensure Exam, nurse residency opportunities, interviewing techniques, transitioning from student nurse to registered nurse, etc. are all taught using a variety of educational modalities based upon the current best available evidence in nursing education.
As we forge ahead in healthcare, nurse educators will continue to evolve to meet healthcare needs through the education of nursing students so as to prepare them to provide care to meet the needs of those we serve well into the future.
Orthotics and Prosthetics
James Haas
Co-owner, Orthotics & Prosthetics Labs Inc.

James Haas
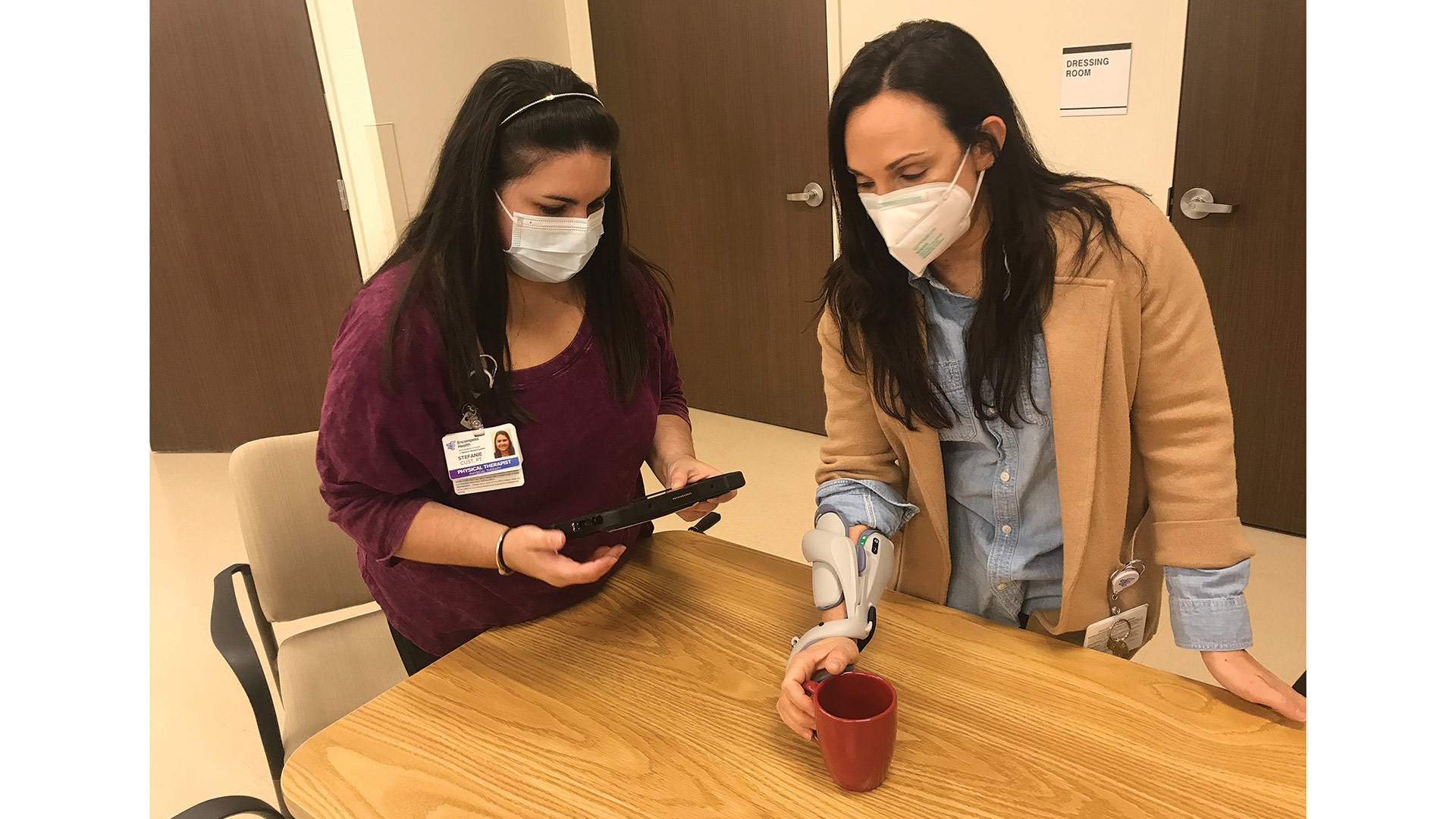
Advances in prosthetic technology have clearly been the most significant development in my field over the past decade. From knees and feet that adapt to different walking speeds and terrains to hands that send sensations of touch to the brain, every aspect of patient care has changed and continues to change at a rapid pace.
Prosthetic feet, knees, and sockets have been greatly impacted. Once made from multi-durometer foams and wood, the prosthetic feet of today are made from carbon, fiberglass, and kevlar laminated with modified epoxy resins. They store energy and adjust to uneven terrain and hills. Microprocessor knees have on-board sensors that detect movement and timing and then adjust a fluid/air control cylinder accordingly. These knees not only make it safer for a person to walk, they also lower the amount of effort amputees must use, resulting in a more natural gait. Sockets once made from stiff materials are now incorporated with soothing gels and flexible adjustable systems that allow a patient to make their own adjustments to improve their comfort.
As for the next decade, I hope to see national insurance fairness. Devices typically last about three to five years. Some people make them last longer, but others, especially growing children, need replacements more often. Many private insurance plans have annual caps and lifetime limits on coverage for orthotics and prosthetics. The Amputee Coalition of America authored insurance-fairness legislation and has lobbied for its implementation for over a decade. This legislation has been ratified in 20 states, including Massachusetts. The Fairness Act requires all insurance policies within the state to provide coverage for prosthetics and orthotics equal to or better than the federal Medicare program and have no coverage caps and lifetime restrictions.
Dental Care
Dr. Lisa Emirzian
Co-owner, EMA Dental

Dr. Lisa Emirzian
The most significant development in the field of dentistry over the past decade has been the integration of digital technology into our daily practices. There are three components of digital dentistry: data acquisition, digital planning, and, finally, the manufacturing of the restoration to be created. Data acquisition today is accomplished with digital radiographs, paperless charting, intra-oral scanners, cone-beam 3D scanners, and video imaging. For the planning process, we now have the ability to merge the data with software that enables computer-aided design and digital smile design, allowing dentists to perform complex procedures, including guided surgical treatments and smile designs, with optimum results. Fabrication and execution of the final restorations can be done in the office or, more often, in laboratories with highly sophisticated digital milling machines, stereolithography, and 3D printing.
In the next decade, we will see data fusion to ultimately create the virtual patient. The next-generation digital workflow will merge intra-oral 3D data with 3D dynamic facial scans, allowing dentists to create 3D smile designs and engineer the dentofacial rehabilitation. The integration of scanners and software will expedite the delivery of ‘teeth in a day.’ In addition, multi-functional intra-oral scanners will allow for early detection of carious lesions and determine risk levels for different patients.
Above and beyond this foreseeable future, artificial intelligence (AI) will be the next paradigm shift. Companies are already looking for big-data collection and deep machine learning to help the practitioner in their everyday chores of diagnosis and treatment. AI cloud-based design platforms will input data, and AI engines in the background will aid in all parts of dental treatment, including diagnosis, design, and fabrication of final restoration.
Let us not forget one thing: the future is all about us — people utilizing technology to enhance the human connection between doctor and patient.
Rehabilitation
John Hunt
CEO, Encompass Health Rehabilitation Hospital of Western Massachusetts

John Hunt
A significant rehabilitation development from the past includes one that may surprise you. Time. A luxury we once knew, time meant patients could recover in a hospital longer after a surgery, an accident, or an illness. Nurses had more time to assess patients to know exactly what they needed. Insurance companies approved longer patient stays through lengthy consideration. Ten years ago, a stroke survivor could recover for two weeks in a hospital and then join us for a rehabilitation stay that would last several weeks.
Today, a three- to five-day stay in the referring hospital, followed by a two-week stay in rehabilitation, is the norm. We are seeing significant decreases in the age of stroke survivors as well as an increase in the number patients who survive with cognitive and physical disabilities. Yet, we also see medical breakthroughs, including the discovery of tissue plasminogen activator (TPA) — nothing short of a miracle. TPA actually reverses the effects of an evolving stroke in patients when used early on, making recoveries easier.
With new advanced technologies being introduced every year, rehabilitation continues to progress at a rapid speed. Looking into the future, evidence-based research will continue to grow to help us make knowledgeable decisions that ultimately impact patient outcomes. Increased clinical expertise will lead to higher functional gains in shorter amounts of time. As a result, acute inpatient rehabilitation will impact the lives of patients like we’ve never seen before.
Hearing Care
Dr. Susan Bankoski Chunyk
Doctor of Audiology, Hampden Hearing Center

Dr. Susan Bankoski Chunyk
The most common treatment for hearing loss is hearing aids. Although digital processing has been available in hearing aids since 1996, the past 10 years have offered great leaps in technology for people with hearing loss. Each generation of computer chip provides faster and ‘smarter’ processing of sound. Artificial intelligence allows the hearing-aid chip to adjust automatically as the listening environment changes, control acoustic feedback, and provide the best speech signal possible. People enjoy the convenience of current hearing aids’ Bluetooth streaming, smartphone apps, and rechargeable batteries.
These features are ‘the icing on the cake,’ but the real ‘cake’ is preservation of the speech signal, even in challenging listening situations. Since the primary complaint of people with hearing loss is understanding in noise, new hearing-aid technology works toward improving speech understanding while reducing listening effort in all environments. This significantly improves the individual’s quality of life.
The negative effects of untreated hearing loss on quality of life are well-documented. Recent research has also confirmed a connection between many chronic health conditions — including diabetes, cardiovascular disease, kidney disease, balance disorders, depression, and early-onset dementia — and hearing loss. This research shows that hearing loss is not just an inevitable consequence of aging, but a health concern that should be treated as early as possible. My hope for the future is that all healthcare providers will recognize the value of optimal hearing in their patients’ overall health and well-being and, just as they monitor and treat other chronic health conditions, they will recommend early diagnosis and treatment of hearing loss.






 “Policymakers do not have to choose between high-quality care and affordability. We have tremendous opportunities for transformative action to support patients and employers.”
“Policymakers do not have to choose between high-quality care and affordability. We have tremendous opportunities for transformative action to support patients and employers.”



































































 I will argue that all is not well with our healthcare system, and that the average U.S. hospital is facing tremendous challenges now and for the foreseeable future.
I will argue that all is not well with our healthcare system, and that the average U.S. hospital is facing tremendous challenges now and for the foreseeable future.










 Few industries change as rapidly — and as dramatically — as the broad, multifaceted realm of healthcare. From oncologists’ use of cancer fingerprinting and gene therapy to facial transplants for accident victims; from cutting-edge protocols to save the lives of stroke and heart-surgery patients to a dizzying array of new treatments to improve vision … the list is seemingly endless, making it impossible to paint a full picture of where healthcare has come in the past decade.
Few industries change as rapidly — and as dramatically — as the broad, multifaceted realm of healthcare. From oncologists’ use of cancer fingerprinting and gene therapy to facial transplants for accident victims; from cutting-edge protocols to save the lives of stroke and heart-surgery patients to a dizzying array of new treatments to improve vision … the list is seemingly endless, making it impossible to paint a full picture of where healthcare has come in the past decade.


















