Hampden Hearing Principal Provides Poignant Listening Points
Sound Reasoning

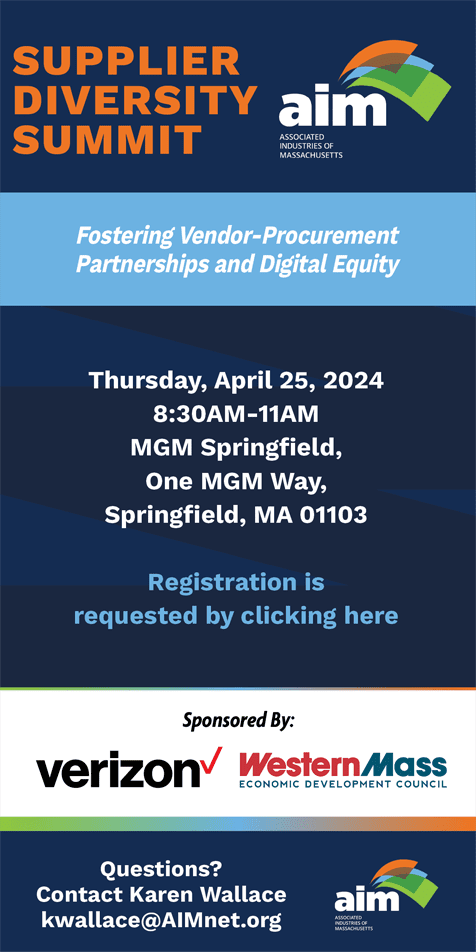
Susan Bankoski Chunyk, here displaying a hearing aid, says new research provides some compelling reasons why individuals should not wait to do something about suspected hearing loss.
Susan Bankoski Chunyk has been quoting the same statistic for years now — because the numbers, to her consistent dismay, haven’t changed appreciably.
The average delay from when someone notices a hearing loss to when that same individual decides to actually do something about it is five to seven years, Bankoski Chunyk, a doctor of audiology practicing in East Longmeadow, told BusinessWest.
The basic reason why hasn’t changed, either. There is a serious stigma attached to hearing aids, she explained, adding that these ever-improving devices have always been associated with age and weakness.
“I’ve had people in their 80s and 90s tell me, ‘I don’t want to look old; those are for old people,’” she said when asked if this stigma was alive and well in the 21st century, noting that such sentiments should certainly answer that question.
What has changed in recent years, however, she went on, are some of the arguments for not waiting five to seven years and instead doing something as soon as hearing loss is noted.
Before, the basic arguments involved quality of life as it related to hearing, both for those suffering the hearing loss and the loved ones and friends coping with it. By way of explanation, Bankoski Chunyk, the region’s first doctor of audiology (more on that later), said she would often quote the line on a bumper sticker used by one of the hearing-aid manufacturers in some of its promotional material, especially as those devices became smaller and less obtrusive: “your hearing aid is less obvious than your hearing loss.”
But in recent years, research has provided Bankoski Chunyk and others like her with more powerful arguments, ones that she believes are already changing some attitudes when it comes to hearing health.
Indeed, numerous studies have linked hearing loss to dementia, depression (especially in women), isolation, loneliness, anxiety, insecurity, paranoia, poor self-esteem, and increased safety risk.
“There’s been a connection established between untreated hearing loss and earlier onset of dementia,” she explained. “The research is going on in multiple sites around the world, and I’m not saying there’s a cause and effect between hearing loss and dementia, but people who have hearing loss and don’t do anything about it are at increased risk of dementia.”
Bankoski Chunyk uses the information from such studies for what has always been a very important part of her practice and is now even more so — education, about everything from the health risks from hearing loss to what causes that condition, meaning everything from diabetes to smoking to noise exposure.
There are many misperceptions about hearing health and hearing loss, as well as that troubling stigma about hearing aids, she said. Overall, there is a general lack of urgency when it comes to hearing and its importance to one’s overall health and well-being, she told BusinessWest, adding that this is true not only for individuals with possible hearing loss, but also their primary-care physicians and the insurance companies that don’t cover hearing aids.
In many cases, hearing loss is often seen as part of the normal aging process, a nuisance rather than a health condition — something to be ignored rather than dealt with directly.
She draws a direct comparison to eye care. “Just because hearing declines with age for some people doesn’t mean it should be ignored,” she explained. “Vision changes are not ignored, even though they are common with age.”

Susan Bankoski Chunyk says that, unfortunately, many misperceptions about hearing health and hearing loss remain, as well as a troubling stigma about hearing aids.
Presenting such arguments and, more importantly, treating those who choose to do something about their hearing loss — hopefully not after five to seven years of waiting for it to get worse — has become a rewarding career choice for Bankoski Chunyk on a number of levels.
More than 30 years after first entering the field, she said she gains great satisfaction from changing someone’s life by enabling them to hear more clearly.
“When a person does come in, they usually kick themselves for waiting so long,” she said. “I love to make people’s lives easier, but I can only do it if they’ll let me.”
For this issue, BusinessWest talked at length with Bankoski Chunyk about her practice and her career, but mostly about some of that recent research she quoted, information she hopes will help change the dynamic when it comes to how people think about their hearing and how it relates to their overall health.
In other words, and as they say in this business, people should take a good listen.
A Positive Tone
Bankoski Chunyk said she first became intrigued by the broad field of audiology when she developed an interest in sign language when she was in high school.
“I got one of those cards with the manual alphabet on it and taught myself how to do all the letters of the sign-language alphabet while on a field trip one day in school, and I was hooked into the whole alternative way of communicating,” she explained, adding that audiology became a career focus in a roundabout way.
Indeed, she enrolled at the University of Connecticut (she’s a native of the Nutmeg State), intending to major in communication disorders with the goal of becoming a speech- language pathologist.
“I’d never heard of audiology before,” she recalled. “But once I started taking the coursework in audiology, I decided that’s where my heart belonged. And I got to combine the sign language for communication with profoundly deaf people with audiology, which covers the whole range of hearing loss.”
Back then, one needed a master’s degree to practice, but, like many professions within healthcare, audiology now requires practitioners to have a doctorate, said Bankoski Chunyk, adding that she earned hers online in 2004 (those who entered the field before the change were not grandfathered in) and thus became the first doctor of audiology in the region.
Her original plan was to get some experience in private practice and then go back to her native Middletown, Conn. and start her own practice there. However, while getting that experience with one of the first audiologists to start her own practice in this region, Kay Gillispie, she became attached to the region and a growing patient base.
The two operated a two-office practice for many years, with Gillispie working in the West Springfield location, and Bankoski Chunyk staffing the East Longmeadow facility. After Gillispie retired, the West Springfield office closed, and Bankoski Chunyk continued practicing in East Longmeadow, where she works with an associate, Jennifer Lundgren Garcia, also a doctor of audiology.
The two perform diagnostic evaluations on adults, fit patients with hearing aids when needed (and do the important follow-up work), and refer patients to specialists when other medical issues present themselves.
Over the years, Bankoski Chunyk said she has seen a great deal of change come to the science — and the business — of audiology.
With the former, she said she’s witnessed profound improvements in hearing-aid technology and ways to fit patients with them and then test and adjust to maximize outcomes.
And with that, she gestured to the something she called real-ear measurement equipment.
“This allows us to measure the sound in an individual’s ear canal without hearing aids in and then with hearing aids in,” she explained, “so that we can make sure that, for soft, medium, and loud sounds coming in, the device is doing the appropriate amount — not overemphasizing, but providing as much benefit as possible.
“By using this, we have a more objective measure than what we used to have,” she went on, adding this advancement, which came to the industry in the mid-’90s, is one of many that enable audiologists to bring real improvement in hearing, and thus quality of life, to patients.
As for the business side of the equation, Bankoski Chunyk said she’s seen it evolve and hearing aids become a commodity of sorts, now available at Costco and Walmart and on Amazon, and perhaps soon to be available over the counter in the same way that prescription eyeglasses are.
And this is where she draws an important distinction between the hearing-instrument specialists working in the Costco Hearing Aid Center and those who have ‘doctor of audiology’ written on their business card.
“A hearing aid is not a retail product; it’s a healthcare product — the FDA classifies them that way,” she explained. “And with hearing aids, there is a lot of review and adjustment and more review to make sure that the results they get are optimized.”
Volume Business
What’s of more importance to Bankoski Chunyk, however, is what hasn’t changed in this field of healthcare, especially that aforementioned lack of urgency and that alarming statistic concerning how long people wait before they call to do something about suspected, or even verified, hearing loss.
“Even physicians will think of hearing loss as ‘oh, you’re getting older, you’re going to have hearing loss,’” she told BusinessWest. “They’ll say, ‘you’ve got normal hearing for your age.’ We cringe when we hear that because there’s no such thing as ‘normal hearing for your age’; you either have normal hearing, or you have a hearing loss, no matter how old you are, and it should be treated.”
She has many concerns in this regard, including the commoditization of hearing aids and the fact that someone will soon be able to buy such equipment over the counter — with potentially serious consequences.
“People might go [buy over the counter] thinking that’s equivalent to what we have, which it won’t be; it won’t be nearly as sophisticated as what we have to offer,” she explained. “And then they’ll have a bad experience, throw it in the drawer, and say, ‘hearing aids don’t work,’ and then reset the clock and wait another five to seven years.”
Of more concern, however, is the recent research showing that those who wait those five to seven years, or longer, are not just missing lines from their favorite TV shows or asking family and friends to repeat themselves because they can’t hear them; they’re inviting other, potential serious health problems.
Indeed, Bankoski Chunyk cited one study showing that people with untreated mild hearing loss had twice the risk of dementia, while those with moderate loss had three times the risk, and those with severe loss had five times the risk of dementia.
“But the people in that study who used hearing aids had no greater risk than people who didn’t have hearing loss,” she went on. “We’re not saying that hearing loss causes dementia; we’re saying that use of hearing aids might help to postpone it, hopefully.”
Bankoski Chunyk said there are many conditions now linked to dementia, and the many reports can lead to confusion and frustration. But when it comes to hearing loss, the link to dementia makes sense.
“It’s been proven that lack of socialization is a big factor in cognitive decline,” she explained. “So we know that what happens with people who have hearing loss — because they’re not wearing hearing aids or they’re not fitted properly — is that they start to retract into themselves and they stop being social, they stop going to parties, they stop going to religious services, they don’t go to the movies, they don’t go out anymore. And that turns into depression, loneliness, anxiety, even to the point of paranoia.
“Gratefully, all this is making some people take things a little more seriously now because everyone is worried about winding up with dementia,” she continued, adding that the hope is that ‘some’ will become ‘most.’
Hearing Is Believing
Returning to the subject of that stigma surrounding hearing aids, Bankoski Chunyk said there used to be a stigma concerning eyeglasses.
“Years ago, glasses were a big deal; they used to call people ‘four-eyes,’” she recalled. “Now, people wear glasses as a fashion statement, and they have multiple pairs in different colors. It’s now cool to wear glasses.”
Hearing aids … not so much. And that picture is not likely to change anytime soon, although the technology continues to get smaller and even less noticeable than one’s hearing loss.
While she isn’t holding out hope that hearing aids can become a fashion statement, Bankoski Chunyk does have hope that more people will hear that message about hearing care equating to healthcare.
And not only hear it, but listen, and then act accordingly.
George O’Brien can be reached at [email protected]