‘I Love the Profession’

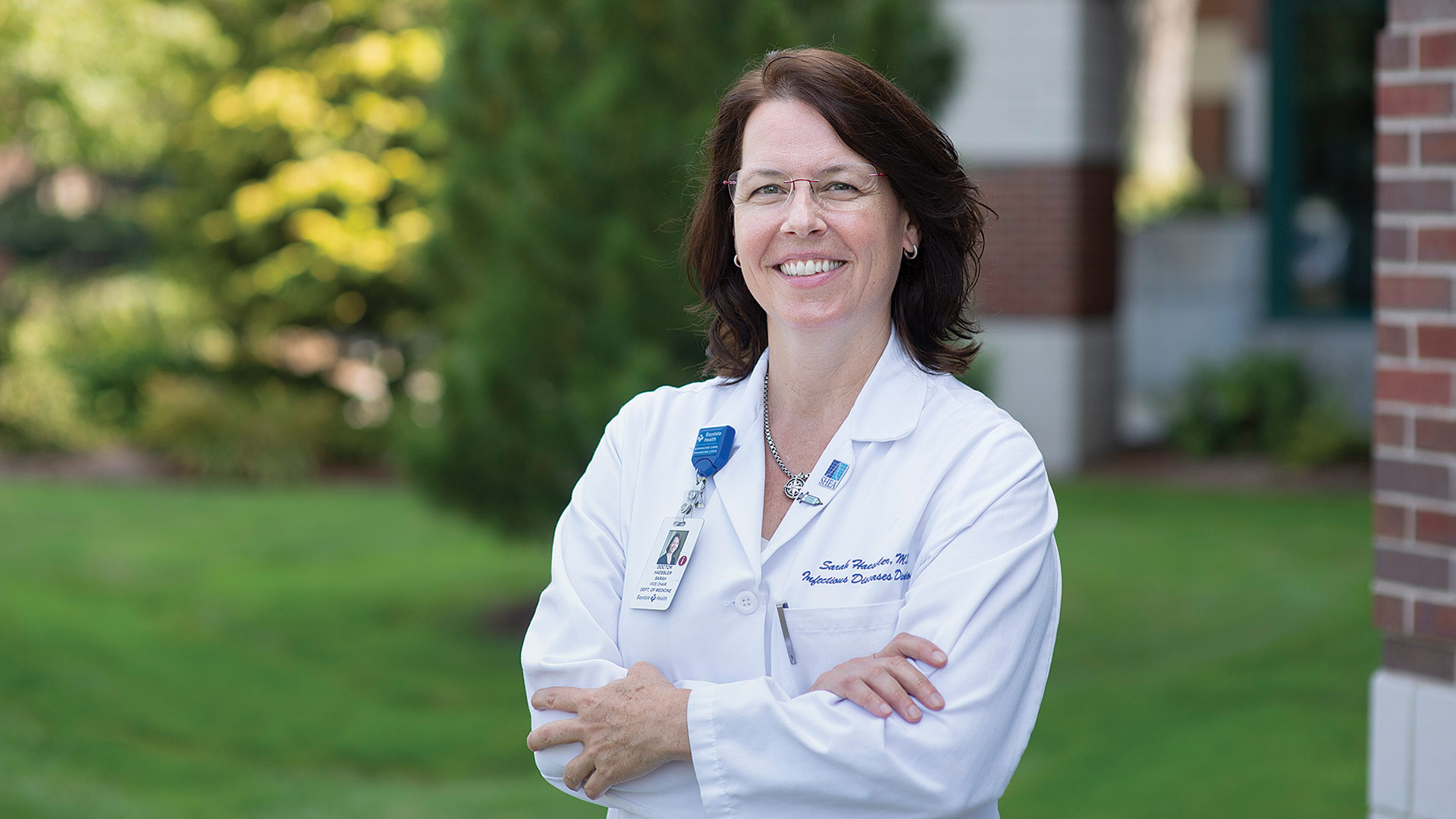
Ashley Girouard is gaining experience through Baystate’s SNAP program for new nurses.
To Ashley Girouard, seeing patients isn’t just treating them and sending them on their way. There’s a connection to be made in each encounter.
“I love making connections with my patients,” she said of her current work in an orthopedic unit at Baystate Medical Center. “A lot of these patients come in for routine hip and knee surgeries, and they’re healthy. And I love being able to talk to them. We’ll talk about sports, we’ll talk about their lives, their family, and I think it’s great. I love making those connections by talking to them.”
At Elms College, where she recently earned her bachelor of science in nursing degree and will soon add the title of registered nurse, Girouard followed in the footsteps of her mother, who made nursing her profession as well.
“I’ve always looked up to her. I see what she does day in and day out,” she said. “I know that I love caring for everybody around me, so I just decided to go into this profession … and I love it.”
Girouard currently works in the Student Nurse Associate Program (SNAP) at Baystate. SNAP nurses function in a supportive role to a registered nurse and work collaboratively with the healthcare team in the management of patient care. This position allows the student to gain experience in providing care to a diverse patient population and to develop strong communication and organizational skills.
Meanwhile, they perform direct patient care, obtain and record vital signs, collect laboratory specimens, document intake and output, communicate with patients and staff, promote patient safety, and function as a team member within the health system. Girouard appreciates the experience she’s getting through the program, not only in the specifics of orthopedics, but how to relate to patients. And she intends to keep learning, in a variety of settings.
“I want to get some med-surg experience, and I’ve always been interested in intensive care. And then I definitely want to go back to school,” she said, looking to move on to a master’s program. “My goal is to be a nurse practitioner.”
When asked why she strives for an ICU role, she said the “go, go, go” of the setting appeals to her. “These patients are very critical, and I’d like to be able to help them in any way possible, and just get them even a little better than they were in the morning.”
Taking classes and gaining learning experiences through the COVID-19 years was difficult, she admitted. “I’m a very hands-on visual learner, and having to learn from home in my room on a desk was not ideal at all.
“But we had amazing professors at Elms,” she added. “And they helped so much, all the time. They would have hourly extra time when you could go on Zoom with them, and if you needed help, they were always willing to help. I think the professors really made a difference. After all, they had to adjust to this big change as well.”
Even a period of mask wearing in class was a reminder that the pandemic wasn’t quite over, so being able to attend classes without masks this past year — and, more recently, work clinical rotations without them — have been pleasant reminders that life has returned to normal.
For health systems, of course, it’s still a very challenging time because of nurse shortages, as all the recent graduates we spoke with told us. And that means greater career opportunities for those entering the field, who are able to write their own tickets — with the right degrees of course.
“Even if there weren’t so many jobs out there, I still would be interested in nursing. I love the profession,” Girouard said. “But I think a lot of people want to go into nursing because they know they can go into deeper specialties like ICU or PICU, things like that.”
The work certainly requires certain traits, she said. “Definitely caring, for sure. And patience. If you don’t have patience, I don’t think this would be a good career choice for you; a lot of patients can be very difficult. And you need to be careful, too. A lot of errors can happen, and we learn in nursing school how important it is to prevent errors. It’s so easy to make a mistake.”
So, as Girouard ponders what might be next for her, both in the work setting and eyeing the next steps in her education, she’s walking into a world of opportunities as an RN with a healthy sense of caution and care, but not anxiety.
“I’m just so excited,” she said. “The last four years were so difficult, especially with COVID and working in the hospital during COVID. And now I get to go to work and not wear a mask. And I’m going to be a nurse, and actually take care of patients and be a difference maker.”
—Joseph Bednar






 The Emergency Department was rather quiet at Baystate Medical Center on Monday morning.
The Emergency Department was rather quiet at Baystate Medical Center on Monday morning.