Healthcare Heroes
Nurse Manager, VA Central Western Massachusetts Healthcare System
Her Work Caring for Veterans Is Grounded in a Sense of Mission

After a decade and a half in the nursing profession, Julie Lefer Quick was looking for a change, and found one at the Veterans Administration’s (VA) outpatient clinic in Springfield.
She also found a level of passion and mission-driven commitment she hadn’t experienced before.
“I can honestly say that I’ve never seen nurses more dedicated to their population; I feel the dedication,” she said. And so do the patients. “Last week, a nurse forwarded me an email that she received from one of her veterans’ caregivers about what great care she took of that veteran, just going above and beyond. And she said, ‘I love my job.’
“Every one of the nurses who works with the VA goes above and beyond every single day,” Lefer Quick added. “And it’s really wonderful to be a part of that, serving such a deserving population.”
She started at the VA in July 2018 as a primary-care nurse. Before that, she worked for a pediatrician in solo practice, including as practice manager, for two and a half years, followed by more than 11 years in the Springfield Public Schools.
“When my son went off to college, I thought, ‘now is a great time to try something new, get back into primary care.’ So that’s when I got the job at the VA.”
When they hear mention of the VA Central Western Massachusetts Healthcare System, most people think of the hospital in Leeds, which houses services ranging from inpatient psychiatric mental-health and substance-misuse treatment to primary care; from rehabilitation to specialties like orthopedics, radiology, cardiology, and many others.
“Every one of the nurses who works with the VA goes above and beyond every single day. And it’s really wonderful to be a part of that, serving such a deserving population.”
“And we also have five community-based outpatient clinics, where we primarily do primary care and then, depending on the clinic, some specialties to support the veterans,” she explained, noting that these are located in Springfield, Fitchburg, Greenfield, Pittsfield, and Worcester. “In Springfield, we have a very large mental-health department, and we also have a small lab, physical therapy, a registered dietitian, a clinical pharmacy, and what’s called home-based primary care.”
As it happens, Lefer Quick loves primary care, and missed that during her years working in the schools. “I had missed the ongoing, deep relationships with patients and their families.”
So, with her son graduating from the school system, she craved a return to care in a medical-office setting, and happened to meet some VA nurses at a Learn to Row event through the Pioneer Valley Riverfront Club in Springfield, where her husband, Ben Quick, is executive director.
“They were like, ‘oh you should come work at the VA,’” she recalled. So she did — and, not surprisingly, she loved the work. Which is why she was hesitant to take the position of nurse manager when it became available last October.
“I wasn’t really sure I wanted to be a nurse manager. I love taking care of my patients. I love working with my team in the VA,” she said. “Nationwide, we practice a primary-care delivery system called the PACT model, which stands for patient-aligned care team. So there’s one provider, one RN, one LPN, and one admin; it’s sort of like a mini-practice within a group practice.
“We always see the same patients, and I had a great team that I worked with,” she went on. “It’s a good model for the patients; they really love it. So I didn’t want to leave my team or my patients.”
But a mentor encouraged her to try something new, and she accepted the detail.
“As a PACT RN, I was providing direct patient care and education, working with my team to meet population health-management goals, such as certain levels of control for diabetes or hypertension. And now I work for the other PACT nurses, supporting them in their practice.”

The busy community-based outpatient clinic in Springfield is one of five operated by the VA in Western and Central Mass.
As nurse manager for two clinics — Springfield and Greenfield — she currently supervises 23 LPNs and RNs, with about three more to be hired soon. And she quickly found she could apply her passion for care in this overseeing role.
“In the VA, we have a unique understanding of the military culture that other providers in the community don’t necessarily have,” she said. “It’s a very sad truth that a lot of our veterans have emotional issues when they come back, but we are on the cutting edge of all types of mental-health treatment modalities and therapeutic options, and we also have the support of Congress — it’s a single-payer system, and we don’t have to be bogged down by some of the stuff that community providers have to deal with. So we, as nurses and providers, can really focus on our veterans and come up with innovative ways to care for them.”
A Passion for Patients
A quick look at the typically full parking lot at the VA’s Springfield CBOC, which stands for community-based outpatient clinic, testifies to the need for the services it provides, from laboratory and pharmacy to primary care and behavioral health.
“From what I have learned as the spouse of a VA nurse manager, it seems that, while most of these workers could get paid more elsewhere, they stay with the VA because they are passionate about caring for our veterans, and they are energetic about supporting each other in this difficult, important work,” Ben Quick wrote in nominating his wife for the Healthcare Hero recognition.
Yet, nursing wasn’t her first career. After graduating from college, she worked briefly in human resources, found she didn’t like that career, and went back to school for a nursing degree.
“Coming out of nursing school a little bit older than the typical students, I kind of took the first job that I could get,” she recalled. “I had a small child, so I didn’t want to work hospital hours, even though I loved the idea of being in the hospital, so I went to work for a pediatrician.”
Which surprised her, considering that her nursing-school rotations caring for youngsters tended to make her cry because she didn’t want to see them hurt or sick.
“I think there’s more of an awareness of mental-health needs in general in healthcare right now. And certainly, veterans who have seen combat are going to need support afterward. So that’s part of our mission.”
But as a pediatric nurse, “I loved seeing the kids grow over the years, seeing new babies born into families, working with parents on all kinds of different diagnoses to help their kids,” she recalled, and her next move was born of wanting to keep caring for children. “Working in the public schools was a way to be available for my son while also reaching a big population of kids. And I loved it.”
So Lefer Quick felt torn about leaving pediatric care for the VA.
“I remember leaving the public-school job for this, and I was very, very excited, but I had this moment of, ‘oh my gosh, am I doing the right thing?’ I said to one of my friends, ‘but I love my kids so much here.’ And she said, ‘you’ll find new patients in a while.’ And I did.”
In doing so, she’s taken to heart Abraham Lincoln’s famous quote that the VA — established 65 years after he uttered it — has adopted as a sort of mission: “to care for him who shall have borne the battle and for his widow, and his orphan.”
“One of the things that almost kept me from accepting the detail to nurse manager was all my patients,” she said, but she understands that all her roles have been supportive in some way: “supporting kids and their families, supporting students at school to be optimally healthy and ready to learn, supporting our veterans, and now supporting the nurses who provide that care to veterans.”
Some of that care is behavioral and substance-related. “We recognize the need for that integrated care for our veterans. I think there’s more of an awareness of mental-health needs in general in healthcare right now,” she noted. “And certainly, veterans who have seen combat are going to need support afterward. So that’s part of our mission.”
She said the VA has felt the strain of a nationwide nursing shortage as much as any other facility, but added that the nurses who take jobs there value the mission President Lincoln put forward — and many are veterans themselves, or come from a strong military family, or are drawn for some other reason to caring for a veteran population.
“That was how I talked myself into the manager position. I thought, ‘well, if I can be a manager with my background, already doing this job, I can support these nurses, which ultimately provides better care for the veterans.’ So I’m not just doing it for my team; I’m helping every single team.”
The COVID pandemic posed challenges across the spectrum of healthcare, but Lefer Quick said the VA was uncommonly prepared for it, as it had already implemented a remote monitoring platform called VA Video Connect, so VA facilities were able to pivot to virtual appointments more quickly than other organizations.
For instance, before the pandemic, “I had a patient who needed monthly monitoring for medication he was on, and he liked to travel. So we would do video visits, and we would have a set appointment to do the follow-up for his medication, wherever he was. So we already all knew how to use this,” she recalled.
And when COVID struck, “we very quickly pivoted to using video for several months, almost exclusively. A lot of our patients did not want to come to the clinic. Nobody wanted to go anywhere. And we already had this in place.”
Their concerns were warranted, as the pandemic hit the elderly population hard in the earliest days of the pandemic. “As you can imagine, a large percentage of the VA population is elderly. I had a father-son set of patients — and the son was 74. So a lot of them, being elderly and therefore immunocompromised, were scared, but the VA already had this amazing video platform, and we had already trained everybody how to use it.”
Meanwhile, “the nurses that I worked with were coming up with great ways to rotate the staff through the clinic so that we could spread out more to allow for that social distancing and masking in a more comfortable way,” Lefer Quick explained. “And we took on new providers and new nurses, even during the pandemic. We didn’t slow down much.”
Cutting-edge Care
In his nomination, Ben Quick boiled his pitch down to three thoughts: the VA’s quality of care is second to none, downtown Springfield has a busy medical practice devoted to healing America’s heroes, and the workers there are humble, passionate, professional patriots. “That’s a Healthcare Hero story that everyone needs to hear,” he wrote.
And now they will.
“The VA is the best employer I’ve ever had in my entire life,” Lefer Quick said. “They value creativity and innovation, and they support us to explore that.
“We really are on the cutting edge,” she added. “The people I work with are doing amazing things and love to be there. No matter where they are, in Springfield or any other part of this country, if someone is eligible for VA care, they really ought to look into it.” n
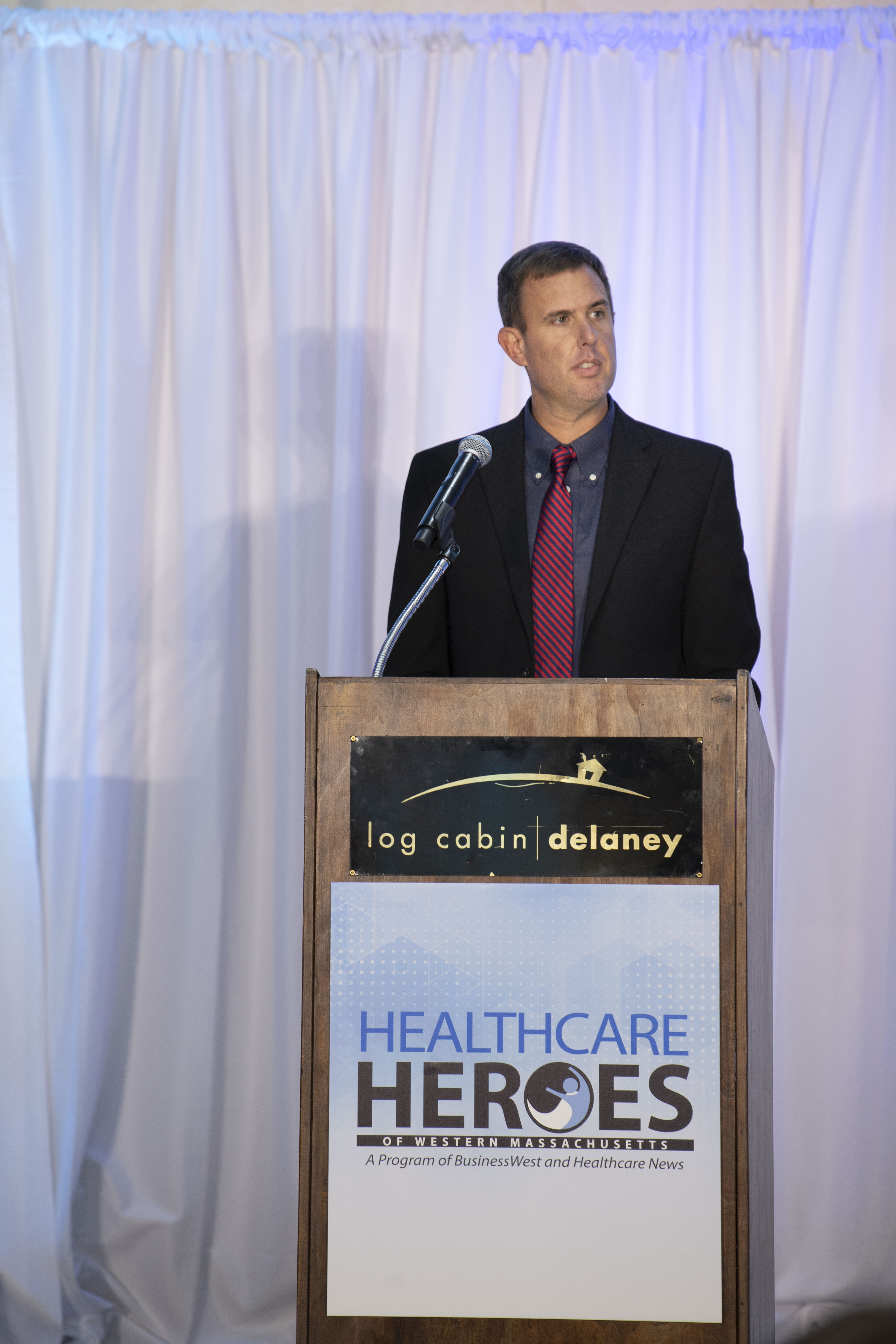
Patient Safety Associates, Holyoke Medical Center
Their Lifesaving Actions Shine a Light on a New Position at HMC
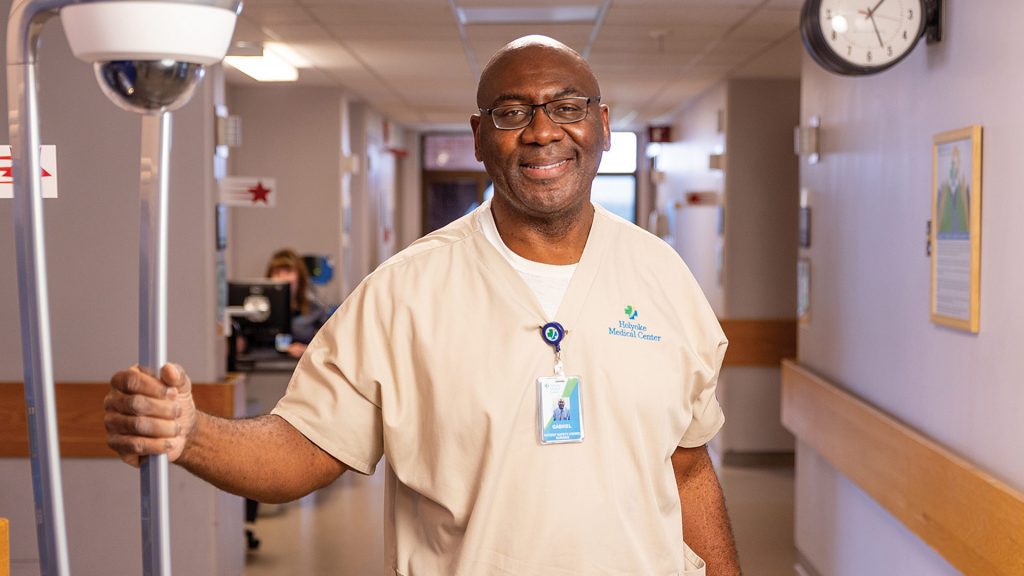
Gabriel Mokwuah

Joel Brito
When Gabe Mokwuah came to this country from Nigeria when he was 12 and heard people talking about ‘football,’ he thought about the sport played with a round ball that athletes try to kick into a net.
The other football, the one that is much more popular in this country? He didn’t know anything about it, and didn’t really want to know anything about it.
But that didn’t stop the football coach at his New York City high school from trying to convince the large, fast, and very athletic Mokwuah to try out for the team. Eventually, and we’re simplifying things here, he succeeded in those efforts. But even then, Mokwuah wasn’t really interested in the sport.
It wasn’t until he started hearing the word ‘scholarship’ and came to understand that football could be a means to an end — a college education and a ticket out of a high-crime area on Staten Island — that he began to really take it seriously.
Fast-forwarding through the next several years, Mokwuah did attend and graduate from American International College, while also playing defensive end and linebacker — so well, in fact, that he was drafted by the Green Bay Packers in the 11th round in 1992 (they only have seven rounds today).
He played in two exhibition games, was cut, tried to catch on with a few other teams, didn’t, and wound up working as a court officer at the Hampden County Jail and House of Correction, a job from which he retired several years ago.
All that adds up to just one of the intriguing backstories that can be told by those now working as patient safety associates (PSAs), or, in his case, patient safety coordinator, at Holyoke Medical Center (HMC).
Joel Brito has one of his own.
He was working for Hulmes Transportation, taking individuals to medical appointments and daily programs while also volunteering his time to help those with substance-abuse issues when he saw an ad posted on Indeed — Holyoke Medical Center was looking for patient safety associates.
“As soon as I saw it, I jumped on it, and here I am. This has always been my dream — I always wanted to be in the healthcare field,” he said, adding that his ambition is to become a certified nursing assistant.
Others now working as PSAs at HMC have backstories as well. Some are retired or semi-retired CNAs who succeeded in finding work that is rewarding on many levels. Others are getting started down the road to careers in healthcare and have taken this entry-level position to explore options and find out if healthcare is for them. Some are in pharmacy programs. One is studying for her MBA.
The PSA position is relatively new to HMC, and healthcare in general, and it represents an imaginative and innovative step forward from the ‘sitter’ or ‘patient observer’ role seen in most hospitals, said Margaret-Ann Azzaro, vice president of Patient Care Services and chief Nursing officer at HMC.
“As soon as I saw it, I jumped on it, and here I am. This has always been my dream — I always wanted to be in the healthcare field.”
Elaborating, she said the role involves not merely sitting with an at-risk patient, but engaging with them as a well, a position that brings more value to the patients and the hospital, but also those who assume that role.
“We thought, ‘let’s come up with a safety role to empower people to not only keep these patients safe, but engage with them as well,” she said. “We don’t have sitters here; we don’t have observers here — we have patient safety associates, and the idea is to give them some education and tools to enrich the experience while they’re sitting with a patient.”
Mokwuah and Brito embody the motivations behind the PSA position and also just how vital these individuals are — to a hospital, to the patients they serve, to initiatives to reduce falls and improve overall patient safety, and, sometimes, much more.
Indeed, both have been credited with saving lives in recent months — Mokwuah in April, by seeing something while in the virtual monitoring room and immediately calling for a team member to check on the patient, and Brito in July for performing the Heimlich maneuver on a patient he heard making sounds of distress while he was sitting with another patient. (More on both episodes later).
Both men were named employee of the month for their respective actions. That’s certainly an honor, and in October, they’ll be receiving another one: Healthcare Hero.
Not on Their Watch
There are actually three distinct roles within the PSA position, and individuals with that title handle all three on a rotating basis, noted Brian Toia, Nursing director of the ICU, RN float pool, and patient safety associates, adding that teamwork is what makes this innovative program so effective.
The first role involves one-on-one direct care — staying within arm’s length of a patient with a high safety risk, including those susceptible to falls, patients with dementia, and those who might be suicide risks. The second involves virtual monitoring. Utilizing a camera system placed in rooms of patients with potential safety risks, PSAs working in the virtual monitoring room can keep tabs on up to 12 patients at once.

From left, Margaret-Ann Azzaro, Joel Brito, Gabe Mokwuah, and Brian Toia.
The third role is what those at HMC call a ‘rounder,’ one person dedicated to a unit who will frequently check on patients, respond to virtual monitoring calls, and also answer patient calls for assistance.
When asked which role he liked the most, Brito didn’t hesitate. “I like being a rounder. I love that it’s a non-stop job.”
But all these roles are vital to the overall mission of keeping at-risk patients safe, said Mokwuah, who coordinates the department and makes the daily assignments.
Before he talked about the PSAs and what they do, he put matters in their proper perspective. “The real heroes are the nurses, the doctors, and the administrators. And they have given us support for this program to take off. Our job is to keep people safe, and our program saves lives — we’ve proven that over and over again.”
“We thought, ‘let’s come up with a safety role to empower people to not only keep these patients safe, but engage with them as well.’”
Azzaro agreed, emphasizing, again, that PSAs are far more than the ‘sitters’ of years ago. These are individuals who can, and do, watch over patients. But they also engage them and help “enrich the experience,” as she put it, while offering some examples.
“We gave them dementia and Alzheimer’s education,” she explained, noting that this, like other aspects of the program, is fairly unique within the industry. “There are certain ways in which we can engage with patients that have dementia, that have Alzheimer’s. One thing that doesn’t help them is to not be stimulated. So the PSAs can read to them, they can play games with them, they can have conversations with them, they can read a book to them, they can put something on the TV or iPad and have the patient watch it with them.”
And while engaging with these patients, or watching them on the monitor, or coming to their assistance as a rounder, the PSAs are ultimately keeping them safe, said Azzaro, noting that there has been a measurable decrease in the number of falls recorded at HMC since the start of the program.
Changing Lives, Saving Lives
As he talked with BusinessWest outside the monitoring room, Mokwuah said the facility boasts a split screen showing more than a half-dozen patients in their beds. At this moment in time, all was quiet and normal.
That was not the case one afternoon back in April, when, while watching that same monitor, he noticed a patient that did not appear well, was acting differently, and had a noticeable status change.
He called for a rounder to immediately check on the patient, who, as it turned out, was experiencing a significant medical event, was unresponsive, and had no pulse. Staff quickly began performing basic life support, followed by advanced cardiovascular life support. After two rounds of CPR and cardiac medications, the patient’s own breathing and heartbeat returned.

Joel Brito (left) and Gabe Mokwuah have both been credited with saving patients’ lives in recent months.
Staff Photo
Joel Rivas, director of Nursing Medical-Telemetry, who nominated Mokwuah for employee of the month, said at the time, “it is my professional opinion that, had the patient’s change in condition not been identified as early as it was, by Gabriel, we would not have had the positive outcome that we had.”
Similar things were said after another incident in early July, when Brito again showed the importance of HMC’s innovative PSA program.
He was serving as a rounder and sitting with a patient when another team member came in to provide patient care. During that time, Brito overheard a patient from another room making sounds of distress. Confirming that his one-on-one patient was safe and in the care of another team member, he stepped into the next room to check on what he’d heard.
“In the beginning, I didn’t pay too much attention to it, but something told me to get up and check that room, and when I did, I was really surprised because the lady was essentially purple,” he said, adding that he quickly positioned himself to perform the Heimlich maneuver and helped to dislodge the obstruction in the patient’s airway.
“This is a job where you have to be humble, you need to have some empathy, and you have to love people. That’s something my mom and my family instilled in me growing up, so I try to live my life that way and help people. This job gives me the opportunity to do that.”
Like Mokwuah, Brito was credited with saving a patient’s life, said Toia, adding that, had it not been for establishment of the rounder’s role within the PSA program, it’s unlikely that someone would have been able to respond as quickly to the situation as he did.
Looking back, Brito said he relied on his instincts and his training, and was thankful to be in a position where he could help people and make a difference in their lives — the most gratifying aspects of the PSA position.
Mokwuah said essentially the same thing.
“This is a job where you have to be humble, you need to have some empathy, and you have to love people,” he said. “That’s something my mom and my family instilled in me growing up, so I try to live my life that way and help people. This job gives me the opportunity to do that.”
Big-game Players
Gabe Mokwuah didn’t get to be a hero on the gridiron, at least at the pro level. But his life and career, especially this latest chapter, show that our heroes come from all walks of life. And they take all kinds of titles.
Patient safety associate is a relatively new one at Holyoke Medical Center, an innovative initiative that is helping to prevent falls, improve overall safety, and, as these cases show, save lives.
Mokwuah was right when he said that doctors, nurses, and administrators are heroes. But so are those with badges that read ‘patient safety associate,’ especially these two lifesavers and Healthcare Heroes.
Clinical Psychologist; Assistant Professor of Graduate Psychology, Bay Path University
She Impacts Lives — and the Next Generation of Mental-health Professionals — for the Better

It’s not easy to cover everything Kristina Hallett has done in her wide-ranging career in one story. At least, not cover it in a way that fully conveys her impact.
Her past titles convey some of it. Director of Brightside Counseling Associates and then director of Children’s Services at Providence Behavioral Health Hospital, both in Holyoke. Supervising psychologist at Osborn Correctional Institute in Somers, Conn. Director of Psychology Internship Training at River Valley Services in Middletown, Conn. And currently, associate professor in Graduate Psycholology and director of Clinical Training at Bay Path University.
Oh, and she’s maintained a private psychotherapy practice in Suffield, Conn. for the past quarter-century.
There are some common threads.
“Dr. Hallett’s career spans over 25 years, during which she provided invaluable psychotherapy, consultation, and supervision to medical and mental-health professionals, addressing myriad relationship and major life issues. Her expertise in complex trauma and dissociative disorders is instrumental in supporting and empowering those facing significant psychological challenges,” wrote Crystal Neuhauser, vice president of Institutional Advancement at Bay Path, one of three people who nominated Hallett as a Healthcare Hero.
Just as importantly, “she is a guiding influence in shaping the next generation of mental-health practitioners. Her commitment to education and mentorship showcases her passion for instilling excellence, compassion, and cultural competence in students. She is especially passionate about guiding under-represented caregivers into the profession to help underserved communities see themselves in their mental-health professionals.”
That’s a mouthful, but it’s important to understand the generational impact of Hallett’s work — not only helping people move through often-severe challenges and trauma toward a happier, healthier, more fulfilling life (which she accomplishes as a teacher, therapist, executive coach, author, speaker, podcaster, and more), but she’s helping to raise up the next wave of mental-health professionals to do the same, at a time when the needs are great.
“When we’re talking about mental health, it’s about connection, and there are different ways to make a connection. And having a role model who look like you and who understands you is really important.”
“I’m just ecstatic about our program,” she said of her role at Bay Path, where she started teaching in 2015. “When I came, we had maybe 50 students. Right now, in our program, we have 280-plus students. This summer, they did a 100-hour practicum with us before their 600-hour internship out in the community. We had 62 students in practicum this summer, which is a logistical challenge, but we’re really able to help shape them, educate them, and give tools and resources to the next generation.”

Kristina Hallett’s books have delved into topics ranging from relationships to banishing burnout.
Staff Photo
Meanwhile, Hallett’s bestselling books, Own Best Friend: Eight Steps to a Life of Purpose, Passion, and Ease and Be Awesome! Banish Burnout: Create Motivation from the Inside Out, inspire personal growth and empowerment, while a co-authored workbook titled Trauma Treatment Toolbox for Teens is a resource for young people facing trauma-related challenges, and her contribution as a co-author to Millennials’ Guide to Relationships: Happy and Healthy Relationships are Not a Myth! reflects her commitment to enhancing the lives of diverse populations.
As an executive coach, she helps participants find lasting change in the areas of burnout, stress, motivation, and self-confidence. And her podcast, “Be Awesome: Celebrating Mental Health and Wellness,” provides hope and guidance to listeners, fostering an environment where seeking help and prioritizing mental health is normalized.
As noted, it’s a lot to take in, but Hallett is energized by the opportunity to impact so many lives in so many different ways. The opportunity, in fact, to be a Healthcare Hero.
Connected to Kids
Hallett’s private practice offers individual and family treatment, with some intriguing specialty areas, including psychotherapy for medical and mental-health professionals, military personnel, and first responders; substance abuse; mood disorders; LGBTQ clients; trauma recovery; and treatment of complex trauma and dissociative disorders.
It’s a far cry from her earliest goal in life, which was to be a pediatrician.
At Wellesley College, where she was a biology major in a pre-med program, she took a psychology course “for fun” — and found the topic interesting, so she added a double major in psychology. “My professors were like, ‘oh, you should go into psychology.’ And I said, ‘no, no, no, I’m going to be a pediatrician … right?’”
During her senior year, as she took her medical college admissions tests, Hallett found herself in an interview, being asked, ‘why do you want to go to medical school?’ And something clicked.
“I had this experience where my mouth kept talking, but a part of my brain said, ‘yeah, why do you want to go to medical school?’”
Her answer was to enroll at UMass Amherst — in a graduate psychology program.
That’s not to say she wouldn’t work with children, adolescents, and families, though. At her earliest career stops, she had plenty of opportunities for that, from her stint as regional program supervisor for the Key Program in Springfield from 1991 to 1995 to her roles with Brightside Counseling Associates from 1996 to 1998 and Providence Behavioral Health Hospital from 1998 to 2003.
“I loved the idea of working with adolescents because, while I was young, still in my 20s, I felt like they’re ripe for change; you can be honest with them … it’s a very real interaction, while adults are just stuck in their ways,” she said, adding quickly, “I don’t think that way anymore.”
That’s because she’s had plenty of experience working with clients of all ages. In fact, her next stops — at Osborn Correctional Institution from 2003 to 2005 and River Valley Services from 2005 to 2015 — broadened her experience dramatically.
Kristina Hallett’s office in Suffield, Conn. is filled with photos, artwork, and mementos from her interactions with patients.
Staff Photo
“So the first half of my career was children and adolescents, but really centered on adolescents,” she said. “And it’s unusual for someone to be running an outpatient mental-health clinic and running inpatient children’s services, and then working in a prison.” At the time, she added, Osborn housed 2,000 male inmates and also arranged schedules for mental-health workers for some other local prisons.
Years later, while working at River Valley, Hallett had a yen to get into teaching, so she joined Bay Path as an adjunct professor in 2015, which quickly led to part-time work and then a full-time opportunity. It sure beat the commute from Suffield to Middletown, but there were other, more important reasons to make the jump.
“Bay Path had just started its clinical mental-health counseling program, and they were going to expand. And I thought, ‘yeah, I’m ready to do this full-time.’”
Her first title was coordinator of clinical training, which became director of clinical training. And this past spring, when the program director left, she took over that role.
“I’ve been responsible for bringing in a lot of faculty over the last few years, and this summer alone, I brought in four faculty who are former graduates of our program, all coming from different perspectives,” she told BusinessWest. “I like to bring back our graduates because they know the program, and we want to support them in their career. I’m trying to create a pathway for our students, post-graduation, to continue their own growth and learning.”
A couple years ago, Hallett’s department procured a behavioral-health workforce and education training grant through the Health Resources and Services Administration, to support and build up the young mental-health workforce, but also to better integrate these professionals into medical settings.
“So, you have a medical office with physicians, and then you have an embedded clinician,” she explained. “You come in for your annual physical, maybe you’ve been feeling a little down, and your physician says, ‘oh, you know what, I’ve got Stacy here who can maybe talk to you about that.’ And Stacy talks to you and sees if there are resources available to help you — therapy or whatever. So that’s a newer model that’s beginning to happen, which is great.
“It’s always about increasing access, because there’s a huge mental-health crisis, a huge need, a huge waiting list,” Hallett went on. “So anything to increase the workforce is great.”
In 2023, the third year of the four-year grant, Bay Path was able to fund 36 students to the tune of $10,000 each. “So 36 students are working full-time, many have families, and they’re still trying to get a master’s degree and go into the field. As you can imagine, it’s really hard to do all that and then work 600 hours as a clinician. So the $10,000 is phenomenal.”
She recently applied for another grant, with a bigger stipend, for students going through their internships and want to work in community-based clinics, either with services from the Department of Mental Health or a majority MassHealth clientele. “So the people who need the services are going to get good services,” she said, while, again, cultivating the next generation of professionals. “I am so excited about it.”
Heart of a Teacher
It was Hallett’s love for educating people, in fact, that led her to finding other ways to communicate.
“I love what I do one-to-one, and I love teaching. So what other ways do I have to make an impact with things that people really need to know?” she said. “The podcast and the books and the speaking are just ways to share messages and really say, ‘there are things that we can do to help ourselves, to feel a sense of agency, even when the world is sort of going crazy around us, and when there are really difficult challenges that we don’t necessarily have any control over.”
So much of her work, she said, has been with community-based organizations because she cares about access to mental health, especially for the underprivileged and underserviced. “I want to support and encourage an increase in a truly diverse workforce because that’s who we are. People need to see people like themselves. It’s not that they can never talk to people with differences; of course they can. But when we’re talking about mental health, it’s about connection, and there are different ways to make a connection. And having a role model who look like you and who understands you is really important.”
As for her decades of work with stress and trauma, in particular her work with clients from the military and first-responder communities, it started early on, working with adolescents in difficult situations.
“There are horrific things that humans do to each other that are certainly hard to live through,” she said. “They’re hard to hear about, and they’re hard to know. So I try to counteract that darkness with some kind of support. People who have gone through really horrible things deserve someone to stand in the witness of that.”
For a while, in the pre-COVID years, Hallett said, she was primarily working with medical and mental-health professionals in her practice. “These are small communities; it’s hard to find providers who work with providers. So that just sort of evolved. I had already started working with veterans and first responders, and then COVID hit, and that was a time when there was so much need.”
She no longer works with teens, and the goal for her adult clients is to get them back out living their lives and doing the work that’s meaningful to them. “But if something comes up at another point in time where something new has happened, you can come back. We create a relationship that allows you to come and go. I’m always working to create these longer-term relationships.”
And, not surprisingly, she has applied that passion to her other career at Bay Path, helping to create an advanced trauma certificate in her department.
“As practitioners in the field, we’re always asking, ‘what’s the latest? What’s backed by science? What do people need to know? What do we wish we knew when we were in school? And how do we continuously support the growth of the next generation?’” she said. “Because we need them.” n
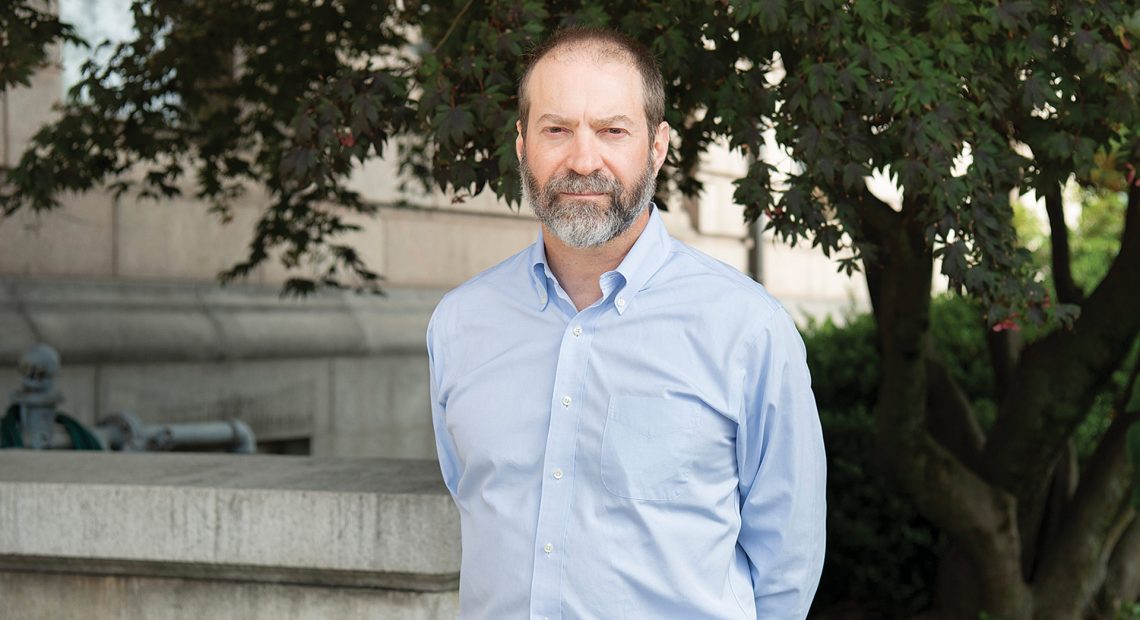
Chief of Emergency Medicine, Mercy Medical Center
He Considers Listening His Strongest, Most Important Talent

As a general rule, physicians working in the emergency room don’t get to know their patients as well as those in primary care or other specialties, who see their patients regularly and over the course of years and, sometimes, decades.
But Dr. Mark Kenton makes it a point to get to know those who come to his ER, the one at Mercy Medical Center. Indeed, he said he always looks to make a connection by listening to each patient and learning about what they are interested in and passionate about.
In addition to making these connections, he tries to get involved and make a difference, in ways that go beyond providing medical care.
“Sometimes, the best medicine you give someone is not actually medication,” he told BusinessWest. “It’s just listening. Everyone has a story.”
He was listening as one patient, a veteran named Homer who was going into hospice care, expressed regrets about never making it to the World War II Memorial in Washington, D.C. So Kenton researched the Honor Flights program and worked with the patient’s family to help make arrangements for him to visit the stirring memorial. Later, he received a letter from that family.
“They said he died two weeks before he was scheduled to go, but he died knowing that he was going, and it meant a lot to him,” Kenton recalled. “That stuck with me.”
He was also listening to another patient who was near the end of his battle with cancer and came to understand that the two shared a love of baseball and the Red Sox. Kenton arranged a phone call to the patient from former catcher Rich Gedman, whom Kenton had come to know well from his participation in Red Sox fantasy camps.
“Sometimes, the best medicine you give someone is not actually medication. It’s just listening. Everyone has a story.”
“He said, ‘I can’t believe Rich Gedman actually called me,’” Kenton recalled, adding that the conversation had a lasting impact.
This ability to listen, and act on what he hears, is one of many traits that has made Kenton a Healthcare Hero for 2023 in the Healthcare Administration category — annually one of the most competitive categories within the program.
He stood out amid a number of others nominated for the award for his ability to act upon what’s heard — in a variety of different settings — and generate needed dialogue, which has sometimes led to real change.
This includes the ER at Mercy, where he has worked with others to improve flow, shorten wait times, and reduce the number of patients who leave the ER without being seen, battles that have become even more difficult amid critical shortages of trained professionals, especially nurses.
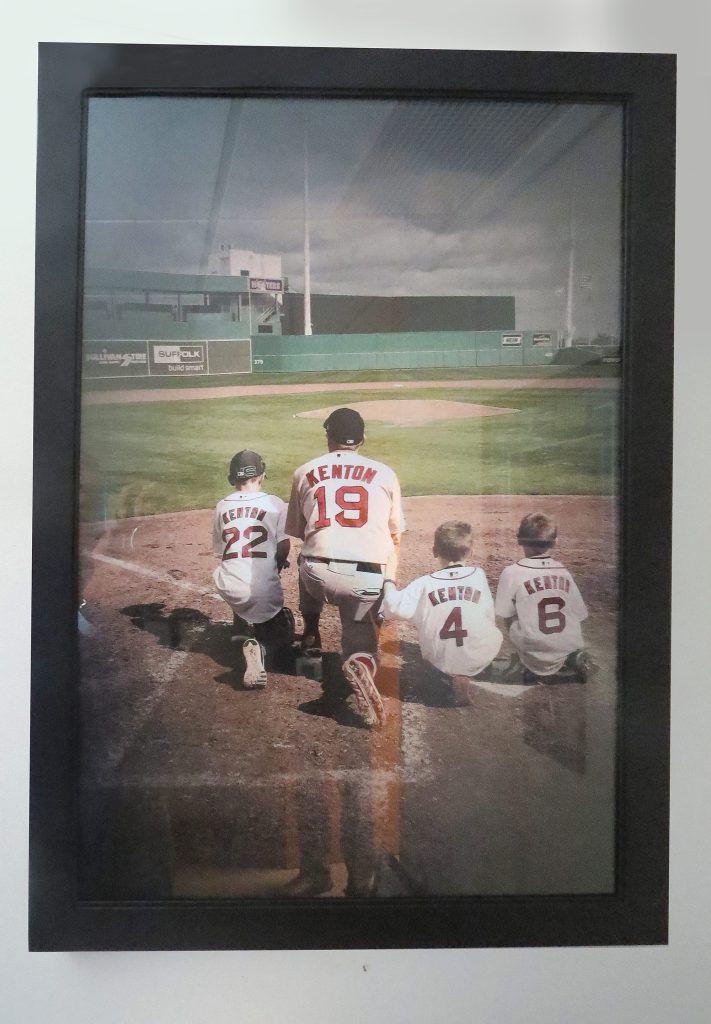
One of Dr. Mark Kenton’s passions is baseball and Red Sox fantasy camps, something that has become a family affair, as in this scene at Jet Blue Park in Florida with his sons (from left) Mark, Davin, and Jacob.
But it also includes the national medical stage, as we’ll see. Indeed, a letter posted on Facebook from Kenton to the CEO of Mylan juxtaposed the CEO’s salary against the sky-high cost of EpiPens and thrust the debate about the rising cost of pharmaceuticals into the national spotlight.
In Massachusetts, Kenton played a strong role in the passage of a bill that would allow EpiPens to be purchased in the same manner as Narcan for municipalities, whereby the state would purchase them at something approaching cost.
Kenton has also advocated for increased protection from workplace violence in hospitals, testifying at the State House after a colleague at Harrington Hospital suffered a near-fatal stabbing. Those efforts have been less successful in generating change — a result he blames on the high cost of measures such as metal detectors — but he continues to push for legislation that might prevent such incidents.
For his ability to listen and effect change — in his ER and many other settings as well — Kenton is certainly worthy to be called a Healthcare Hero.
A Great Run
The art hanging on the walls of Kenton’s office certainly helps tell his story.
Most of the pictures are baseball-themed — he played in college, has attended the Hall of Fame induction ceremonies in Cooperstown since 1981, and has more than 7,000 baseball autographs, by his estimate — including photos from the fantasy camps he’s attended, with his children prominent in many of them.
“I’ve been going for 13 years now, and it’s been a pretty amazing experience,” he said, noting that he’s been on the same field as many Red Sox legends. “Now, it’s more about going back and playing with friends than seeing the Red Sox — but they’ve become friends, too.”
But there’s also a framed photo of the cast members of The Office, a gift from his children. He is a huge fan of the show, and notes with a large dose of pride that he’s met several of the cast members and possesses a suit jacket that Steve Carell wore on the show.
While Kenton spends a good amount of time in this space, his true office, if you will, has always been the ER, and especially the one at Mercy. He arrived there in 2003 and became chief of Emergency Medicine in late 2019, three months before COVID hit and turned the healthcare system, and especially the ER, on its ear.
The trajectory for this career course was set over time, and Kenton believes his passion for helping others began when he watched medical dramas on television with his mother and became captivated with what he saw.
“My mother had cancer as a child; she spent a lot of time in hospitals and always had a fascination with healthcare,” he recalled. “She was always reading medical books, and we watched every show you can think of — Quincy; Trapper John, M.D.; St. Elsewhere; you name it.”
Because of his love for baseball, Kenton initially considered a career as an athletic trainer, since he could combine both his passions, baseball and healthcare, and he attended Springfield College with that goal in mind.
He quickly realized that the life of an athletic trainer did not have a lot of stability. And after working as an EMT, a rewarding but also harrowing experience — “I remember going to shootings and the shooter was still on the loose” — he decided the emergency room was where he wanted to spend his career. He earned his medical degree at Lake Erie College of Osteopathic Medicine, with the goal of completing his residency in Baystate Medical Center’s ER, a path that became reality.
“I hand out my business card to patients, talk to them, and ask, ‘why are you here today?’ I do that as one more check to make we’re not missing something.”
As he talked about working in the ER, Kenton related what he told his students when he served as medical director of the Physician Assistant Program at Springfield College. “I would always say, ‘be a little scared every day when you walk in — never lose that. Have a little fear when you walk in, because you don’t know everything, nor should you know everything. You need to know what your resources are and how to utilize those resources. You also need to know that you’re going to be tested — every day.’”
Safe at Home
These days, most of Kenton’s work is administrative in nature — he does one clinical shift per week — and, summing it up, he said it’s about making this ER as safe, welcoming, efficient, and effective as he can.
It needs to be all of the above because the ER is the “front door to the hospital,” as he put it, and a safety net for many within the community.
“There are so many patients that don’t have primary-care doctors now or don’t have insurance,” he said. “The ER is what they turn to.”
As he works with his team to improve flow, reduce wait times, and improve the ‘leave without being seen’ numbers, Kenton relies on what might be the strongest of his many skills — listening. In fact, he’s in the waiting room every ‘admin’ day talking with not only patients, but their families as well.
“I hand out my business card to patients, talk to them, and ask, ‘why are you here today?’” he said. “I do that as one more check to make we’re not missing something. I tell them that we’re working hard to get people through the system, and we’ll work on getting you through as soon as we can. And then, I listen.”
This brings him back to his comments about how everyone has a story, and it’s important to know and understand that story.
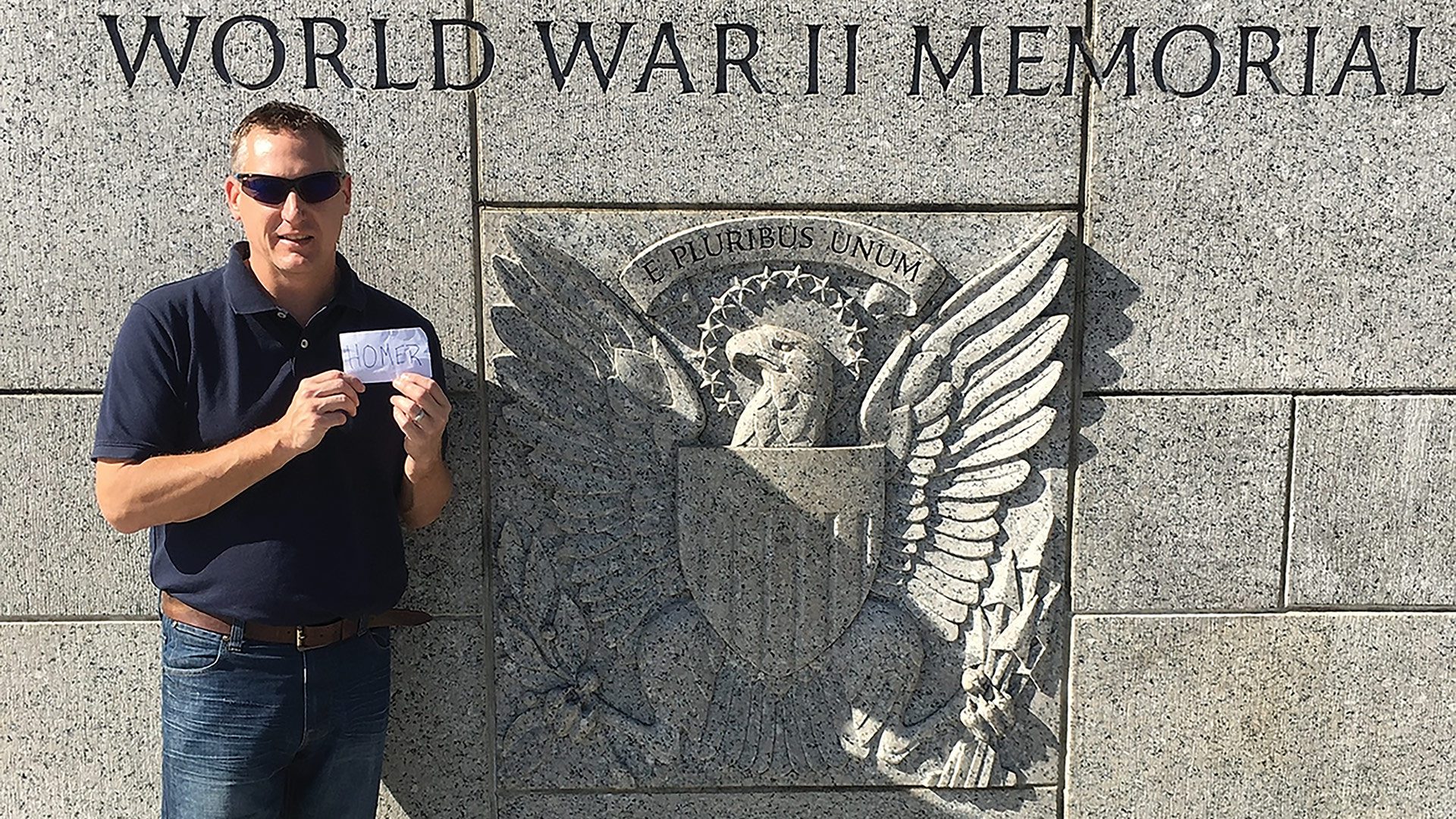
Dr. Mark Kenton holds up a card with the name ‘Homer’ on it at the World War II memorial in Washington, fulfilling, in a way, a dying patient’s desire to visit the memorial.
“You can look at the medical problem, but if you look at them as just a patient, you kind of forget that behind that patient is a person who’s scared, a family that’s scared,” he said. “Some people have lived incredible lives and been very fortunate, and some people have not had very good luck, or they’ve made bad choices, or they haven’t had the opportunities that others have had.
“I’ve taken care of Tuskegee Airmen; I took care of a gentleman who told me he flew on the Enola Gay,” he went on, referencing the famed African-American fighter and bomber pilots who fought in World War II and the B-29 that dropped the atomic bomb on Hiroshima. “You learn from those stories.”
While listening, learning, taking care of patients and their families, and improving efficiency in the ER, Kenton has also become an advocate for needed change in healthcare. His open letter to the CEO of Mylan on Facebook was spurred by incidents in his personal and professional life.
Indeed, while on vacation with his family, his son had an allergic reaction to peanuts. He soon learned that a prescription for two EpiPens, the best treatment for anaphylaxis, would cost $600. Fortunately, that prescription was transferred to a pharmacy that would accept his insurance, bringing the cost down to $15.
But he understood that such good fortune would elude others. While working a shift in Mercy’s ED a few months later, he saw two patients suffering from anaphylactic reactions and gave them both EpiPens, knowing they wouldn’t be able to fill the prescriptions going forward because they didn’t have insurance.
His frustration with this matter prompted his letter, which garnered press across the country and a live interview on Fox Business. More importantly, it generated real change, especially in the Bay State. Kenton testified before the state Senate on a bill introduced by former Sen. Eric Lesser to make EpiPens available for purchase by the state, just like Narcan.
Stepping Outside the Box
Two years after Kenton received that letter from the family of that veteran who died before he could get to the World War II memorial, his wife was running in a marathon in D.C., and he made the trip with her.
He wrote Homer’s name on a piece of paper, took pictures of it in various spots at the memorial, and sent them to his family.
“I said, ‘your dad finally made it,’” he told BusinessWest. “From what he told me during that relationship we established in a really short period of time, that brought closure to me, that he made it there.
“There are things you can do beyond providing medication to someone — sometimes you just have to step outside the box a little bit,” he went on, using a baseball term to get his point across.
This ability to forge those relationships, listen to each patient’s and each family’s story, and go well beyond simply providing medication helps explain why Kenton stands out — in his field, in his ER, and in his community. And why he is being recognized as a Healthcare Hero. n
Pediatric Emergency Nurse, Baystate Medical Center
Her Passion for Behavioral Health Has Enhanced Care Across an Entire ER

Ellen Ingraham-Shaw just couldn’t get away from children — even when she thought she wanted to.
And thanks to her leadership and innovative thinking, a lot of kids are better for it today.
“I actually started my career as a kindergarten teacher,” she said, before jumping back in time a little to when her interest in working with children really began.
“Growing up, I was a horseback rider, and I got into teaching younger kids how to horseback ride; that’s how I started working with children and adolescents, including working summer camps when I was in college,” she recalled.
Then she studied early childhood education and psychology at Mount Holyoke College before spending the first five years of her career as a kindergarten teacher.
There, Ingraham-Shaw saw needs that can’t always be addressed in the classroom.
“I worked in Chicopee, and in my classroom, I had a lot of homeless students,” she said. “So I started getting really interested in the socioeconomic status of kids and all the barriers that can really get in the way of how kids learn.
“I was happy, but I didn’t see myself doing it forever,” she continued, “so I went back to school for a second bachelor’s in nursing at UMass Amherst. After that program, I started working at Baystate Medical Center on one of the adult floors. And I just thought I didn’t want to work with kids anymore after feeling kind of burnt out.”
“Especially during the pandemic, the behavioral-health population just kind exploded in our ER. And I just got really passionate about it.”
So when friends asked her whether she wanted to enter pediatrics, she said no — but that feeling eventually thawed, and she applied for a position in Baystate’s pediatric ER. And she fell in love with it, calling it a well-run unit that, she realized early on, had an openness to new ideas and a focus on behavioral health that she would eventually expand in a number of ways.
“Especially during the pandemic, the behavioral-health population just kind exploded in our ER. And I just got really passionate about it,” she said. “And I’m lucky that my managers and my educators on my unit really support us working toward the things we’re interested in. If you want to seek out opportunities to do your own education, they give you opportunity to research.”
Thus began a fruitful career in pediatric emergency care with a focus creating more education and resources around behavioral health.
“I’ve been able to do education on de-escalating patients, just helping with the safety of the staff and the patients. And I think our physical restraint numbers have decreased; we have seen a decrease in having to resort to a restrictive environment with the kids.”
Ingraham-Shaw also worked closely with Pediatric ER Manager Jenn Do Carmo on Narcan take-home kits for the Pediatric Emergency Department. They were talking one day about how Baystate’s adult ED provides take-home kits to their substance-misuse population, but the Pediatric ED had no such process. So they decided to change that. Ingraham-Shaw created an education flier for nurses and doctors, made sure the kits were stocked, and educated every nurse on how to educate patients and families in their use.
“I did some education with our staff on how to identify patients that might be at higher risk,” she explained. “These are patients who come in with an overdose or, unfortunately, we’re seeing a lot of adolescents these days with suicide attempts and self-harm; sometimes they could be opioid-related, sometimes not. But if someone has a past overdose attempt, they’re at a higher risk of potentially overdosing on opioids in the future.

Ellen Ingraham-Shaw says pediatric emergency nurses bring not only care, but large doses of compassion and education to parents.
“So we’re making sure we have Narcan out in the community,” she added. “The nursing job is to help identify the patients that could be at risk, then working with the providers to make sure Narcan gets prescribed.”
Do Carmo, who nominated Ingraham-Shaw, said this program has the potential to save the lives of pediatric patients who overdose on opioids in the community. “Ellen is also going into the community and teaching local schools about the process of administering Narcan,” she wrote. “Ellen is a strong advocate for her patients and is a Healthcare Hero.”
Knowledge Is Power
As another example of thinking — and leading — outside the box, Do Carmo noted that Ingraham-Shaw noticed a gap in education on the care of LGBTQ and transgender patients, and took it upon herself to create educational materials and a PowerPoint presentation on how to care for and support these individuals.
“The entire Emergency Department now provides her representation on transgender education in nursing orientation,” Do Carmo wrote. “This presentation provides a clear understanding of a population in dire need of support and words and ways that help support the care of this population.”
Ingraham-Shaw told BusinessWest that she developed that education on LGBTQ and transgender health for a staff meeting, and the educators in the ED now utilize it as a required part of onboarding training for all emergency-medicine staff at Baystate, not just in the Pediatric ED. “So all of our staff has some level of training in how to be respectful and understanding of patients in our community.”
That aspect of education can be lacking in the training and college programs medical professionals experience entering their careers, she added. “So I think our people are definitely able to support those patients a lot better.”
Providing care that’s not sensitive to that population typically isn’t a problem of malice, but ignorance, she was quick to add. “It’s just people not knowing. And now my unit especially has at least a little baseline of how to be more respectful and understanding of patients.”
Of course, sensitivity to what patients are experiencing comes naturally in a pediatric ER, where the days can be challenging and the situations dire.
“I did some education with our staff on how to identify patients that might be at higher risk. These are patients who come in with an overdose or, unfortunately, we’re seeing a lot of adolescents these days with suicide attempts and self-harm; sometimes they could be opioid-related, sometimes not.”
“One thing I do like about it is that every day is completely different. I think it’s gotten a little bit harder now that I just had my own baby; I’m still adjusting to that,” she said of the toughest cases. “But the majority of what we see is more urgent care, or things likely to be seen in a primary-care setting. Those usually have a happy ending — you help educate the family, you make sure the child is safe, is eating, drinking, breathing, and then they usually get discharged home.”
At the same time, “unfortunately, we do see some really devastating new cancer diagnoses, we see some car accidents, so it’s definitely emotional. I think my co-workers do a really good job of supporting each other through those difficult times. Healthcare can be sad, and I think it’s especially sad when you know something bad happens to a child. And we do a lot of compassion with the families as well; we take care of the whole family, not just the child.”
Again, she comes back to the education aspect of her work, even for things families don’t specifically bring in their kids for, like properly installing car seats.
“When we’re at the triage desk, we first bring the kid in, we make sure they’re safe, and then that’s another point where we can just educate them and do that community health and make sure everyone’s safe by teaching families simple things like car seats.”
Going beyond the basics is how Ingraham-Shaw has really made a difference, though, implementing new ideas in an organization she says is very interested in hearing them.
“My management team is just really open. We have a lot of freedom to do things,” she said, before giving another example in the behavioral-health realm.
“One of my co-workers and I, a few years ago, started a behavioral-health committee. We try to meet monthly, just to talk about what’s going on with the unit, trying to work on different projects,” she explained. “One thing we did was make an informational pamphlet for the families and the patients that come in for behavioral-health issues because the way we treat them is much different than other patients. And sometimes they’re there for a really long time. So we want to do what we can just to support the families a little bit more.”
Do Carmo praised Ingraham-Shaw for identifying barriers in communication and creating a tool that has improved communication between nurses and patients. “Ellen works very closely with the behavioral-health team to ensure the behavioral-health population receives the needed care plans and treatments.”
Long-time Passion
Ingraham-Shaw’s interest in mental health was clear when she first studied psychology in college, but at the time, she couldn’t have predicted how it would become an important aspect of her career.
“When I was looking for jobs, if I didn’t find a teaching job, I was looking for other psychology-related jobs,” she said, adding that she’s in graduate school now, working on her doctor of nursing practice degree (DNP) to be a psychiatric nurse practitioner.
“I always thought that was a possibility, but I didn’t think this was the route I’d take,” she said. “For nurse practitioners, at least, the education track is different. So you’re a nurse first, so you get that compassionate care and bedside manner down first. And then you start learning the more advanced things.”
Once she has her DNP, she said she’d like to stay in the pediatric arena, although she’s hoping to gain a wide range of experience through her clinical rotations.
“Baystate in general is very supportive of education,” she added, noting the system’s tuition-reimbursement and loan-forgiveness programs, in addition to its affiliation with UMass Medical School’s Springfield campus, which is where she’s taking her graduate track.
“One of the reasons why I chose that school is because they have a focus on diversity and behavioral health,” she noted. “So I’ve been working hard, but I have also been lucky to find myself in places, and around people, that are supportive and inspirational, and I’ve been given a lot of opportunities to focus on the things that I want to do.”
As part of her graduate education, Ingraham-Shaw is hoping to focus on opioid and overdose education in her scholarly project. “It’s something I’m passionate about, and I’ve done a lot of my own learning. So I’m hoping to do some more research and actually implement some projects with that.”
For her work creating and cultivating a handful of truly impactful projects at Baystate already, but especially for the promise of what she and her colleagues have yet to come up with, Ingraham-Shaw is certainly an emerging leader in her field, and a Healthcare Hero. n
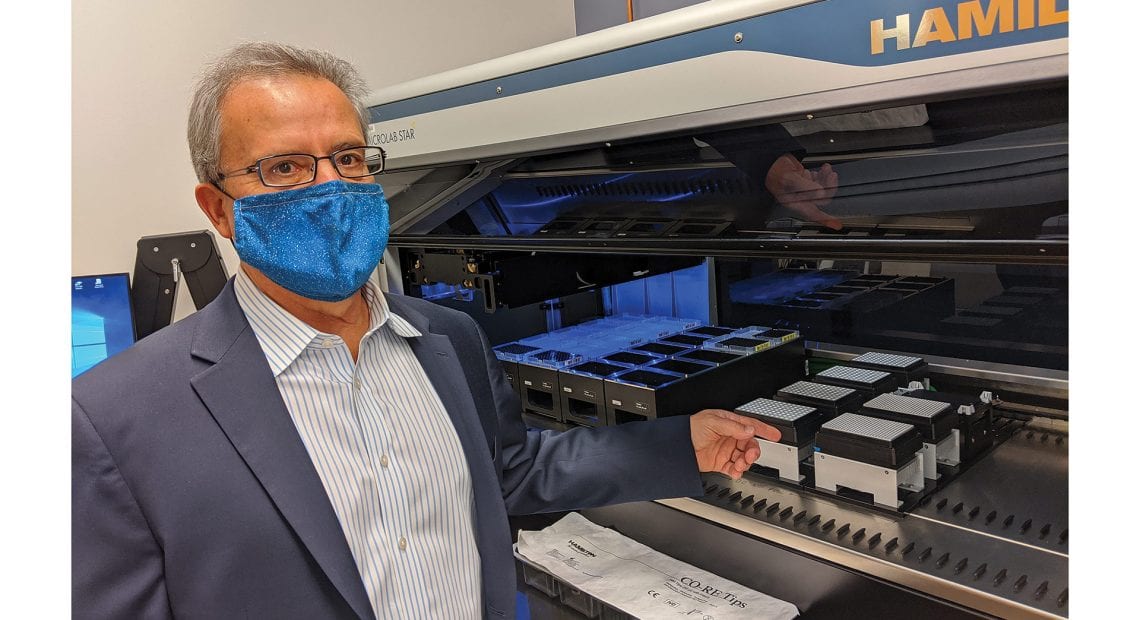
Practice Manager of Thoracic Surgery, Nursing Director of the Lung Screening Program, Mercy Medical Center
She Has a Proven Ability to Take the Bull by the Horns

It’s been seven years now, but Ashley LeBlanc clearly remembers the day Dr. Laki Rousou and Dr. Neal Chuang asked her to consider becoming the nurse navigator for their thoracic surgery practice at Mercy Medical Center.
She also clearly remembers her initial response to their invite: “absolutely not.”
She was working days in critical care at the hospital at the time, and liked both the work and the schedule: three days on, four days off, she told BusinessWest, adding that it takes a while for a new position like this to get approved and posted, for interviews to take place, and more — and the doctors used the following weeks to make additional entreaties, with reminders that she wouldn’t have to work any weekends or holidays.
But the answer was still ‘no’ until roughly six months after that initial invite, when she had one particularly challenging day on the floor with a very sick patient. Challenging enough that, when Rousou tried one more time that afternoon, ‘no’ became “I’ll update my résumé and hear you out.”
“He got me at a weak moment, and it was the best decision I ever made, because they have been amazing mentors, and they’ve opened my mind up to this whole other world,” she said, adding that her career underwent a profound and meaningful course change, one that led her to being named a Healthcare Hero for 2023 in the Emerging Leader category.
Indeed, during those seven years, LeBlanc has emerged as a true leader, both in that thoracic surgery practice, which she now manages, and in efforts to promote awareness and screening for lung cancer — one of the deadliest cancers, and one she can certainly relate to personally. Indeed, she has lost several family members to the disease, many of whom would have qualified for screening had it been available at the time of their diagnosis.
“He got me at a weak moment, and it was the best decision I ever made, because they have been amazing mentors, and they’ve opened my mind up to this whole other world.”
In many respects, and in many ways, she has become a fierce advocate for patients related to lung cancer screening, treatment, and research, and concentrates her efforts on ways to decrease the mortality rate of lung cancer and break down the stigma of that disease by educating the community, connecting them to resources, and, in many respects, guiding them on their journey as they fight lung cancer.
When the screening program was launched, those involved didn’t really know what to expect, LeBlanc said, adding that, in the beginning, maybe a handful of people were being screened each month. Now, that number exceeds 250 a month, and while only a small percentage of those who are screened have lung cancer, she said, each detected case is important because, while this cancer is deadly, early detection often leads to a better outcome.
This is turning out to be a big year for LeBlanc, at least when it comes to awards from BusinessWest. In the spring, she suitably impressed a panel of judges and became part of the 40 Under Forty Class of 2023. And in late October, she’ll accept the Healthcare Heroes award for Emerging Leader.
The plaques on her desk — or soon to be on it — speak to many qualities, but especially an ability to work with others to set, achieve, and, in many cases, exceed goals, not only with lung cancer screening, but other initiatives as well.

Dr. Laki Rousou never stopped trying to recruit Ashely LeBlanc to manage the thoracic-surgery practice at Mercy Medical Center, and he — and many others — are glad he didn’t.
Staff Photo
Rousou put LeBlanc’s many talents in their proper perspective.
“Before we even had the formal program, I would say something sort of off the cuff, like, ‘I wish we could do this’ … and the next week, I would have the answer, or it would be done,” he said. “Then it turned into ‘OK, let’s try and do this,’ and in the next week or two weeks, it would be done. And then it turned into a situation where she would have an idea and we would talk periodically, but she would take the bull by the horns and just do things that were best for thoracic surgery, but also the screening program.”
This ability to take the bull by the horns, and many other endearing and enduring qualities, explains why LeBlanc is a true Healthcare Hero.
The Big Screen
There’s a small whiteboard to the right of LeBlanc’s desk. Written at the top are the words ‘World Conquering Plans.’
This is an ambitious to-do list, or work-in-progress board, with lines referencing everything from a cancer screening program for firefighters to something called a Center for Healthy Lungs, which would be … well, just what it sounds like. “That’s a bit of a pipe dream,” she said. “We’re going to need our own building.”
While it might seem like a pipe dream, if it’s on LeBlanc’s list of things to get done … it will probably get done. That has been her MO since joining the thoracic surgery practice, and long before that, going back, for example, to the days when she worked the overnight shift as a unit extender at Mercy until 7, then drive to Springfield Technical Community College for nursing classes that began at 8.
“Sometimes, I would snooze in the car for 15 or 20 minutes,” she recalled, adding that she wasn’t getting much sleep at that time in her life. “You just do what you have to do to make it happen.”
Initially, she thought what she wanted to make happen was a career in law enforcement — her father was a police officer in Northampton — but her first stint as a unit extender at Mercy, while she was attending Holyoke Community College, convinced her she was more suited to healthcare.
But plans to enter that field were put on ice (sort of, and pun intended) when her fiancé, a Coast Guardsman, was stationed in Sitka, Alaska.
She spent three years there, taking in winters not as bad as most people would think, and summers not as warm as they are here, but still quite nice. And also working for the Department of Homeland Security as a federal security agent for National Transportation Safety Board at Sitka’s tiny airport.
“The evidence is staggering concerning the number of people who have a scan done, and they have an incidental finding, and there is no follow-up for that incidental finding.”
LeBlanc and her husband eventually returned to Western Mass. after a stint on the Cape, and she essentially picked up where she left off, working as a unit extender at Mercy.
“It was five years later, and it felt like I never left,” she said, adding that she soon enrolled in the Nursing program at STCC and, upon graduation, took a job on the Intermediate Care floor, which brings us back to the point where she kept saying ‘no’ and eventually said ‘yes’ to Rousou and Chuang (who is no longer with the practice).
Rousou told BusinessWest they recruited her heavily because they knew she would be perfect for the role they had carved out — and they were right.
Over the past seven years, LeBlanc has put a number of line items on the ‘World Conquering Plans’ list, and made most of them reality, especially a lung cancer screening program, which wasn’t even on her radar screen when she finally agreed to interview for the job.
Indeed, she was prepared to talk about patient education and how to improve it and make it more comprehensive when Rousou and Chuang changed things up and focused on a screening program.
Thinking Big
Once she got the job, she focused on both, with some dramatic and far-reaching results.
As for the screening program, she said such initiatives were new at the time because the Centers for Medicare Services had only recently approved insurance coverage for such screenings. At Mercy, with Rousou, Chuang, and, increasingly, LeBlanc charting a course, extensive research was undertaken with the goal of incorporating best practices from existing programs into Mercy’s initiative.
“We had no idea what our expectations should be or how it would be received in the community — it was a very new thing,” she recalled. “That first month in 2017, we did seven scans; then we did 29, and by the end of the year, it was over 50 scans a month. A year after we started, it was over 100.”
Now, that number is more than 250, she said, adding that such screenings are important because, while lung cancer is the deadliest of cancers, there are usually no visible signs of it — such as unexplained weight loss, coughing up blood, or pneumonia — until its later stages.
“When patients are diagnosed with stage 4 lung cancer, the treatment is, by and large, palliative, not curative,” she explained, “which makes it extra important to try to diagnose these people with lung cancer at an earlier stage.”
In addition to her work coordinating the screening program, LeBlanc also handles work implied by her initial title — nurse navigator.
This is work to help the patient understand and prepare for the procedure they are facing, such as removal of a portion of their lung, and answer any questions they may have.
“When the surgeon leaves the room … that’s when a patient will take that deep breath and say, ‘I have so many questions,’” she told BusinessWest. “It can be overwhelming, and this gives me an opportunity to answer those questions, which can involve anything from the seriousness of the procedure to where to park or what to bring to the hospital with them.”
Meanwhile, she has taken a lead role in efforts to build a strong culture within the thoracic surgery and cancer screening programs, where 14 people now work, and make it an enjoyable workplace, where birthdays and National Popcorn Day are celebrated, and teamwork is fostered.
“I think it’s important to enjoy where you work, and when we’re happy, I think that carries over to patients, and they feel that,” she said. “At Easter, we have an Easter egg hunt, with grown, professional adults running around the office looking for Easter eggs. It seems silly, but it’s wonderful at the same time.”
Then, there’s that ‘World Conquering Plans’ board next to her desk. LeBlanc said she and the team at the practice have made considerable progress with many of the items on that list, including plans to expand the office into vacated space next door with an interventional pulmonary department and an ‘incidental nodule’ program.
The interventional pulmonary program is a relatively new specialty that focuses on diagnosis of lung disease, she said, adding that an interventional pulmonologist has been hired, facilities have been created, and patients have been scheduled starting early this month.
Progress is also being made on the incidental nodule program, which, as that name implies, is a safety-net initiative focused on following up on the small, incidental nodules on the lungs that show up on scans other than lung cancer screenings and are often overlooked.
“The evidence is staggering concerning the number of people who have a scan done, and they have an incidental finding, and there is no follow-up for that incidental finding,” she explained, adding that such findings often get buried or lost in reports. “When patients come to Dr. Rousou, they’ll often say, ‘I’ve had a scan every year for the last so many years; how come no one saw this until now?’”
Breathing Easier
As for the Center for Healthy Lungs … that is a very ambitious plan, she said, one that exists mainly in dreams right now.
But, as noted earlier, LeBlanc has become proficient in making dreams reality and in drawing lines through items on her whiteboard.
That’s what Rousou and Chuang saw when they recruited LeBlanc — and kept on recruiting her after she kept saying ‘no.’
They could see that she was an emerging leader — and a Healthcare Hero. n
Personal Trainer and Owner, Movement for All
She Inspires Others to Improve Their Mobility — and Quality of Life

One of Cindy Senk’s first experiences with yoga wasn’t a positive one.
Her back was very painful on the right side. “The yoga teacher came up in my face and said, ‘you can do better, you can do better’” — but not in an encouraging way, she recalled.
“It was almost hostile — this in-my-face attitude,” she went on. “I was really taken aback by that. I felt like, you don’t know me; you don’t know my health history; you don’t know what I’m feeling. I wanted to say, ‘get out of my face,’ but I didn’t — I just stepped back, and I never went back to that yoga studio.”
The experience drove her when she launched her own fitness and training practice, Movement for All, 20 years ago.
“I decided I would never be that teacher. I would never put someone in that particular place,” Senk told BusinessWest. “My philosophy as a teacher is to educate and empower my students, my clients, to make the choices that feel right because they feel it in their body. They know how they feel.”
That philosophy has led her not only to success with Movement for All, but 40 years of successes with specific populations, like people with arthritis, older individuals, and clients with cognitive challenges — because she understands that everyone, no matter their challenges, can thrive when they’re not treated in a cookie-cutter way.
Kelly Gilmore understands this. One of three clients who nominated Senk as a Healthcare Hero, Gilmore, a department chair at West Springfield High School, was hospitalized with a condition that diminished her mobility, stamina, and overall physical and mental state so severely that she couldn’t return to her teaching position.
“None of the numerous medical specialists that I continued to see regularly could offer a path toward improvement, beyond pain relief,” she wrote. “I set out to find a healthcare/fitness professional that was committed to helping me restore my health, strength, and mobility. Cindy offered exactly that. She met me where I was and created a personalized plan to move me to where I needed to be. She empowered me to take charge of my healing, unlocking the power inside of me, one step at a time.”
Starting a yoga regimen sitting in a chair, rather than on a mat on the floor, Gilmore began, within the next few months, to move freely, climb stairs, and go on walks. “Most importantly, I was in charge of my classroom again, offering my students the energy and vitality they deserve from their teacher.”
That’s real impact on clients with real problems. Multiplied over four decades, it’s a collective impact on the community, especially populations not always served well, and it certainly makes Senk deserving of being called a Healthcare Hero.
Brotherly Inspiration
Senk traces her passion for helping people to her childhood — in particular, her experiences with her younger brother, Bobby, who was born with cerebral palsy in 1955, long before the Americans with Disabilities Act codified many accessibility measures.
But Bobby had his family.
“My mother was a real advocate for him,” Senk recalled. “And we grew up in this environment in Forest Park where Bobby was one of the gang. We would accommodate him if he had trouble keeping up because of his crutches; we would just get him in a wagon and drag him around the neighborhood. He was always just part of the group. There was no, ‘well, Bobby can’t do that, so we can’t do it.’ It was never like that. It was always, ‘how can we creatively include him?’ And I think that’s really where this passion of mine comes from.”
Senk has had her own share of physical challenges as well; she was diagnosed with spinal issues at age 18 — issues that led to a lifetime of arthritis and have given her unique insight into people with similar problems, and led her into decades of advocacy in the broader arthritis community.
She’s never been free from arthritis; in fact, the day she spoke with BusinessWest at her home, Senk said she woke up with a lot of pain.
“My philosophy as a teacher is to educate and empower my students, my clients, to make the choices that feel right because they feel it in their body. They know how they feel.”
“It was just one of those days, you know?” she said. “So I started my gentle yoga I do every morning, I got in the shower, I was moving around my house, I had a class online that I teach, and then I had a client. And now I feel 1,000% better from when I woke up at 5:30 because I’ve been moving for six hours.
“It comes down to wanting to help people be functional, be fit, and have tools they can use to help themselves with whatever challenges they’re facing. And I think my passion for that came from a young age. Everything kind of flowed from all that: discovering how movement helps me and sharing that with others. Because I know how much movement helps me.”
Senk started her career with group exercise like step aerobics and regular low-impact aerobics, and later started practicing yoga to help her back — her main arthritic trouble spot. That was 35 years ago, and yoga has been an important part of her practice ever since.

Cindy Senk calls these women “the heart of my in-person classes on Tuesday nights.”
“I have my basic certification, but then I have specialties in yoga for arthritis, accessible yoga, subtle yoga, and I use all of those to put together whatever program I need for this particular client in this particular class. I feel lucky to have a lot of tools in my toolbox.”
It’s been gratifying, she said, to help clients discover those tools, especially those who didn’t think they could achieve pain relief and mobility.
“A lot of times, in the beginning, people that are in chronic pain are very tentative about movement because they think they’re going to hurt worse,” she said, adding that she draws on her experience as a volunteer and teacher trainer with the Arthritis Foundation — and her own experience with arthritis, of course — to help them understand the potential of yoga and other forms of exercise.
“It’s the idea of the pain cycle, where we think, ‘oh I can’t; it hurts,’ so we move less, and then we hurt more,” she explained. “The idea of movement breaks that pain cycle. You’re giving the power to the client through movement. It’s a journey that I’m on with them.”
It’s a good idea, Senk said, for people in pain to first see their primary-care doctor or a specialist to find out exactly what’s wrong and what their options are, whether that’s yoga, an aquatic program, a walking program, or another activity that can keep them mobile.
“She met me where I was and created a personalized plan to move me to where I needed to be. She empowered me to take charge of my healing, unlocking the power inside of me, one step at a time.”
“There are more than 60 million of us in this country who have arthritis — and that’s doctor-diagnosed, so a lot of people probably have arthritis and are not doctor-diagnosed. And it’s not just older people; it’s kids as well. It’s very pervasive, unfortunately. So you need to get the knowledge first, and then, if you want to move and exercise or whatever it may be, you need to find a professional who knows what they’re doing.”
Living Her Passion
Senk’s four-decade career as a fitness professional has brought her to commercial fitness settings, hospitals, senior-living communities, corporate environments, and the studio she runs out of her own home. She has also taught as an adjunct professor at Holyoke Community College, Springfield College, and Manchester Community College, in addition to 25 years of volunteerism with the Arthritis Foundation and her role chairing of the Western Massachusetts Walk to Cure Arthritis for the past three years.
That’s a lot of passion poured into what essentially boils down to helping people enjoy life again.
“The bottom line for me is to just encourage people to find things that are helping them stay functional, whether it’s a gym they love to go to or a more private type of setting like I offer here,” she said, noting that her home studio also includes outdoor activities and virtual classes.
“I think it’s important for people to find where they fit, where they’re comfortable. And if they go to a gym or they go to a yoga studio and it’s not their fit, just keep looking. Find your people. Find the people that really speak to you and that will support you and not judge you and not put you down because maybe you can’t bend as much.”
She said she loves hearing clients say they were able to take a vacation and hike without falling down, ride a paddleboard, even reach up into the cabinets at their cabin.

Cindy Senk demonstrates some of the simple tools of her trade.
“I live for stuff like that. As somebody who has arthritis and chronic pain, I know it can be very easy to get in the bubble of your own head and say, ‘I can’t move today … right?’ But when I’m having my class here and I’m focusing on them, that takes a whole other attitude. It takes me out of my own pain space, if you will, and helping other people uplifts me. It just brings me joy and helps me feel better. It really does.”
It certainly has helped Lisa Borlen, a teacher at Valley View School in North Brookfield, one of Senk’s nominators, who shared how working with her has given both her and her mother a new outlook on life. Looking back to her recovery from surgery in 2021, she emphasized how Senk makes everyone feel welcome.
“I was still in a sling when I returned to yoga, and Cindy offered suggestions for poses from seated in a chair to standing against a wall,” she recalled. “My safety was her utmost concern. As I grew stronger, she made adjustments to the practice. I could continue to practice yoga with my class and I always felt supported. My physical therapist and surgeon were pleased with my progress and thought that the yoga classes were instrumental in my recovery.”
Susan Restivo, a retired Springfield teacher who also nominated Senk, joined Gilmore and Borlen in stressing that Senk is not only a teacher, but a lifelong learner, and that informs her work in the community.
“She is doing what she wants — what she started doing as a big sister, never knowing that helping her brother would be the start of her journey of serving others,” Restivo wrote. “Way back then, there was no equipment or an understanding of services for those that needed a Cindy Senk.”
That equipment and understanding are available now, though. So is Senk, and a lot of people are living more active, more pain-free, and happier lives because of the way she lives her passion.
“People say, ‘oh, you’re 70, you should retire, you should slow down,’” she said. “But I still feel like I have things to offer. I really do. I feel like I have people to help, ways to be of service, and I still have a lot of energy to do it. So that’s what I do.”
Nurse, Urology Group of Western New England
During Her Long Career, She Has Made a World of Difference

Now 87, almost 88, Joanne (Jody) O’Brien is two decades and change past what the Social Security Administration considers ‘full retirement age.’
But she is still working — two days a week as a triage nurse for the Urology Group of Western New England (UGWNE), in its Northampton office. She’s doing plenty of other things to keep busy, which we’ll get to, but for now, let’s focus on her day job — and the fact that she still has one.
When asked why, her face curves into a huge smile — it seems to be almost permanently like that — and she offers a simple and direct explanation.
“I love nursing,” she told BusinessWest with a voice that would imply this would be obvious if she’s been doing it for more than 67 years. But she wanted to elaborate, and did.
“I lucked out picking nursing as a profession coming out of high school because it’s just been the most rewarding career I could possibly imagine,” she said. “I’ve enjoyed it so much that I don’t want it to end. As long as someone keeps me employed, I’ll keep coming to work.
“I absolutely love what I do — I can’t say enough about how great nursing has been for me,” she went on. “It’s a wonderful career to have. I’ve tried so many different aspects of it, and I’ve loved them all. So I figured there’s no sense packing it in if you love what you’re doing.”
Her career has placed her in many settings — from a hospital ship that was part of Project Hope in the early ’60s to Western New England College, where she was director of Health Services; from an eye-surgery office in Hawaii to the Hampden County Jail and House of Correction, where she was a per-diem nurse and, later, director of nurses, with many other stops as well.
“I lucked out picking nursing as a profession coming out of high school because it’s just been the most rewarding career I could possibly imagine. I’ve enjoyed it so much that I don’t want it to end. As long as someone keeps me employed, I’ll keep coming to work.”
But longevity and this variety of professional settings only begins to explain why O’Brien has been chosen as a Healthcare Hero for 2023 in the Lifetime Achievement category. Beyond her various day (and night) jobs, she has undertaken a number of service and volunteer assignments — from reading at Valley Eye Radio to taking care of orphans in Romania; from teaching English to nursing students in China to tagging sharks in Belize; from restoring and protecting turtle habitats in Costa Rica to working at Whispering Horse Therapeutic Riding, supporting riders with disabilities.
All this suggests she could easily have been nominated in several, if not all, the categories of Healthcare Heroes. Because of the length, variety, and broad impact of her work, she is being honored in the Lifetime Achievement category, one that has traditionally been dominated by administrators. In this case, though, it is going to a provider. A provider of care. A provider of hope. A provider of inspiration.

Jody O’Brien with staff members at the Urology Group of Western New England’s Springfield office.
Staff Photo
Through her 87 years, 67 of them as a nurse, she has seen just about everything, including a global pandemic. Summing it all up, she said her passion for helping others hasn’t dimmed — and has probably only grown stronger — nearly 70 years after she entered nursing school.
This enthusiasm and energy was conveyed by Dr. Donald Sonn, a physician with UGWNE, who was among those who hired her 18 years ago.
“When we first interviewed her, we were struck by how positive and effervescent she was, and how energetic she was,” he recalled. “I’m constantly amazed by her energy and her positive attitude.”
Calling her an “ombudsman” for the practice’s patients, Sonn said O’Brien consistently draws praise for her calm, steady hand (and voice on the phone) and her desire to assist others.
All of this — and much more — explains why she is a true Healthcare Hero.
Riding the Wave
‘Cuba si, Yanquis no.’ That translates to ‘Cuba yes, Yankees no,’ and it’s a phrase, and a song, that O’Brien heard repeatedly as she served aboard the USS Hope, the former Navy hospital ship that was chartered to the People to People Health Foundation in 1960, when it was docked in Trujillo, Peru two years later.
“The people who met us at the dock were Communists, and they did not want us there,” she recalled, adding that the exploits of the USS Hope in Peru later became the subject of the book Yanqui Come Back!
O’Brien spent a year on the Hope, earning a $25 monthly stipend. But as those credit card commercials used to say, it was a learning experience that was priceless.
She worked beside a constantly changing team of doctors that performed surgery on the ship and in hospitals on the mainland, with procedures ranging from plastic surgery for burns to work to address cleft palate and hairlip, to removal of tumors, some of which had grown to enormous sizes because the patients hadn’t seen a healthcare provider in years, if not decades.
Urologist Dr. Donald Sonn calls Healthcare Hero Jody O’Brien an “ombudsman” for the practice’s patients.
Staff Photo
“People would walk for miles to get to the ship to be treated, and we treated everyone who needed it,” she recalled. “It was such a learning experience for me working with all these doctors.
“I was still young and adventurous,” she went on as she talked about how she paused her career, sort of, to serve on the ship, adding that she has remained young at heart and has always, in her recollection, been adventurous.
Indeed, the book on her life and career has many intriguing chapters, some of which are still being written. In literary circles, they would call this a ‘page turner.’
Our story starts in Iowa, where O’Brien was born and raised, and where she decided she wanted to be a nurse. She attended nursing school in Davenport — a three-year diploma program that cost $500.
Upon graduation, she took a job in Davenport, but soon thereafter, she went to Hawaii to stay with a friend who had recently had a baby and wanted her company while her husband was deployed.
It was in Hawaii that O’Brien became acquainted with Project Hope. She visited the ship when it was docked and became intrigued with its mission. After returning to Iowa, she filled out an application to serve in Project Hope as an operating room nurse, and in 1962, she was approved for service.
During her year on the USS Hope, she met a volunteer named Ed O’Brien, from Holyoke. Upon returning to Iowa, she would drive to the Paper City to renew acquaintances. They would marry in 1963 and eventually settle in East Longmeadow.
Thus would commence a series of assignments in the 413, but also well beyond it.
Care Package
These included a lengthy stint at what was then Wesson Women’s Hospital, working in labor and delivery, and another as a nurse practitioner in an ob/gyn office.
From 1983 to 1988, she served as director of Health Services at Western New England College, handling the needs of 6,000 students, and also as a per diem nurse at the Hampden County Jail and House of Correction.
She then accepted a travel nurse assignment at Castle Hospital in Kailua, Hawaii. She stayed in Hawaii for a dozen years, also serving as nurse manager of an eye-surgery center and as branch director of Nursefinders of Hawaii. And while in the Aloha State, she earned a master’s degree from Central Michigan University.
“She would go on a trip every three or four months, and it was always something really fascinating — volunteering in some third-world country or teaching children or reading to the blind. She has a tremendous record of service.”
She returned to Western Mass. in 2000 and took a job as area director of Nursefinders of Eastern Massachusetts, and soon thereafter became a flex team manager at Baystate Medical Center, managing 60 RNs, 25 technical assistants, 45 constant companions, and the ‘lift team.’
At the Urology Group of New England, which she joined 18 years ago, she works two days a week — Monday and Wednesday. The former is generally the busiest and perhaps the most difficult of the days of the week, but that’s when the group needs the help, so that’s when she works.
O’Brien’s whole career has been like that, in many respects — showing up when and where the help is most needed.
That’s true professionally, but also in her work as a volunteer, with work that is wide-ranging, to say the least.
Indeed, during the three days she’s not working at the Urology Group — and all through her life, for that matter — she has found no shortage of ways to give back and be there, for both people and animals.
Among them is her work with Valley Eye Radio, where she reads the local newspaper for the benefit of those who can’t read it themselves.
“It makes you feel good to know that, for people who cannot read or have difficulty reading, we can share what’s going on today in Springfield or the United States or the world,” she said. “We can share that information with them.”
Meanwhile, she also volunteers with Greater Springfield Senior Services, helping individuals who can no longer handle their own finances with bill paying and other responsibilities, and with Whispering Horse Therapeutic Riding, a nonprofit that, among other things, brings horses to nursing homes, where residents can feed and pet the animals.
“The way they light up when they see these horses … it’s so gratifying,” she told BusinessWest, adding that she and a colleague will visit facilities regularly — sometimes weekly, other times monthly.
Animals have always been a big part of her life — and her strong track record of giving back. In addition to tagging sharks and restoring turtle habitats, she has also volunteered at animal sanctuaries in Australia to care for koalas, often taking her grandchildren with her on such service trips, introducing them to the many rewards that come with such work.
“At this age, you know you don’t have many more days to fill, so you fill each one of them,” she said, but concedes that she’s always wanted to stay busy.
“She’s done so much in her life … I’ve always looked forward to listening to her talk about trips, her escapades,” said Sonn, choosing that word carefully. “She would go on a trip every three or four months, and it was always something really fascinating — volunteering in some third-world country or teaching children or reading to the blind. She has a tremendous record of service.”
In both aspects of her life — as a nurse and as a volunteer — the common thread has been a desire to help those in need, and this explains why she has been chosen as a Healthcare Hero for 2023.
“I loved working at Western New England; the college kids were a joy to work with,” she said, adding that each stop in her career has been different — and enjoyable. “There’s something about taking care of people and helping them deal with mental and physical problems and seeing what you can do to help them in their lives.”
Still Making a Difference
There are many people who have worked well into their 80s in healthcare. And there are many people who have put dozens of lines on a résumé detailing a lengthy list of career stops.
But there are few who have the passion, dedication, and resolve to use their talents and their love for helping others to make a world of difference, in every aspect of that phrase.
Jody O’Brien is such an individual. That commitment has helped her stand out in this field for seven decades. It makes her a Healthcare Hero. n
Here, Shared Research by Nurses and Engineers Will Benefit Patients Everywhere

Co-directors Frank Sup and Karen Giuliano. Leah Martin Photography
Intravenous (IV) infusion pump systems are among the most recognized technologies in healthcare, used by about 90% of hospital patients.
They’re also hopelessly out of date, Karen Giuliano said.
“The design has been around a long time, and hospitals don’t buy one; they buy an entire fleet. They have to invest in training, service contracts, and IT infrastructure. To install a platform is a huge investment and effort.”
And that has led to stagnation, she added. “Over 80% of pumps are really old platforms and don’t do the job they need to do. They’re not developed for today’s standards.”
Enter the Elaine Marieb Center for Nursing and Engineering Innovation at UMass Amherst, which has made improving the safety and usability of IV smart pumps one of its first major projects. The team has been exploring flow-rate accuracy in a variety of settings and use cases, with the goal of developing pumps that eliminate inaccuracy, inconvenience, and resulting medical errors through new technology and simplified design.
The work is gaining widespread attention, as Giuliano, co-director of the center and associate professor of Nursing, and postdoctoral research fellow Jeannine Blake were recently recognized by the Assoc. for the Advancement of Medical Instrumentation (AAMI) for the Best Research Paper in 2021.
Their paper, “Nurse and Pharmacist Knowledge of Intravenous Smart Pump System Setup Requirements,” explored knowledge of intravenous smart-pump system setup requirements among nurses and pharmacists. The results were published in Biomedical Instrumentation & Technology, AAMI’s peer-reviewed journal.
“There’s already a critical nursing shortage, fatigue, and burnout. How can robotics be used to maybe alleviate some of those problems? We can use robotics as an extension of the nurse.”
“We don’t want to build a new pump; we want to build a set of requirements for manufacturers that have been sitting idle for too long without being forced to innovate for the safety of patients and the workflow of the nurses,” Giuliano told BusinessWest.
The effort demonstrates the types of innovation she and Frank Sup, associate professor of Mechanical and Industrial Engineering and the other co-director of the Elaine Marieb Center for Nursing and Engineering Innovation, intended when they launched the center in early 2021. It also reflects the cross-educational opportunities for people like Blake, the first nursing doctoral student to enter an engineering postdoctoral fellowship at UMass.
“Students have come out of here with a siloed education, nurses and engineers. There’s not a natural inkling to work together; they might not even know the importance of collaborating in that way,” Giuliano said. “What we want is to have students graduate that already have that in common, to reach across the aisle. The healthcare environment should not be a silo.”
Under Sup’s leadership, the center has also begun research on the use of robotics in healthcare. It teams doctoral students from both engineering and nursing, as well as an undergraduate nursing honors student, to identify challenges and develop robotic solutions to improve healthcare delivery for patients and providers.
The incorporation of robotic technology into the healthcare system is ongoing and already includes innovations like fully autonomous disinfecting systems and invasive surgical devices, and Sup feels it’s essential that these new technologies are integrated into the field of nursing at multiple levels, including hospital administration, the clinical workplace, and university education. And students need to interact with robots to better understand and utilize this technology in a controlled setting before patient care is involved.
“What are robotics, what can they do, what are they good for, and how can we start to train nurses and engineers in robotics? What day-to-day situations might nurses face in the hospital, clinic, and home, and what might be the best use cases for these robotics systems?” he asked. “That’s where this program started. Nurses are not typically trained in robotics, so we actually start to expose them to these things.”
That may seem like a scary thought to some, or imply that robots could replace nurses, but that’s far from the case, Sup added.
“There’s already a critical nursing shortage, fatigue, and burnout. How can robotics be used to maybe alleviate some of those problems? We can use robotics as an extension of the nurse, potentially doing things when they’re not there, like monitoring and lower levels of service.”
By bringing nurses and engineers together at the earliest stages of product innovation, the Elaine Marieb Center promises a raft of such breakthroughs that will result in better technology and, more important, better patient care.
Come Together
This is how Giuliano and Sup described the center’s mission at its opening last year:
“Today, healthcare technologies are too often made without the insights and understanding that clinicians bring to the table. Nurses are end users, facing healthcare challenges on the frontlines of patient care. Engineers have the expertise and skills to envision and create medical devices and can work with nurses who bring the real-world healthcare experience needed to design the best possible products and solutions.
“This transformation depends heavily on collaborative research and development work among nursing, engineering, and other disciplines,” they went on. “The ability to quickly and effectively develop and test innovations requires both nursing and engineering skillsets. The power of the nurse-engineer approach is derived from the mutual collaboration between the two, where the nurse identifies the problem, and the engineer facilitates potential solutions.”
One problem in the past, both of them explained to BusinessWest, was that products too often wound up in the hands of nurses too far along in the design and development process to change very much.
“I realized how important it was to have a front-end-user perspective built into the products rather than trying to back-engineer it when it’s 90% done.”
Giuliano, with more than 25 years of experience in critical-care nursing, medical product development and innovation, and patient-centered clinical outcomes research, should know. Prior to joining UMass Amherst, she spent many years working on medical product development from an industry perspective, including 12 years with Philips Healthcare.
Early in her career, she said, “I realized how important it was to have a front-end-user perspective built into the products rather than trying to back-engineer it when it’s 90% done.”
Now, at the center, “we have the ability to prototype things and test them in nursing simulation labs and test them in actual hospitals,” she added, the latter through a collaboration with Baystate Health.
Meanwhile, Sup was also a natural choice to co-direct the new center. As director of UMass Amherst’s Mechatronics and Robotics Research Lab, his research has long focused on developing human-centered mechatronic technologies for augmenting human performance and exploring how to enable robots to fluently interact physically with humans. To that end, he brought teams of nursing and engineering students together to work on senior capstone design projects.
The model was formalized as the Elaine Marieb Center for Nursing and Engineering Innovation with the help of two major gifts: $1 million in seed funding from alumni Michael and Theresa Hluchyj, longtime supporters of both the College of Engineering and the College of Nursing; and $21.5 million from the Elaine Nicpon Marieb Charitable Foundation to the College of Nursing, with a significant portion designated to support the new center.
“Innovation is often accelerated at the intersection of different academic disciplines,” Michael Hluchyj said when announcing the first gift. “The worldwide health crises resulting from the COVID-19 pandemic make clear the critical need for innovative solutions in clinical settings where both nursing and engineering play vital roles.”
And nurses need to have a seat at the innovation table early, Giuliano said.
“Nurses use more products and are part of more services than any other healthcare provicer,” she told BusinessWest. “If they’re not at the table, you’re not going to have the right products. They’re not going to be usable, and if they’re not usable, then they don’t do the job. And from an economic standpoint, they don’t generate the revenue that the company wants. So it’s a lose-lose, which we can turn into a win-win.
“We want to be a usability testing center,” she went on. “So if a company has a product at a certain point in development, has an idea what’s supposed to do and how it’s supposed to work and what its value is, we literally bring it into a sim lab.”
The usability test involves two people, a nurse and a volunteer patient, and both evaluate it, as test administrators watch how it’s used. “If the same mistake is made over and over, it’s a design flaw; it’s not a user error,” Giuliano explained. Then all those results and perceptions go back to manufacturer, who has the opportunity to make improvements early in the process.
To that end, the emerging product prototyping laboratory on the Amherst campus will enable students to design and prototype new products, while a proposed usability laboratory on the Mount Ida campus will allow for product and service testing by frontline clinical end users.
“Having a better understanding of frontline clinician knowledge is a fundamental part of our overall program of research on improving the safety and usability of IV smart pumps,” Blake said when she and Giuliano received the AAMI’s award for their research earlier this year. “We are very excited to receive this award, which supports our continued efforts in this important area of research.”
Promising Outcomes
Better research resulting in better patient care is the goal, whether it’s IV pumps, robotics at the hospital bedside, or any number of other ongoing projects at the center, from cloud-based home-healthcare monitoring to wearable sensors that record body movement to assess chronic pain.
Part of the center’s raison d’être is that nurses and engineers are both trained problem solvers who rely on innovation to find solutions, but their paths rarely cross, and the timeframes required for them to find solutions are dramatically different.
Giuliano got her PhD while at Phillips Healthcare because “I really wanted to be a better researcher so I could test products in a meaningful way.” Later, she added, “I realized I liked academia — I was a better student as a 40-year-old than as a 20-year-old — and I knew I wanted to go into academia and try to recreate the nurse-engineer pairing in the academic environment.”
By teaming up with Sup, who was already pursuing those connections, and with the help of some generous gifts from supporters who saw potential in this model, a center was created that is not only generating some impressive outcomes, but is paving a new way for diverse minds to collaborate and improve the patient experience across the globe.
“The whole idea of this center is for academic clinicians, students, nurses, and doctors to bring in industry partners,” Sup said. “It’s going to be innovative, and it’s going to make a difference.”
And it clearly lives up to the title of Healthcare Hero in the category of Innovation.
“This work that’s being done will make its way to safety standards everywhere,” Giuliano said. “Nobody else is doing that. It’s huge.”
Joseph Bednar can be reached at [email protected]
This Critical Team Provides Hope — and a Roadmap to Recovery

Team members of the Addiction Consult Service at Holyoke Medical Center, from left: Eddie Rodriguez, John Martinez, Lauren Carpenter, Maria Quinn, Kelly Jean Deming, Em Moulton, and Jose Ramos.
Patrick Hamel remained calm and collected as he chronicled his quarter-century-long battle against addiction.
In telling that story, he recalled more relapses than he could count; how he lost jobs, alienated family and friends, and had run-ins with the law (including some B&Es to support his drug and alcohol use); getting thrown out of the house by his wife on a few occasions; the awkwardness of having his daughter visit him in a halfway house; and even that night a little more than two years ago when he decided that enough was enough and tried to end his life.
He didn’t become emotional — though he did have to stop and collect himself a few times — until he started talking about the Addiction Consult Service (ACS), or the Recovery Support Team, as members call it, at Holyoke Medical Center’s Comprehensive Care Center (CCC) and, especially, Maria Quinn, the charismatic psychiatric mental-health nurse practitioner and leader of that unit.
That’s because Quinn, those who work with her, and those to whom she has referred Hamel have enabled him to move beyond all that has happened to him and now lead a much better life.
“She just listened, and we came up with a plan. She got me hooked up with an amazing therapist. We saw each other every week — she was there for me; she was my support.”
“She is so amazing; she’s like my knight in shining armor,” said Hamel, who would then concisely and effectively sum up what Quinn and other members of this team do. “She just listened, and we came up with a plan. She got me hooked up with an amazing therapist. We saw each other every week — she was there for me; she was my support.
“Mind you, I’ve been in other types of medical treatment facilities and other programs,” he went on. “And I always felt like I was a number, or I was there to meet a quota; it was just a job. You can see with Maria that it’s not just a job; it’s something she’s passionate about.”

Patrick Hamel says those at the Addiction Consult Service listened and helped him come up with a game plan for recovery.
Hamel didn’t nominate the ACS for the Healthcare Heroes award, but his words, and the emotion attached to them, help explain why this special unit is being honored this year in the Community Health category.
In short, there are now hundreds, if not thousands, of people, who would say the same things if they were asked — about not just what the ACS does, but how it goes about its difficult and critically important work.
“We’re essentially ever-present — we like to make jokes that we stalk our patients while they’re here, even if we’re not fully involved,” she explained, adding that this is her way of saying that Recovery Support Team members make sure that those patients with addiction issues, either from the Emergency Department or inpatient units at the hospital — many of whom don’t have anyone to visit them while they are in the hospital, for many of the reasons Hamel listed above — have someone to talk to. And, far more importantly, someone to listen, someone who can help them determine what comes next for them, whatever that might be, including ongoing support at the CCC.
“That connection needs to happen so that people can stay and continue to get the treatment that they need,” said Quinn, adding that one of the goals of the program is to build trust among those touched by the ACS, because such trust has often been missing, and it is a key ingredient in their success.
“Historically, people with addiction haven’t been treated well in the healthcare system, so there’s a lot of mistrust, and we see that,” she noted. “We talk about it often and sense that the wall may be coming down and people are starting to bloom because we see our patients become a little more trusting.”
“One thing I’ve learned in this process is that everyone’s recovery is different. You have to listen to the patient to understand what they’re looking for in their recovery. By listening to them, I’ll know what kind of direction I can give them.”
Lauren Carpenter, a certified addictions nurse, agreed. When asked how she got into this specific line of work and what she likes about her work with this constituency, she said simply, “being able to help and care for people who aren’t used to being helped and cared for — building that connection and that rapport and making sure they know there is someone there who cares.”
The ACS is comprised of a nurse practitioner, a certified addictions nurse, a recovery-support coordinator, and recovery coaches. And, as noted, it is a collaborative effort, involving partners such as Tapestry Health, the Gándara Center (which employs the recovery coaches), River Valley Counseling Center, Hope for Holyoke, and the Holyoke Health Center. Together, these agencies are working to reduce opioid overdoses and help people like Hamel find a path to a better life.
The positive results of their efforts can be seen — and heard — with people like Patrick Hamel and countless others like him.
The Power of Hope
John Martinez’s battle against addiction was and is very similar to Hamel’s.
He described several stints of incarceration, homelessness, and, by his count, four suicide attempts.
He’s been sober now for 13 years and has spent the last several as a certified recovery coach, helping others find the strength and conviction to change their lives, as well as needed referrals and direction. The process starts simply with providing hope that life can get better, he said, adding that this isn’t all that coaches provide, but it may well be the most important thing.
“I remember being hopeless — I know what that’s like,” he recalled. “One thing I’ve learned in this process is that everyone’s recovery is different. You have to listen to the patient to understand what they’re looking for in their recovery. By listening to them, I’ll know what kind of direction I can give them.”

Recovery coach John Martinez says that, among other things, he provides those he counsels with the hope that life can get better.
As noted, recovery coaches are part of the team at the Comprehensive Care Center, and part of a broad, collaborative effort that has come together at a critical time for the Greater Holyoke area.
Indeed, while much of the focus the past few years has been on the pandemic, and understandably so, addiction has only become a bigger, more dangerous, and more deadly problem for the region.
The number of opioid-related overdose deaths increased 9% in Massachusetts in 2021 over 2020. Meanwhile, there are significant disparities in overdose rates, particularly among Black and Latino individuals in Massachusetts; from 2019 to 2020, there was a 70% increase in overdose deaths among Black/non-Hispanic individuals and a 10% increase in Hispanic/Latinx individuals. From 2020 to 2021, there was a 6% decrease in Black/non-Hispanic deaths and an increase of more than 7% for Hispanic/Latinx individuals, according to the Massachusetts Department of Public Health.
Steadily rising numbers over the past several years prompted the HEALing Communities Study, whereby scientists from the nation’s leading health agencies and four major academic institutions are partnering with communities in four states, including Massachusetts, to test a set of interventions designed to reduce overdose deaths by 40% over three years in participating communities.
Through a grant awarded to Boston Medical Center, a collaborative was created involving several agencies in Greater Holyoke, with Quinn taking the lead as the appointed addiction expert for the Holyoke community. The goal is to address opioid use, with a specific focus on overdoses, she said, adding that the linchpin of the initiative was creation of the ACS and the CCC.
“Prior to that, it was just me trying to do it all — start people on medication, get referrals out, try to make appointments, trying to get people to stay here [the hospital] — and it was challenging.”
“Our goal is not to cure them; our goal is to treat them with dignity and respect, and that includes treating their withdrawal. It includes giving education and resources. Some people decide that they no longer want to use and want to work toward abstaining and not using, and some don’t.”
With the grant funds, Quinn was able to hire Carpenter as well as a recovery-support coordinator and other team members.
Together, they have put together a system to “find patients,” said Quinn, noting that, before creation of the ACS, many would essentially fall through the cracks.
“Lauren became really good at figuring out which patients we should look at, and we started finding our patients and going to them, often intervening even before a consult was sent,” she told BusinessWest. “And that’s important because people would be leaving the hospital; if you were using opioids or were addicted to opioids, in particular, and didn’t get that, you would feel really, really sick, and if your withdrawal wasn’t being treated, you would probably be leaving.
“So we’d introduce ourselves and let people know why were there,” she went on, adding that, by and large, patients were not used to such a “proactive and impactive” approach to their care, and would have questions about what they could do for them.
What they can do is listen and begin a discussion about what happens next, said Carpenter, who walked through what might be a typical case.
“Someone will come into the ED, and I’ll get notified that this person is there and that they are in withdrawal,” she explained. “At that point, I will meet with the person, gather a history, assess their withdrawal, and then I’ll get Maria involved. I’ll talk with the ED provider, Maria, the addiction consult … Maria will meet with the patient, give recommendations, and order appropriate medications to treat their withdrawal. And when someone is actually on the med floor, we’d start the discussion of ‘what do you want to do from here?’”
As Quinn noted, the course varies with the patient. Often, those at the ACS will connect them to opioid-treatment programs, including two in Holyoke, if they are not already in a program, or connect them with a recovery coach while they are in the hospital.
“Not everyone’s goal is abstinence,” she said. “Our goal is not to cure them; our goal is to treat them with dignity and respect, and that includes treating their withdrawal. It includes giving education and resources. Some people decide that they no longer want to use and want to work toward abstaining and not using, and some don’t.”
When asked how those at the ACS measure success, Quinn said it depends on what how the patient would define that term.
“For some people, having air in their lungs is successful,” she told BusinessWest. “Anyone who leaves here feeling that they’ve been treated well … that’s a big success for me.”
Impact Statement
As he talked about Quinn and those she works beside at the CCC, Hamel stressed the present tense.
He is still working with these individuals at the CCC, and they are still making a huge impact on his recovery. He’s not sure they, and especially Quinn, understand just how much of an impact. So, he made it clear.
“I wouldn’t be where I am without them,” he said, adding that these individuals are more than healthcare providers, but are, in many respects, friends and even family.
“They want to make a difference — it’s not just about an f-ing paycheck,” he said in conclusion. “That’s where I get a little passionate and emotional; two years ago, I wanted to kill myself, and now…”
He didn’t finish the sentence, but didn’t really have to. The pause explained not only the journey from where he was to where he is now, but why the Addiction Consult Service is truly a Healthcare Hero.
George O’Brien can be reached at [email protected]
Chief and Physician, Baystate Noble Hospital Emergency Department
He Has Devoted His Career to Improving the Community’s ‘Safety Net’ Net’

Leah Martin Photography
Dr. Sundeep Shukla, or ‘Sunny,’ as most everyone calls him, has always felt at home in the emergency room, and he has never really wanted to work anywhere else.
There is a fast pace and decidedly unpredictable nature to the work, he told BusinessWest, noting that each day, and each hour, are different from the one before and the one after. But there are many more reasons why he has chosen to spend his career in this setting, the most important being the ER’s important role, both to the hospital in question and to the community it serves.
“The emergency room is the safety net for all patients,” Shukla explained. “Many patients do not have access to healthcare; we feel that the ER can provide care to anyone who walks through the door, regardless of whether you have insurance, regardless of your background; we’ll see anyone who walks through our doors, and I’m proud to say that.”
But Shukla has done more than work in the ER. Indeed, throughout his career he has devoted time and energy to bringing new efficiencies, better ways of serving patients, and, yes, better ways of doing business to the ER, especially in his current role as chief of the Emergency Department at Baystate Noble Hospital in Westfield.
And he brings what would be considered a somewhat unique background to this assignment. In addition to his undergraduate degree from the University of Missouri and his medical degree from Manpial University in Karnatka, India, Shukla also earned an MBA, with an emphasis in medical management, from UMass Amherst in 2017.
He has used all these degrees, as well as his hands-on experience in the ER, to help improve service, efficiency, and quality, and reduce wait times and what are known as ‘walkouts’ — people who come to the ER but leave before being seen, for whatever reason.
“Having earned that MBA, I was able to reconfigure how I look at things in my brain. Before, it was all medicine-related, but by doing the MBA, I was able to focus on flow and how we could improve certain processes to make an impact on the total visit.”
“Having earned that MBA, I was able to reconfigure how I look at things in my brain,” he told BusnessWest. “Before, it was all medicine-related, but by doing the MBA, I was able to focus on flow and how we could improve certain processes to make an impact on the total visit.
“At Baystate Noble, we do small thinks like put a greeter in the waiting room so when patients come in there’s someone they can talk to, someone they ask questions to; they round, they give patients blankets or small things just to make them feel appreciated,” he went on. “We also strive to push our nurses and docs to really bring patients in when they come into the ER; they don’t sit very long in the waiting room.”
As a result of such initiatives, Noble’s ER has made great strides during Shukla’s tenure. The unit has dramatically increased patient-satisfaction scores, for example, while also gaining certification as a geriatric ED, well-suited to serve the needs of older patients in the community.
The sum of these efforts has earned Shukla the Healthcare Heroes award in the highly competitive category known as Emerging Leader. And he is worthy of that designation, not only for his work in the ER, but also at Baystate Health (he is on the system’s board of directors), in the community (he sits on the nonprofit People’s Institute and also coaches youth soccer and baseball), and even on the ice.
Indeed, Shukla is one of the team physicians for the Springfield Thunderbirds, and was with the team through its exciting run to the Calder Cup finals last season.
He described that work as fun and rewarding — adjectives he would apply to every aspect of his work in medicine and administration.
Degrees of Improvement
Shukla was born in England and came to this country with his family in 1980. Early on, he said, his father, a professor of Pharmacology at the University of Missouri, and mother, a school teacher, impressed upon him the importance of not only education, but service to the community.
He achieved both while serving as a volunteer at the University of Missouri Hospital and Clinics while in junior high school, work he described as a learning experience on many levels.
“During the summer, I went there every Tuesday and Wednesday and spent eight hours each day volunteering in different parts of the hospital,” he recalled. “It was then that I realized that this was my true calling because I really wanted to help people and really wanted to make a difference.”
After graduating from medical school, he became a resident at Baystate Medical Center with a focus initially on general surgery. But at the advice of some friends who implored him to consider emergency medicine because he seemed a natural for that kind of work, his career outlook began to shift.

Dr. Sundeep Shukla, seen here with his son, Deven, is one of the team physicians for the Springfield Thunderbirds, one of the many ways he is involved in the community.
“I did some shadowing, I did some shifts in the ER, and eventually I went through the process of applying to be an ER resident,” he said, adding that he quickly fell in love with that setting — again, not just because of the fast pace and each-day-is-different aspect of the work.
“Not everyone has access to healthcare, and I’m a big proponent of health equity because I feel everyone should have the same access to healthcare as your next-door neighbor,” said Shukla, who, before coming to Noble, served as associate medical director in the Emergency Department at Baystate Franklin Medical Center. “When patients some come to my ER, I treat them with respect, I treat them exactly how I’d want to treat my family members, and I try to everything I can to make sure their health is better when they leave the ER.”
Elaborating, he said many people are coming to the ER on the worst day of their life, whether they’re having a stroke, a heart attack, or other medical problem, and it is the job of the ER doctor to “step up and help those patients.”
“It’s our goal to help lift them up and help them feel better,” he went on. “And in terms of mindset, you have to be able to function on the go and multi-task many different things, because there so many problems that are detail-oriented: the lab or CT scan, whether you have to stitch someone up, give different medications … there are all these processes you have to follow, and with every visit, there’s quality involved, and you have to meet certain metrics.”
Despite the fast pace and the constant flow of new patients, Shukla said he makes it a priority to truly connect with his patients.
“I always try to make a connection with my patients because, if I’m able to make that connection, whether it’s with a sports team that they like or a restaurant that they enjoy or some type of hobby they like, I feel like we can relate much better, and they can trust me. They just met me just a few minutes ago, so it’s really important that I build a trust and a relationship with them so that when I give them advice or we have what’s called ‘shared decision making,’ we can come with a good plan together. That’s why I’ll always spend the extra minute just to know them a little better.”
“They just met me just a few minutes ago, so it’s really important that I build a trust and a relationship with them so that when I give them advice or we have what’s called ‘shared decision making,’ we can come with a good plan together. That’s why I’ll always spend the extra minute just to know them a little better.”
Shukla currently works at all the hospitals in the Baystate system — Baystate Medical Center, Baystate Wing, and Baystate Noble — and became chief of the ER at Noble in March 2020, just as the pandemic was reaching Western Mass.
In each setting, and especially at Noble, he has been consumed with not only treating patients and making those important connections, but improving the overall experience.
“We try to look at the entire process — from when a patient walks into the waiting room all the way to when they go home,” he explained, adding that little things, such as having a greeter in the ER and having nurses, doctors, and other care providers working collaboratively so that patients don’t have to repeat their history and answer the same questions over and over again, often add up to big improvements in service, patient-satisfaction ratings, and statistics such as those concerning walkouts.
“The most dreaded word that most people see in emergency medicine is walkouts, which is basically a person who registered but wasn’t actually seen,” Shukla said. “That’s a problem throughout the United States, so we work really hard in the Baystate Health system to bring those numbers down. Even one patient walking out troubles us.”
Meanwhile, throughout his career, and even more so during COVID, he has put considerable emphasis on outreach and educating the community, with the goal of helping people make better, smarter choices about their health and well-being.
Indeed, he’s a frequent guest on area radio stations and has penned articles for several media outlets, all with the goal of creating a better-informed community.
“If people are educated, they can take care if their health better,” he said, adding that such efforts took on greater importance during the height of the pandemic, when the public had more questions — and needed more answers — and trust was a huge factor.
“We had a lot of COVID issues to contend with, but we also had to build up trust in the community,” he said, “because a lot of people were concerned about the ways people were contracting COVID, how they would protect themselves, the vaccines … there were many thongs we had to educate people on, and we did a lot of outreach for that.”
ERing on the Side of Caution
Overall, Shukla, as chief of the ER, assumes a role that blends medicine with administration, and, with his background and MBA training, he can bring a unique perspective to the table.
“Not many physicians go back and get a degree like an MBA; most of us go to school for a very long time as physicians, so not a lot of us go back,” he explained, adding that he enjoys both sides of the equation — business and especially medicine.
“It’s important for me to be well-rounded and understand how things are run,” he said, adding that he took a marketing class in 10th grade and since then has always been fascinated by business and management. “I really enjoy business, and so there’s the budget/financial aspect that I really like in administration, because I feel I can look at spreadsheets and Excel sheets in a different way than I did a few years ago before I earned my MBA.
“I understand the budget and the finances a lot more than I used to,” he went on, “and also how I can cut costs and improve efficiency in the ER, whether it’s flow in the ER or how I can reduce the cost of staffing or increase staffing to help show a return on investment.”
Going all the way back to when he was volunteering at the University of Missouri Hospital as a junior-high student, Sunny Shulka has known that he was destined to be in a profession — and a place — where he could help people.
That profession turned out to be healthcare, and the place is the ER, or the safety net, as he called it, which is now more his home.
For his efforts to continually improve that safety net, make it stronger, more welcoming, more comfortable, and better able to serve all those who come through its doors, Shukla is certainly an emerging leader, and truly a Healthcare Hero.
George O’Brien can be reached at [email protected]
Chief Operating Officer, MiraVista Behavioral Health Center
This COO Empowers Team Members and Leads by Example

Leah Martin Photography
Mark Paglia was a wrestler at Cathedral High School and later at American International College.
He said the great thing about wrestling is there is “no one-size-fits-all method that leads to success.” But there are several qualities, traits, and habits that wrestlers possess. “They trust themselves and count on their teams to train together to get better. They aren’t afraid to try new things. They are disciplined, grateful, focused, detailed-oriented, and able to adjust.”
These are qualities, Paglia told BusinessWest, that positioned him well for his current role as chief operating officer at MiraVista Behavioral Health Center, and the myriad challenges that have come with that assignment.
While working for Mercy Medical Center and its parent company, Trinity Health Of New England, Paglia served in several different roles, including executive director of Behavioral Health. He would sum up his tenure this way:
“I became the ‘project guy,’ the ‘turn-around guy,’ where I would be asked to go into departments or services that were really struggling both from a regulatory side or the financial side and turn them around,’” he said.
He was given a number of difficult assignments in that vein, such as leading efforts which led to the successful redesign of the methadone maintenance treatment program, resulting in two-year licensure with the Department of Public Health; leading efforts to open the new Clinical Stabilization Services unit; stabilizing redesign throughput for behavioral-health patients in Mercy’s emergency room; and leading the Outpatient department from a state of uncertainty to being fully licensed and financially viable. Ultimately, he was charged with winding down behavioral-health services at Providence Behavioral Health Hospital when Trinity Health Of New England made the difficult decision to close them in 2020.
As noted, these experiences, including his wrestling prowess, helped steel him for what has been his most stern career challenge, but also the most rewarding one: opening a new behavioral-health hospital, MiraVista, at the Providence Hospital site in April 2021 — in very little time, in the middle of a pandemic, in the midst of a nationwide nursing shortage and general workforce crisis, and at a time when the need for behavioral-health services was soaring due to COVID and the many ways it impacted people of all ages.
“I really find myself leading from behind, where I screen, recruit, and hire exceptional people, identify what the goals of the organization are, invite the individuals to participate, and identify what their passions are — what they believe in — and then empower them to go.”
But his efforts to open MiraVista’s doors under such difficult circumstances and then put it on a path to accreditation and expansion of both inpatient and outpatient services only partly explains why Paglia has been chosen as a Healthcare Hero for 2022 in the Health/Wellness Administrator category.
Another key consideration is the manner in which he manages — and has managed throughout his career.
He calls it ‘invitational leadership,’ which, as that name suggests, aims to ‘invite’ employees and all other stakeholders to succeed. It involves sending positive messages to people, making them feel valued, able, responsible, and worthwhile.
“I identify goals for the organization and goals for the various departments, and then invite the individuals responsible for that work to participate and own the work,” he said while explaining what this practice means to him. “Through that, I really find myself leading from behind, where I screen, recruit, and hire exceptional people, identify what the goals of the organization are, invite the individuals to participate, and identify what their passions are — what they believe in — and then empower them to go.”
Summarizing thoughts expressed by team members at MiraVista, Erin Daley, chief Nursing officer and herself a Healthcare Hero in the Emerging Leader category in 2017, wrote in her nomination of Paglia:
“His impact is garnered through his compassionate and inclusive leadership of clinical and operations teams; we find Mark, more often than not, behind the scenes working with the team and individual staff members to make them as effective and productive as they can be. Universally, team members remarked that Mark inspires them to do their best work for patients and for each other because he makes them feel their contribution is valued and an essential part of the process. Simply put, he listens. He engages people and integrates ideas, and this is what distinguishes him as a hero; his impact has longevity and grows exponentially through others.”
Such sentiments explain why Paglia will be taking the stage at the Log Cabin on Oct. 27 to be recognized as a Healthcare Hero. More importantly, they explain why he has emerged as a true leader within this region’s healthcare sector.
Taking the Lead
Paglia took what would be considered a non-traditional path to his current post with MiraVista.
Indeed, after earning a degree in business management at AIC, he went to work for a flat-glass manufacturing company. Along the way, he was asked to coach wrestling at Minnechaug High School, a role that made him realize how much he liked working with young people and helping them develop.

Mark Paglia, seen here with several team members at MiraVista Behavioral Health Center, practices what is known as the ‘invitational’ style of management.
That experience inspired him to go back to school to earn a teaching degree. He would eventually land a job in Connecticut working in a day-treatment program for youth with behavioral-health issues.
“I was really drawn to the kids, but I felt like I didn’t have enough time with them in the school setting,” he told BusinessWest, adding that these sentiments led to another rather sharp turn on the career path, this one taking him to a job as director of the Adolescent and Family Services Department at the Gándara Center’s main office in Springfield.
“I think that’s where I found my passion for caring for those who are in need,” he explained. “And that’s where I started to understand business management and performance management, and that’s where I learned the invitational model of empowering people; that was the foundation for my career.”
Fast-forwarding somewhat, Paglia said he spent nine years at Gándara before becoming program director for the Brightside Treatment Center, part of the Sisters of Providence Health System, in 2009, and later became director of Outpatient Services – Behavioral Health at Providence Behavioral Health Hospital, and then executive director of Behavioral Health for Mercy Medical Center and its affiliates, including Providence Behavioral Health Hospital, Brightside, and behavioral-health services on the Mercy campus.
“I’m blessed to work with some of the most passionate, committed, extraordinary leaders … it’s a joy to come to work every day.”
While he was in that role, Trinity Health Of New England made the difficult decision to close Providence Behavioral Health Hospital in early 2021, leaving a huge void in services available to the public.
Seeking to fill that void, Health Partners of New England acquired the property with GFI Partners with the intention of bringing back inpatient psychiatric services and a compliment of substance-use programming. And it turned to Paglia to get that difficult job done.
Recalling those days and, ultimately, the reopening of that facility, Paglia said the sum of his previous experiences certainly helped him overcome a number of hurdles, adding that he was essentially starting up a new business, starting with the hiring of staff.
The first priority was the methadone clinic, which served 600 patients and needed to remain open, and did, with the transition from Trinity Health Of New England to MiraVista, sister facility to TaraVista Behavioral Health Center in Devens, taking place at midnight on April 20. What followed was a ramping up to open an adult inpatient psychiatric unit, he went on, adding that this was achieved 10 days after the acquisition, with a second unit added in June, followed by a detox unit and then an adolescent inpatient psychiatric unit, a clinical stabilization service unit, and other substance-use addiction services.

From left, Mark Paglia with Erin Daley, chief Nursing officer; Erica Trudell, director of Nursing for Inpatient Behavioral Health Services & Education; and Alicia Morel, Talent Acquisition specialist.
Overall, MiraVista has expanded inpatient bed capacity from 36 at opening to 101 today. This includes 50 acute-care psychiatric beds in separate units for adults and adolescents, 30 detoxification beds in its acute-treatment unit for substance-use disorders, and 21 beds in post-detoxification for individuals transitioning to outpatient care. And it is staffing up for the opening of another unit, a substance-use program. Meanwhile, planning and preparation continue for the opening of what Paglia called the most challenging unit — a child psychiatric facility — with an anticipated opening date of February 2023.
Overall, MiraVista has gone from one employee, Paglia, to roughly 350 team members in just over 16 months — again, in the middle of a pandemic and a workforce crisis. In a word, he described this as an “extraordinary” accomplishment, adding that “we are midway through our journey to hire the very best staff to reach an expected 650 employees.”
Equally impressive, he said, is the number of visits from the Joint Commission on Healthcare Accreditation that the facility and its team have endured on its way to accreditation.
“Typically, an organization has one visit every three years for their accreditation,” he explained. “Because we had different lines in different units open at different times, we had four surprise Joint Commission visits where they did a complete audit and survey, and I’m incredibly proud that we passed all four with deeemed status, which gives us the opportunity to qualify for our CMS-contracted services with Medicare and Medicaid, which is a difficult achievement. To do all that in one year is pretty extraordinary.”
“I picked up quickly a long time ago that when someone is passionate about what they’re doing, they have their own internal motivation to be successful.”
He credits all that MiraVista has achieved to date to the team of leaders he has assembled.
“I attribute a lot of it to the leaders that we were able to bring in to create the foundation for this organization,” he told BusinessWest. “I’m blessed to work with some of the most passionate, committed, extraordinary leaders … it’s a joy to come to work every day.”
Shared Mindset
One of the goals of invitational management is to make all members of a team feel the same way, Paglia explained, adding that he strives to accomplish such sentiment through active listening, getting employees involved, inspiring them to assume a sense of ownership in the operation, and making sure those in every position know they have an active role in the success of the company.

MiraVista Behavioral Health Center is appropriately lit up for September, which is Recovery Month.
“I picked up quickly a long time ago that when someone is passionate about what they’re doing, they have their own internal motivation to be successful,” he said, adding that one of the goals for him and other leaders is to match this passion with career opportunities that will enable those individuals — and the company — to grow.
While doing all that, he also likes to bring fun into the equation. In fact, it’s a big part of the success formula.
“We plan for fun,” he said, adding that an ‘engagement committee’ he established has launched several initiatives that team members can take part in together, from a Halloween party to a recent barbecue and cornhole tournament; from an ice-cream social to fitness challenges.
The cornhole event and ‘mismatch day,’ where employees wear outfits that do not match, don’t explain why Paglia is an effective leader — or a Healthcare Hero for 2022 in the Administrator category.
But they are part of the explanation.
There are, in fact, many parts to this equation, but the result is an engaging administrator who has taken the lead at MiraVista — in every sense of that phrase.
George O’Brien can be reached at [email protected]
Director of Medical Oncology, Sister Mary Caritas Cancer Center, Mercy Medical Center
This Physician Provides a Needed Blend of Science and Humanity

Leah Martin Photography
On one wall of Dr. Philip Glynn’s office at the Sister Mary Caritas Cancer Center, sharing space with some diplomas and a few other photographs, is a framed, signed picture of Glynn standing beside Dr. Siddhartha Mukherjee, author of the Pulitzer Prize-winning The Emperor of All Maladies: A Biography of Cancer.
Glynn was instrumental in bringing Mukherjee to Springfield several years ago for a talk at CityStage, and prevailed upon the author, and fellow oncologist, for a photo that would become a treasured keepsake.
As he talked with BusinessWest about his career and being chosen as the Healthcare Hero for 2022 in the Patient/Resident/Client Care Provider category, Glynn gestured toward the photo — but really Mukherjee and his widely acclaimed book — on several occasions.
He did so to indicate everything from his great fondness for the book and general agreement its author on the progress made to date to the promise of great advancements in the future, to the fact that cancer, treating patients diagnosed with it, and providing them and their families with an all-important support system has in many ways defined his life and career.
Indeed, for more than 35 years now, Glynn has been at the forefront of cancer treatment in this region, touching the lives of several generations of area residents, and in many different ways — but mostly by providing quality of life, however it is to be defined by each patient, a subject we’ll return to later.
“It’s such a challenging balance — the human side and the science side. We are all disciplined to make sure that we stay abreast of the science side — that’s our fundamental responsibility, and it all starts with knowledge; there’s no substitute for that. How you integrate that into what patients need on a daily basis … that’s the art of it.”
While he is being honored as a Healthcare Hero in the Provider category, Glynn could be a recipient in almost every one of the others, with the notable exception of Emerging Leader, which would have been an apt description a few decades ago.
He has been an effective administrator and leader, having been instrumental in creating a comprehensive oncology program at Mercy that rivals anything that can be found in much larger cities such as Boston and New York.
Meanwhile, he has been innovative on many fronts, from the telehealth program he piloted in 2017 that allows Mercy cancer patients to get a second opinion on treatment from physicians at the Dana-Farber Cancer Institute in Boston, to his leadership role in creation of a new palliative-care unit that at Mercy that take the name of one of Glynn’s patients, the late restaurateur and serial entrepreneur Andy Yee.
He would certainly draw consideration in the Community Health and Collaboration categories for his work in this region to not only treat cancer but work in concert with others to diagnose and prevent it. And the sum of his many accomplishments would make him worthy of the Lifetime Achievement honor.
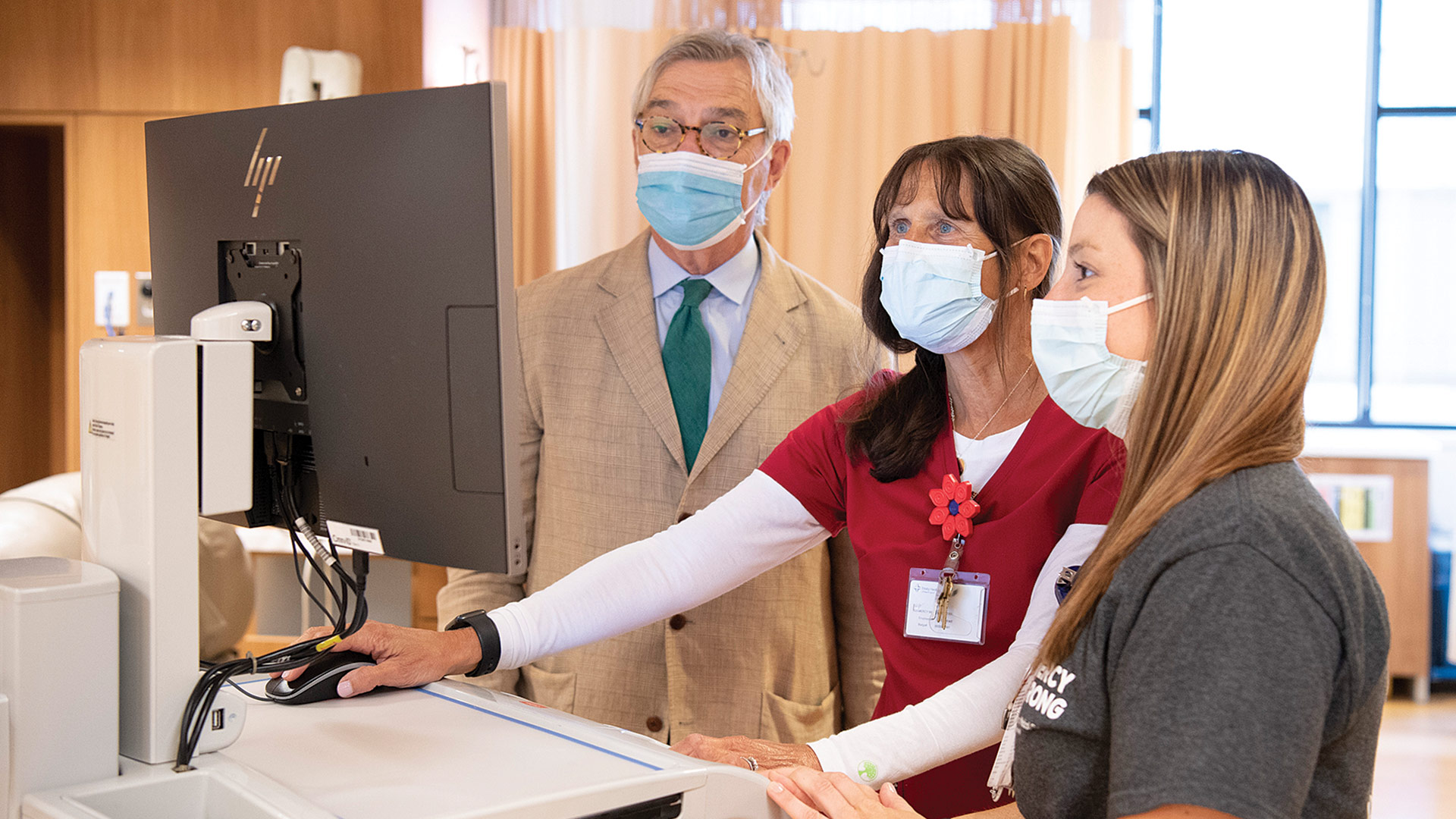
Dr. Philip Glynn, seen here with Oncology Nurse Manager Cynthia Leonard (left) and Stephanie Palange, RN, has spent his career guiding patients and their families through their cancer ‘journeys.’
But he is being honored in the Provider category because this is what Glynn, who is certified in medical oncology, palliative care and hospice, and internal medicine is perhaps most noted for — being a provider, of not only direct care, but also information, guidance, and, on many occasions, inspiration to fight the most difficult fight of one’s life.
He is described as a fierce advocate for his patients and a great listener who enables patients and their family members to be heard. Glynn said that what begins when individuals hear that they have cancer is a journey, one that often tests them in ways they could not have foreseen or imagined, and he is there with them for every step of that journey.
Overall, he described oncology as an intricate, all-important blend of science and humanity.
“It’s such a challenging balance — the human side and the science side,” he said. “We are all disciplined to make sure that we stay abreast of the science side — that’s our fundamental responsibility, and it all starts with knowledge; there’s no substitute for that. How you integrate that into what patients need on a daily basis … that’s the art of it.
“The other thing that’s really important is that you don’t give treatment for hope. You give treatment to help people live longer and better.”
“And that’s where the greatest satisfaction comes in,” he continued. “When you sit down with someone and say, ‘here’s what we’ve got, here’s the science that will take care of this disease, here’s the limits of the science for this disease’ — that communication with the patient, with the family, brings you to the point where they’re comfortable with the plan of action.”
Making patients and families comfortable, in every sense of that term, is why Glynn is certainly worthy to be called a Healthcare Hero.
A Compelling Story
As he offered BusinessWest a tour of the Caritas Center, Glynn talked with recognizable pride in his voice about what has been accomplished at that facility.
Formerly a provider of radiation treatment, it is now a true cancer center, he said, noting that it now includes a large treatment space with more than 30 infusion bays, an oncology pharmacy, laboratory space, and other facilities. Overall, the center provides care that may include cancer surgery, chemotherapy, radiation therapy, and clinical trials that provide patients with access to new treatments.
In many respects, the expansion and evolution of the cancer center is the culmination of a career spent in oncology, one that was inspired by many factors and several role models.
Early on, however, Glynn wasn’t sure if he was a good enough student or if he would work hard enough to pursue a career a health career.
Two summers working as an orderly at an Appalachian hospital in West Virginia while he was attending Boston College eventually convinced him that he did.
“The second summer I was there, I was hooked. I said, ‘this is what I want to do,’” he recalled. “It was a great experience; it all become something that I wanted to be part of.”
Glynn earned a degree in psychology at BC, attended Columbia University for pre-med, and earned his medical degree in Italy after failing to gain admission to schools in this country (and learning Italian). After residency at St. Raphael Hospital in New Haven, he completed a medical oncology fellowship at Baystate Medical Center.
Initially, he had visions of becoming a primary-care physician in a rural setting, but during residency, several role models in oncology steered him toward that specialty. He went into private practice, first in Agawam and then Springfield, while also serving as director of Medical Oncology at Noble Hospital and the Noble VNA and Hospice Service.
In 2012, he joined Mercy Medical Center and the Sister Caritas Cancer Center as director of Medical Oncology. In that role, he wears many hats and is responsible for all aspects of the program, including cancer prevention, screening, diagnosis, state-of-the-art treatment and services, counseling, and rehabilitation. He also assists with the implementation of new initiatives, such as cancer survivorship, navigation, community outreach, and clinical research and clinical-trial participation.
He is also a provider, seeing 20 patients a day on average and guiding them through their own individual journey that generally begins with three basic questions regarding their cancer: ‘what is it?’ ‘how much is there?’ and ‘what are you going to do about it?’”
Obviously, the answer to that last question has changed most profoundly over the course of his career.
“I couldn’t have imagined it when I started; it’s changed that much,” Glynn said, gesturing toward the picture on the wall and how Mukherjee had carefully and effectively chronicled the advancements. “Seventy years ago, we did gruesome surgery, and then we had gruesome surgery with radiation, and then you added in chemotherapy. But now we’ve learned about cell biology and what drives cancer cells, so we look at genes, potential immunotherapy, a host of options; it’s absolutely exceptional.”
His ultimate goal is to bring to each patient an improved quality of life, which, as noted, varies with each case.
“If you come in, an oncologist sits down, describes to you what you have, and says, ‘this is not a curable disease; this is lung cancer that has spread to the bone,’ or ‘this is colorectal cancer that has gone to multiple different organs; you do not have a curable disease. Then, what becomes critically important is to give a treatment that is going to ideally shrink the tumor and help someone live longer and better,” he explained. “You need to avoid treatments that are going to make the treatment worse than the disease. Someone may come in with bad disease, but they’re not terribly symptomatic with it … you don’t want to give them a treatment that’s going to be terribly debilitating if you can’t give them some kind of promise that they’re going to live longer from it.
“On the other hand, if you take the other end of the spectrum, the 22-year-old kid with an advanced testicular cancer … that kind can be cured,” he went on. “You have the conversation with him and say, ‘look, the next several months are going to be hell, but you’re going to get through it, and you’re walking away. That quality of life is a quality of life you’re giving a promise to — ‘you’re going to be OK,’ as opposed to the quality of life of ‘this isn’t curable, but we’re going to make sure you’re as comfortable as you possibly can be.
“The other thing that’s really important is that you don’t give treatment for hope,” Glynn continued. “You give treatment to help people live longer and better.” All this brings him back to that integration of humanity and science that he spoke of earlier, a balance, he said, which is at the very heart of effective oncology care.
There are many aspects to this equation, he added, with one of the most important, and sometimes the challenging, being communication and providing information.
“And there are times when it gets really hard,” he explained. “We live in a world that’s packed with information. Some of it’s good, and some of it’s not so good. Patients come in with very unrealistic expectations, and that becomes a very challenging conversation.”
For that reason, he brings patients to his office, positions them in front of his computer, and directs them to websites he considers reliable, with much of the rest he described as ‘storytelling.’
He said patients — and, often, family members — want and need to know about everything from prognosis to the toxicity of treatments; from their therapeutic options to recovery time and what recovery will be like.
“But it’s also important to let them know that we’re going to have a support system there for them,” he explained. “There is going to be a doctor available 24/7.”
Throughout his career, Glynn has been that doctor, there for early-morning and late-night phone calls to make sure patients are heard, and staying with them often well beyond the end of treatment, regardless of outcome.
The Plot Thickens
Returning once again to the photo on wall, Glynn said he believes the best message of that book is the promise of the future.
“He [Mukherjee] says that we probably won’t cure cancer, and I find that sensible,” Glynn noted. “After all, we don’t cure diabetes, we don’t cure heart disease, and we won’t cure cancer.”
But there will be new advancements, new and better ways of screening, preventing, and treating the emperor of all maladies, he said, adding that, while his career is winding toward its conclusion, the oncologists who follow him will have new, previously unimagined tools with which to carry on the fight.
And they can certainly draw inspiration from him.
Glynn may not have written the definitive biography of cancer, but he has authored a remarkable career, one marked by treating patients with respect and dignity, handling the heavy burden of their care with grace and humility, and providing that critical blend of science and humanity.
And that makes him more of than worthy of the title Healthcare Hero.
George O’Brien can be reached at [email protected]
Division Chief, General Medicine and Community Health, Baystate Health
He Convened a Broad, Effective, Street-level Response to a Pandemic

Leah Martin Photography
From his years working at a VA hospital in Rhode Island to his more recent community-health role overseeing Baystate Health’s medical practices in Springfield, Dr. Paul Pirraglia has always seen himself as a problem solver.
“It’s gratifying to take care of a patient and get a problem solved, or at least controlled for them — when you can address a concern that is having an impact, not just around a health issue, but in a broader sort of way,” he said. “Take a patient who has diabetes. You can get their diabetes under control, but because food is such a huge part of diabetes, if you can actually get them access to good, nutritious foods, then it’s not just about the diabetes; it’s a life changer in a way.
“As medical professionals, we really want to make a difference in people’s lives,” he went on. “So it’s gratifying to be able to serve when there’s a substantive need.”
COVID-19 would certainly qualify.
Which is why Dr. Andrew Artenstein, Baystate’s chief physician executive, who spearheaded pandemic response throughout the system when COVID arrived early in 2020, asked Pirraglia and Dr. Jackie Spain, co-chief medical officer of Baystate’s BeHealthy ACO, to convene a workgroup to mitigate the impact of coronavirus on the most vulnerable patients in the community, particularly those with significant social needs.
“It was clear that traditionally underserved populations were going to get hit especially hard by this pandemic.”
The workgroup included representatives from Baystate Health and its four community health centers, Caring Health Center, the BeHealthy Partnership (a Medicaid accountable-care organization, or ACO, that includes Health New England as the insurer and Baystate Health and Caring Health Center as care sites), the Public Health Institute of Western Massachusetts, and University of Massachusetts Chan Medical School – Baystate.
The group looked at factors that could contribute to risk, such as low-income housing, where COVID cases were occurring, where ACO members lived, medical conditions were associated with worse COVID outcomes, as well as solutions such as access to pharmacies that home-deliver, food delivery, and transportation.
“On a personal level, I’m drawn to research: here’s a vexing problem; how do we solve it?” Pirraglia said, which is one reason this strategy resonated with him. “When Dr. Artenstein said we needed to do something, it was very, very early on, but it was clear that traditionally underserved populations were going to get hit especially hard by this pandemic. He said, ‘do what you need to do; I’ve got your back.’ So what Jackie and I did was convene a group which was not limited to just Baystate; we got all the leaders we needed.”
That included professionals from a wide range of offices at Baystate and beyond, from infection control to diagnostics and laboratory; from diversity, equity, and inclusion to community relations.
“We were able to pull together a multi-disciplinary group of folks who saw the importance of convening and doing this work,” Pirraglia said. “Despite the jobs they had and their schedules, we met on a weekly basis for many, many months in a row; attendance was phenomenal. That’s because people saw the need to do this.”

This Springfield Housing Authority testing event was organized by the COVID mitigation team.
The goal was to figure out the needs of the Springfield population and communicate with them in a way that was meaningful, and the work progressed rapidly.
Initially, the workgroup explored ways to protect people who were at risk, trying to catch people who had not been infected and keep them from getting infected, while identifying who was infected and making sure those around them had protection. To aid in this effort, a grant from the Community Foundation of Western Massachusetts enabled community health workers (CHWs) to supply materials such as facemasks, portable pulse oximeters to measure blood-oxygen levels, and room dividers and air mattresses so families could quarantine within their own living spaces.
“We really broke into two groups, one group more patient-facing and another group more community-facing, and then continued to meet and engage and make sure there was good crosstalk back and forth between us,” Pirraglia told BusinessWest, while stressing the importance of communication early on.
“The communication was with the community and within all the different groups that were participating in this workgroup. But we were also communicating with our community health workers, the on-the-ground folks, the ones gathering the patient needs and delivering on those needs. And the communication, I have to say, was pretty robust, in large part because people were committed to making this happen.”
The group performed geographic analysis to determine where to focus its efforts, gathering information about patient conditions in various areas so they could inform the CHWs on the ground about which areas were riskiest and who needed help, he explained.
“I can’t emphasize enough how important our community health workers were in this work. We were the coaches, but they were the players; they were the ones on the field making this happen.”
“We had to prioritize what we were doing, so communication was paramount. At our Tuesday meetings every week, we’d say, ‘this is what the maps are showing, this is what we now about pharmacy deliveries, this is what we know about food deliveries, this is what we know about the ability to reach out to people.’ We needed to make sure all the different arms knew what the others were doing so we were able to work in concert.”
Mission Accepted
In nominating him for the Healthcare Heroes award in the Collaboration category, Michael Knapik, Baystate’s vice president of Government and Community Relations, noted that Pirraglia — an attending physician who sees some of the city’s most vulnerable patients at Baystate Mason Square Neighborhood Health Center and also a professor of Medicine at UMass Chan Medical School – Baystate who teaches residents at Baystate High Street Health Center and Baystate Brightwood Health Center — has always been mission-driven.
“This became especially important as the COVID pandemic snapped into sharp focus the inequities that have been occurring in healthcare,” Knapik said. “People who were already suffering due to inequities related to their vulnerabilities — socioeconomic, racial, ethnic, and identification factors as well as medical comorbidity all contributing — were now at highest risk from COVID-19 in terms of cases, hospitalizations, and death.”
But Pirraglia himself stressed multiple times during his interview with BusinessWest that he’s not the Healthcare Hero here, not really.
“I can’t emphasize enough how important our community health workers were in this work,” he said. “We were the coaches, but they were the players; they were the ones on the field making this happen. Based on priority lists that we made for them, they were able to reach out to patients and find out what their needs were. We created a needs assessment, and then the CHWs were the ones who came up with a contact-free delivery system. COVID mitigation isn’t their primary work, but they jumped in with both feet: ‘what do you need us to do?’ If you ask me, they’re the heroes.”
As the initial surge eased and vaccines became available early in 2021, the workgroup pivoted to that effort, as vaccination delivery to traditionally underserved groups has been a challenge in a state where early allocations from the federal government were deemed insufficient to supply both mass-vaccination sites and smaller providers, Knapik noted. The rollout through a state registration site put those without access to the internet, as well as transportation to such sites, at a disadvantage.
To address this, Baystate started to vaccinate patients age 75 and older from its community health centers in lockstep with the state’s phased rollout, with staff calling patients and inviting them to get vaccinated. In all, they were able to vaccinate 650 people over the course of six weeks, many of them individuals who would have had difficulty getting to any of the state sites. Meanwhile, the workgroup used a series of webinars and other outreach programs to communicate the importance and safety of vaccines.
Pirraglia and his team prepared a lengthy article for the International Journal for Equity in Health last year called “COVID-19 Mitigation for High-risk Populations in Springfield,” detailing the workgroup’s efforts. It concluded, “our highly intentional and methodical approach to patient and community outreach with a strong geographic component has led to fruitful efforts in COVID-19 mitigation. Our patient-level outreach engages our health centers’ clinical teams, particularly community health workers, and is providing the direct benefit of material and service resources for our at-risk patients and their families. Our community efforts leveraged existing relationships and created new partnerships that continue to inform us — healthcare entities, healthcare employees, and clinical teams — so that we can grow and learn in order to authentically build trust and engagement.”
That’s not to say the group couldn’t have done some things differently, Pirraglia said. “It’s difficult because we’re not in a setting where these entities would necessarily be meeting and collaborating. So there was probably more we could have done that was broader and more in concert.
“But I feel confident that, if another crisis came, we could convene another group, or at least use the methodology we used,” he continued. “Certainly, the community outreach and patient-oriented piece of it worked really well, and we’d probably carry that forward if we had another crisis. It really was, in my mind, highly effective.”
Mission Accomplished
As noted earlier, Pirraglia has always taken a mission-based approach to care.
“What I mean by that is we take care of a traditionally underserved population with a lot of social challenges in their life,” he told BusinessWest. “These are patients who have difficulty with travel, with food, with shelter, with a lot of other issues in their lives. So just being able to deliver care is more challenging because the patients oftentimes have these other contexts to deal with. Our work has been to try to deliver the best care we can to our patients despite some of the challenges they face.”
Throw in a pandemic, and … well, you can see why we consider the effort heroic, even though Pirraglia doesn’t consider himself a hero.
“It was a really gratifying experience to have people totally on point, using their expertise in trying to figure out this really scary problem,” he said. “We learned that you can be nimble, you can be collaborative, you can tackle a really complex problem. And when you’re working on a group like this and the communication is good, the sense of mission is good, and there’s clarity about where we’re going with it, great things can happen.”
Joseph Bednar can be reached at [email protected]
Health and Human Services Commissioner, City of Springfield
Public Health Has Become Her Life’s Work

Leah Martin Photography
When then-Mayor Michael Albano invited her to take on the considerable challenge of directing Springfield’s Health Department and Human Services Department as one entity and oversee that consolidation effort, Helen Caulton-Harris was caught somewhat off guard.
She didn’t know Albano, was not active in his campaign for the corner office, and was not expecting any invitations to join his administration.
So when the request came, she had to think about it for a while, but eventually said ‘yes.’ But certainly not with the expectation that 26 years and two mayors (including the current office holder, Domenic Sarno, who has had the job for 14 years) later, she would still have that title on her business card.
“I certainly didn’t see this as something that I would be doing two and half decades later,” she said, adding that she has stayed in this post for several reasons, but especially because she loves not only the work, but also her ability to make a real difference in the community, and also because there is still considerable work to do.
And there are always new and different challenges to meet, not the least of which is the COVID-19 pandemic, which has tested Caulton-Harris and her department in every way imaginable. It has also been a learning experience on many different levels, as we’ll see, and one that has provided some valuable lessons on how things can be done better and more efficiently.
“The way in which our public-health community has shifted because of the pandemic is that we’ve learned to work together,” she told BusinessWest. “We understood that we had to collaborate and coordinate, and that we must share information. We’re no longer working exclusively in silos; we are working across the public-health venue.
“The way in which our public-health community has shifted because of the pandemic is that we’ve learned to work together.”
“Every two weeks, we have a session with all of our partners to talk about our outreach, lessons learned, and best practices,” she went on. “So those things are part of what has happened as far as COVID-19 is concerned — our communication strategies have become more concrete.”
Caulton-Harris is the 2022 Healthcare Hero in the prestigious Lifetime Achievement category, and she has truly accomplished quite a bit in her career, especially this current chapter.
Overall, she has been an advocate, a true believer in the power of information — she preaches education — and a leader who has taken problems head on and achieved notable progress in areas ranging from teen pregnancy to infant mortality; from care for the homeless population to policies limiting smoking in public places; from substance-use disorders to violence prevention.
There are always new challenges, she said, adding that, today, there are many that she and her department are addressing as the landscape continues to change and evolve.
“Today, we’re dealing with the legalization of marijuana; cannabis is legal, but we still need to educate people about it,” she noted. “Also, gaming and problem gambling. We also have an opioid crisis, which is different than other substance-abuse matters because of fentanyl and the cheap way in which individuals are getting their products and how it escalates and has such an impact on our young people and our communities as well.”

Helen Caulton-Harris has tackled many different public-health issues over the years, from teen pregnancy and infant mortality to violence, drugs, and HIV/AIDS. Leah Martin Photography
While there have been many accomplishments during her lengthy career, she considers the biggest to be the merger of the Health and Human Services departments into one entity.
“They should not be seen as separate — they flow together,” she said with clear conviction in her voice. “I describe public health as a social-justice movement rooted in science. And Human Services really is about social justice.”
For all that she has accomplished during her life and career, and for the manner in which she has worked to improve the health and well-being of all those living, working, and doing business in the City of Homes, Caulton-Harris is a true Healthcare Hero.
A Life’s Work
When asked if she misses the regular weekly press briefings that came to symbolize the early months of the pandemic, Caulton-Harris flashed a wide smile and said simply, “not really.”
Those briefings, which also featured Sarno; Dr. Mark Keroack, president and CEO of Baystate Health; and Dr. Robert Roose, chief administrative officer at Mercy Medical Center, were conducted to keep city residents informed about was happening and what to possibly expect next, and provide up-to-date statistics concerning cases, hospitalizations, deaths, and more.
She doesn’t miss them because they came to symbolize the very worst days of the pandemic in a city that was hit very hard by COVID. But also because, while Caulton-Harris, as noted, preaches the importance of information and education and still makes regular appearances on TV, she prefers not to be in front of the camera. Instead, she would rather be working behind the scenes, advocating of behalf of area residents and providing a voice for those who struggle to make to make their voice heard.
It has been that way since her early days in the broad realm of healthcare, working with women on the issue of reproductive health, a subject which has, to a large degree, come full circle with the recent Supreme Court vote to overturn Roe v. Wade (more on that later).
“I would talk to them about the choices as far as pregnancy, whether that was to continue the pregnancy, terminate, or adopt,” she said. “So very early on in my career, I became an advocate.”
Later, while working at what is now the Mason Square Neighborhood Health Center, she was influenced by several role models, especially African-American nurses, who showed her that there were career paths for young people like her.
“I got an opportunity to see what the possibilities were for my own career,” she said. “There were individuals from my community who were making a difference in the lives of others.”
“I did not believe it was going to go on for two and half years — we’re still dealing with the pandemic today. Early on, we thought it might be a month or two, but it continues to be a pervasive virus that we’re dealing with.”
In 1994, Caulton-Harris would become executive director of the Area Health Education Center at Springfield Technical Community College, one of six such facilities in the Commonwealth, a role that enabled her to work with young people who were interested in careers in healthcare.
“I got to mentor and nurture them in a way that was very special to me,” she said, adding that, while she was in that post, she was approached by Albano about being the first commissioner of the Department of Health and Human Services.
Recalling that conversation she had with the mayor about this opportunity that doubled as a stern challenge, she said it focused on why the departments should be merged and how that should be undertaken, but also how such a merger could help address the emerging health issues of that day.
And there were many of them, she recalled, citing a sky-high teen-pregnancy rate, an equally alarming infant-mortality rate, HIV/AIDS, violence, and drugs, among others.
And it was that conversation that prompted her to leave what was a good position and step into one that would be challenging on many levels but also one that would enable her to impact lives and make a difference in the community.
“I was not quite clear on the politics of the position,” she admitted. “For me, I filtered it with the fact that I really can make a difference in the city by putting policies in place that would stay as a foundation moving forward.”
And that is exactly what she has done.
Learning Experiences
While tackling the many challenges that impact health, Caulton-Harris and other city leaders were confronted by the pandemic, which in some ways defines her career, but also sums up her straight-on approach to issues affecting the public.
“The pandemic was something that I was not prepared for and could not have foreseen as something that I would have to deal with,” she told BusinessWest. “I don’t think anyone thought we’d be dealing with a pandemic like we did in 1918, but here we are, 100 years later, dealing with a global pandemic that was devastating the world.
“Very early on, it was clear that this was devastating — our hospitals were overrun with COVID patients; our community was devastated. The Black and Brown communities in the city of Springfield probably got hit the hardest in terms of livelihood and being able to work, so we knew that staying home from some jobs simply wasn’t an option for some people. So it was all-consuming; I lived COVID-19 education every day, and I continue to do that.”
The seriousness of the virus was one issue, Caulton-Harris went on, adding that the degree of difficulty in coping with the situation was compounded by information from state and federal agencies that was often lacking, inconsistent, and at times quite confusing.
“In the early part of the pandemic, we were told that masks were not necessary, and then we were told we needed to mask up,” she recalled. “We did not have vaccines, so education and working with the public became critical. It was my lived public-health experience that enabled me to take on the pandemic. I did not believe it was going to go on for two and half years — we’re still dealing with the pandemic today. Early on, we thought it might be a month or two, but it continues to be a pervasive virus that we’re dealing with.”
As she noted, the COVID experience, if you will, has generated improvement in how those involved in matters of public health communicate, collaborate, and work together to serve the community.
As an example, she cited the work of a collective that came to be known as the ‘VAX FORCE.’
“This was a combination of physicians, community members, researchers … there were 15 individuals who were appointed by Mayor Sarno to be part of this VAX FORCE,” she recalled. “We met to put strategies in place to be able to work with the public, and that manifested itself in vaccination clinics that we had in the North End, the South End, Mason Square, Indian Orchard, and other neighborhoods. We were very intentional about the fact that we had to meet people where they were, and we used all of the expertise of the individuals on the VAX FORCE to come up with a strategy to market and make sure we were hitting all the various communities that we needed to hit.
“That, to me, was a very important strategy, and one that we put together in a way that was different than what we would have done had we not experienced the pandemic,” she went on, adding that this will be the blueprint for how to do things moving forward.
The Next Chapter
When asked what might come next for her as she nears retirement age, Caulton-Harris opted to borrow some words used recently by tennis star Serena Williams, who eschewed the term ‘retirement,’ and instead said that she will be ‘transitioning,’ or ‘evolving.’
Caulton-Harris said she will likely be doing some of the same, noting she is working on a book, a personal history of sorts, that she started maybe a decade ago.
“It’s going to be about the journey that I’ve had, from the public-health perspective, but also the personal side,” she said. “I think it’s important to be able to talk about the experiences and let people know the human side of who we are.”
Some would say she’s already written the book, the one about how to be a true leader in public health and make a difference in the community. The one about how to be a Healthcare Hero.
George O’Brien can be reached at [email protected]
SPRINGFIELD — In the spring of 2017, Healthcare News and its sister publication, BusinessWest, created a new and exciting recognition program called Healthcare Heroes.
It was launched with the theory that there are heroes working all across this region’s wide, deep, and all-important healthcare sector, and that there was no shortage of fascinating stories to tell and individuals and groups to honor. That theory has certainly been validated.
But there are hundreds, perhaps thousands of heroes whose stories we still need to tell, especially in these times, when the COVID-19 pandemic has brought many types of heroes to the forefront. And that’s where you come in.
Nominations for the class of 2022 are due July 29, and we encourage you to get involved and help recognize someone you consider to be a hero in the community we call Western Mass. in one (or more) of these seven categories:
• Patient/Resident/Client Care Provider;
• Health/Wellness Administrator/Administration;
• Emerging Leader;
• Community Health;
• Innovation in Health/Wellness;
• Collaboration in Health/Wellness; and
• Lifetime Achievement.
Nominations can be submitted at
https://businesswest.com/healthcare-heroes/nominations/
For more information call Melissa Hallock, Marketing and Events Director, at (413) 781-8600, ext. 100, or email to [email protected]
Lifetime Achievement
President and CEO, Center for Human Development

Jim Goodwin
In His Long History with CHD, He’s Seen Plenty of Lives Changed
On more than one occasion as he spoke with BusinessWest, Jim Goodwin referred to “short-termers” — employees who, for whatever reason, don’t stay at the Center for Human Development for very long, and don’t get to see the full scope of CHD’s impact on individual lives.
And that’s unfortunate because that impact, he noted, can be slow.
“One of the positives about being here a long time is you get to see how things change,” said Goodwin, the organization’s president and CEO. “We’re not working with a group of people where you sit down and have a conversation and they come away changed. It’s a process.”
For instance, he said, “people that experience serious substance-use issues often try and fail, try and fail, try and fail, and then they make some progress. When you’ve been around a while, you know failure is part of the process, and you see the change over time.
“It’s the same thing with mental health,” he went on. “Certain things in mental health never go away. It’s like diabetes; it’s with you for life. You figure out how to cope with it, how to live with it — and that is a long, hard process.”
That process may include a combination of resources, from medications to therapy to stress-management strategies, he explained.
“When you get to see it happen over time, you see that people can learn skills, they can learn to function normally with various forms of mental illness. You see the difference in people who get services and hang in there and fight the fight and come out the other end. I’ve gotten to see a lot of people come out the other end, develop those skills, and change their lives.”
“People that experience serious substance-use issues often try and fail, try and fail, try and fail, and then they make some progress. When you’ve been around a while, you know failure is part of the process, and you see the change over time.”
In his 42 years with CHD, the last 16 as president and CEO, Goodwin has seen plenty of growth; since 2005, the agency has grown from a $48 million entity to $125 million, and from around 1,300 employees to 2,000. He sees the impact, as he noted, in those individual lives changed, but it’s the sheer number of those stories, and the scope of CHD’s work, that has earned Goodwin the title of Healthcare Hero for 2021 in the Lifetime Achievement category.
“There are a lot of things I’m proud of,” he said, trying to sum up those years. “CHD has had tremendous growth over the years. And as needs have changed, we’ve been able to change and adapt and provide services in more areas.”
Opioid use is one such growth area, he noted. “Over the years, the need for substance-use services has grown substantially, and that has required us to deliver services differently.”
Today, CHD’s services span a wide gamut, including behavioral health and addiction recovery, housing and homelessness, food insecurity, youth welfare, intellectual and developmental disability, child development and advocacy, and more.

Jim Goodwin addresses those gathered to celebrate the 2018 opening of Goodwin House.
“Jim has led CHD to step in and provide services where many others would not, including to people involved with the justice system, the homeless, people with severe mental illness or disability, and many others,” said Ben Craft, CHD’s vice president of Community Engagement, who nominated Goodwin for the award.
One recent example Craft cited is Goodwin House, a 90-day residential program providing substance-use treatment services for male teenagers. The facility and its staff work to help clients not only maintain their sobriety through proven recovery strategies, but also reconnect with their families, education, and job opportunities.
“Jim has quietly built an organization that is racially and culturally diverse and one of the region’s most highly rated employers,” Craft added, “one that has grown with the needs for its services and remained nimble and innovative to keep up with the turbulent environment in which it operates.”
Expanding on an Idea
When Goodwin considers CHD’s impact over the years, he’s quick to include the organization’s 2,000 employees as well as its clients.
“These are good jobs with good benefits that allow people to have good lives and do work that they’re proud of,” he said, noting that the broad diversity of his team reflects the makeup of CHD’s clients, most of whom access services in a geographic region spanning from Amherst and Northampton to Hartford and Waterbury, Conn.
It’s an impressive footprint for an agency born from a desire by its three founders — Bill Seretta, Kathy Townsend, and Art Bertrand — to offer community-based care. In the 1960s, Goodwin noted, community services were hard to come by, and people struggling with hunger, homelessness, or simple healthcare needs easily got lost in the system. Young people, particularly those with mental-health issues, were shuffled into state training schools that were more like prisons than centers of care.
“CHD took kids from training schools and served them in foster-care and group-home models, and started to have a lot of success,” he added. “It grew from there. These community-based models started to take off because they were so successful; then we started doing it with adults.”
Today, community-based care remains the heart and soul of CHD’s mission, but the breadth of services has expanded, with more than 80 programs that help people tackle some of life’s toughest problems — often in ways that other agencies hadn’t considered.
“We provide a combination of different types of services,” Goodwin said. “Many can be identified as a mental-health problem or a substance-use problem, but it’s often tied in with other things, especially all the things associated with poverty, joblessness, and homelessness. Many times, especially in the past, agencies would take on one component or the other; they might provide homelessness services or mental-health services. But we’ve been able to combine lots of different services to create a bigger package that does the full scope of things.”
It’s those connections — recognizing the role of social determinants of health and tackling the root causes of issues — that sets CHD apart, but it’s not easy work, Goodwin said. “Some days, it can be very difficult, but when you look at the whole picture, most days I’m really glad we’ve taken all that on.”
It also cultivates an organization with career mobility, he added, as employees can move around and take on different roles as they gain experience in other fields. “One of the good things about CHD is you don’t have to leave to try something new.”
But those connections between clinical and non-clinical supports poses a constant challenge to come up with new ideas and approaches, he added. “You have to be creative.”
Take, for example, Innovative Care Partners (ICP), which is a collaboration between CHD (the managing partner), Gándara Center, and ServiceNet designed to better serve clients in the MassHealth program for their behavioral-health needs. ICP’s care coordinators connect clients with other members of the healthcare-delivery system, including hospitals, primary care, and other providers, across the four Western Mass. counties to help ensure they’re getting needed services without duplication or inefficiencies.
“We get people to follow a set of services that speaks to their behavioral-health needs,” he said, which might include medication, psychiatry, or counseling, but the program also focuses on the factors that get people into health trouble, such as poor nutrition, high levels of anxiety and stress, and high blood pressure.
“Together, primary-care health professionals sign off on a comprehensive plan that speaks to the full range of their needs,” Goodwin explained. “That’s a change. There used to be walls between mental-health services and medical services. Everybody knew that didn’t make any sense, but until recently, it never became a focus of attention.”
Learning Experiences
Needless to say, the Center for Human Development has had a challenging 18 months navigating the COVID-19 pandemic. With 850 residential mental-health beds and thousands of clients accessing outpatient care, there was plenty of learning on the fly — especially when it came to telehealth — but everyone came through to continue meeting the needs that drew Goodwin to CHD 42 years ago, and plenty of others.
“We’re proud of our impact, and that includes our economic impact,” he said. “We provide local jobs, and our people are spending money in their local communities, buying homes … a lot of things are happening because they’re here and CHD is paying them. I think we contribute to the economy in a big way.”
But the main impact remains those individual lives that are changed — albeit sometimes very slowly.
“My goal from the very beginning was to have an agency people would be proud to work for and feel good about what they’re doing,” he said, admitting that the work can be tough, navigating thorny issues like homelessness, drug addiction, and young people in trouble with the law.
“That can be very difficult for the workforce,” he added. “But overall, it’s also very rewarding. It’s the type of work you can be proud of and see accomplishment.”
Joseph Bednar can be reached at [email protected]
Collaboration In Health/Wellness

Collaborators in DASHH include Revitalize CDC, Baystate Health, Health New England, the BeHealthy Partnership, Holyoke Medical Center, the Public Health Institute of Western Massachusetts, the Pioneer Valley Asthma Coalition, and the Green & Healthy Homes Initiative.
This Coalition Keeps People Healthy in Ways Its Partners Couldn’t Achieve Alone
If there’s anyone who understands the impact of asthma in Greater Springfield, it’s Sarita Hudson.
Specifically, as director of programs and development for the Public Health Institute of Western Massachusetts and manager of the Pioneer Valley Asthma Coalition, she understands the connections between one’s physical environment and health — and the factors that have consistently placed Springfield high on lists of riskiest places to live with asthma. But even the Asthma Coalition has its limits.
“We had been doing asthma interventions, working with community health workers, working with clients, doing education, helping them identify triggers,” she said. “But it’s not enough if we can’t actually fix anything in the home.”
Meanwhile, as vice president of Public Health for Baystate Health, Frank Robinson understands the many ways the system’s community health programs and providers promote preventive health and wellness.
“We had been doing asthma interventions, working with community health workers, working with clients, doing education, helping them identify triggers. But it’s not enough if we can’t actually fix anything in the home.”
Still, “Baystate would never be going out and creating healthy homes by doing environmental changes and mitigations,” he explained. “That is not the work of the healthcare system. To be aligned with someone who does that work and gets the health implications and health impacts is perfect, though — it makes a perfect marriage.”
That organization would be Revitalize Community Development Corp. (CDC), which does have a long history of making critical repairs, modifications, and rehabilitation on the homes of low-income families with children, military veterans, the elderly, and people with disabilities.
When these three organizations started talking — about asthma and other issues — they were intrigued by what they might accomplish by working together, said Revitalize CDC President and CEO Colleen Loveless.
“We’d been doing some of this work — mold remediation, pest control — but hadn’t formalized the process in collaboration with insurance companies and the healthcare system,” she told BusinessWest.
Now, thanks to a collaboration called Doorway to an Accessible, Safe and Healthy Home (DASHH), these three organizations are not only identifying families in need of intervention for environmental health issues, and not just educating them on lifestyle changes, but actually making the necessary physical changes to their homes.
“We started talking, and we applied for a technical-assistance grant from the Green & Healthy Homes Initiative in Baltimore. They’ve been doing this work for decades,” Loveless explained. “We were one of five sites awarded that technical-assistance grant.”
Baystate followed with a capacity-building grant, other state grants followed, and DASHH was in business. Since its beginning in 2015, the program has served 130 households with asthma remediation and education, as well as 101 households for age-in-place modifications. Last year, it launched a COVID-19 response project (more on that later), impacting more than 1,550 households and approximately 6,881 individuals.
“It’s a business model that shows that, by intervening and creating healthy homes through environmental remediation, removing asthma triggers, and improving the physical environment, we could reduce asthma incidence in high-risk populations,” Robinson said.
Families referred by Baystate for environmental interventions receive three to five visits to conduct testing, at the start and end of the process, and provide education on how to keep the home clean and safe. If needed, Revitalize CDC brings in services ranging from air-duct cleaning to mold remediation; from pest control to floor covering and replacement, and also provides air purifiers, HEPA vacuums, and cleaning supplies.

By partnering with health-centric organizations, Colleen Loveless (center) and Revitalize CDC were able to infuse home-rehab efforts with a focus on wellness.
“The goal is to keep people from having to access primary care or the emergency room, and not miss school or work,” Loveless said. “Asthma has such a ripple effect.”
Better Together
The initial goal of DASHH was to help older people by improving their housing conditions related to asthma and falls, most notably by providing home assessments and home repairs to help them stay healthy and age in place. Breaking down this enterprise that has earned the title of Healthcare Hero for 2021 in the Collaboration category, the individual honorees are:
• Revitalize CDC; which performs assessments and interventions for adults and children with asthma and COPD and makes safety modifications and aging-in-place improvements so seniors may safely remain in their home;
• The Public Health Institute of Western Massachusetts, which provides support on asthma issues; measurement evaluation; support and coordination for referrals, education, and outreach; coordination and support for asthma home-visiting services; and technical assistance and support, as well as providing materials and services in Spanish;
• Baystate Health and the BeHealthy Partnership (a MassHealth accountable-care partnership plan option made up of the Baystate Health Care Alliance and Health New England), which provide referrals to DASHH through five health centers: Baystate General Pediatrics at High Street, Brightwood Health Center, Caring Health Center, High Street Health Center Adult Medicine, and Mason Square Neighborhood Health Center; and
• The Green & Healthy Homes Initiative, a national network that provides technical assistance on planning, database services, and access to best-practice strategies. The organization worked with the other partners on feasibility studies to come up with ways to fund interventions in the home and determine how those efforts might impact healthcare costs and decrease healthcare utilizations regionally.
After its initial success with Baystate, Revitalize CDC expanded its service area in 2019 to begin collaborating with Holyoke Medical Center and its team of community health workers and navigators. To boost such efforts, the city of Holyoke recently awarded Revitalize CDC’s Healthy Homes Program $100,000 from American Rescue Plan Act funds.
DASHH serves low-income families in Hampden County, which ranks last among the Commonwealth’s 14 counties for health outcomes and health factors for racial/ethnic groups. Springfield had been the asthma capital of the U.S., according to the Asthma and Allergy Foundation, until 2019, and now ranks 12th — still not the most desirable ranking, but an improvement, to be sure.
“You talk to the families, and you see that this is the kind of impact that changes their health,” Hudson said of DASHH’s efforts. “It means they can breathe easier and get the supplies they need.”
For instance, in some cases, “the ventilation ducts have never been cleaned, and every time the heat comes on, they have an asthma attack. Now they’re clean, and it doesn’t happen,” she went on. “Some of these are small, simple repairs.”
This issue has been important to Hudson for a long time, through the Pioneer Valley Asthma Coalition, which was formed 15 years ago to address childhood asthma by improving medical and self-management of the condition, as well as by reducing environmental triggers.
The coalition focuses on outdoor air pollution and indoor air quality and has successfully advocated for new policies, including statewide regulations to prohibit tobacco sales to those under 21; green cleaning policies and procedures adopted by Holyoke Public Schools; an ordinance against burning construction and demolition debris; and asthma protocols and an idle-free vehicle policy adopted by Springfield Public Schools, among many other successes.
It’s work — not just the physical interventions, but education of homeowners, landlords, and primary-care physicians — that should be happening on a wider scale, Hudson said, not just in homes, but in schools and other older buildings where people gather.
“We really see a lot of our housing stock as old, with deferred maintenance, including so much of our rental housing. That’s why we are pleased to see more funding around whole-house renovations.”
Quick Pivot
Last year, the DASHH coalition began supporting patients at risk of contracting COVID-19 by providing them with essential supplies and access to nutritious food at home. It made contactless deliveries that also included COVID-prevention supplies, including disinfectants, microfiber cleaning cloths, cleaning gloves, dish detergent, food-storage containers, hand soap, disinfectant wipes, paper towels, and food from local pantries.
“These are people who were quarantining, and we were providing them with cleaning supplies, hand sanitizer, and facemasks — and we found many were food-insecure, so they were provided food from local food pantries,” Loveless said. “The whole DASHH program just expanded from asthma to COVID, and we’re still seeing it now.”
Meanwhile, she’s excited about seeing the coalition continue its broader work — and those regional asthma statistics improve further.
“It’s been a really, really great partnership. It’s a win-win situation — the healthcare system saves money, we’re serving more low-income families in need, and patients are healthier. So it’s really a win-win-win.”
Robinson agrees. “I think the role of Revitalize and other housing providers that understand these issues have made a difference — and make healthcare providers’ jobs much easier,” he said. “They have been instrumental partners in creating safe and healthy houses for older adults as well as creating healthy homes for folks with respiratory diseases, asthma in particular.”
The work is both deeply collaborative and, dare we say, heroic.
“I’m so appreciative,” Loveless said. “Together, we’re able to serve more people in need.”
Joseph Bednar can be reached at [email protected]
Innovation In Health/Wellness
Director of LGBTQ Services, Cooley Dickinson Hospital

J. Aleah Nesteby
She Pioneered Appropriate Care for a Population That Sometimes Lacks It
By Mark Morris
Healthcare was Aleah Nesteby’s second career goal.
“My first career goal was to be a standup comic, but I eventually realized I didn’t have the stomach for all the rejection that involved,” she said.
As it turned out, comedy’s loss was healthcare’s gain. For the past several years, she has been a family nurse practitioner and director of LGBTQ Health Services at Cooley Dickinson Health Care — and is now beginning a new career at Transhealth Northampton.
In doing so, she will continue her pioneering work providing culturally sensitive healthcare for often-marginalized populations — work that many health organizations have since adopted, long after Nesteby became an early pioneer in this region — and a true Healthcare Hero.
“I thought, if my friends can’t access good care in San Francisco, is there anywhere they can? I also thought, well, I could do that.”
According to the Centers for Disease Control and Prevention, members of the LGBTQ community face an increased risk of health threats due to discrimination and stigma. In her role with Cooley Dickinson, Nesteby has worked to bring more equity and compassion to healthcare for the LGBTQ community. As a practitioner, she has maintained a patient panel of about 500 people, many of whom are transgender.
It’s a passion that predates her medical career, to be sure. Since college, Nesteby has had an interest in healthcare among marginalized populations, but at the time, care focused specifically on LGBTQ people didn’t exist. In the early 2000s, while in San Francisco, she learned that some of her LGBTQ friends were not able to access healthcare.
“I thought, if my friends can’t access good care in San Francisco, is there anywhere they can?” she said. “I also thought, well, I could do that.”
So she did. And for her years of cutting-edge advocacy for this broad and sometimes misunderstood population, Nesteby certainly merits recognition in the category of Innovation in Healthcare.
Training Ground
In addition to treating patients, Nesteby’s responsibilities include training providers and staff on how to make medical facilities more welcoming and inclusive.
Much of the training I would call LGBTQ 101,” she said. “It’s a discussion on how to treat people respectfully and how to engage them in language they would like you to use.”

After years of pioneering work at Cooley Dickinson, Aleah Nesteby is taking her passion and talents to Transhealth Northampton.
One common question — she’s heard it countless times — challenges why LGBTQ patients should be treated differently than anyone else. She explains that everyone has unconscious biases that play into their decisions about treatment for people.
“I try to help providers understand that, even though they think they are treating everyone the same, some of what they are saying isn’t being received by the patient in the way it might have been intended.”
For instance, microaggressions are a common issue — those backhanded compliments and minor comments that might not be insults, per se, but add up in a negative way to the person who hears them. A gay or lesbian person might be told, “I couldn’t tell whether you were gay or straight,” and a transgender person might be asked what their old name was.
“It’s these low-level, unpleasant interactions that many medical folks aren’t even aware they are doing,” Nesteby said, emphasizing that training should include all employees in the medical setting, not just direct care providers. For example, a visitor to the doctor’s office typically first speaks with someone on the front desk, then a medical assistant or nurse, and, finally, with the physician or nurse practitioner.
“Even when all the providers are trained and great to be around, if the staff aren’t trained, it can still be a negative experience for some,” she explained.
Nesteby also helps providers with more detailed training that addresses health issues specific to the LGBTQ community, such as hormone therapy for transgender adults and working with transgender children.
“I’ve also trained doctors on PrEP, a pre-exposure prophylaxis for HIV,” she said. “It’s a medication people can take before being exposed to HIV to help prevent transmission.”
In some ways, Nesteby has always been an LGBTQ trainer. She was studying to be a nurse practitioner back when the transgender health movement — commonly called trans health — was just beginning. Because it wasn’t included in the curriculum, she invited a lecturer to speak to her class about trans health.
“In the beginning, there were lots of things to learn and new ground to break,” she recalled.
Nesteby is now in demand as a speaker at conferences around the country, though her appearances during the pandemic have been virtual. She also participates in TransLine, an internet-based consultation service. “People can e-mail their questions about trans health to volunteers like me, and we answer them as they come in.”
As she became established and word got out that her practice included trans health, patients would travel from hundreds of miles away just to be seen by Nesteby. However, “as trans health has become a more accessible field and more providers have become comfortable with it, there’s less need for people to travel long distances.”
Continuing the Conversation
Reflecting on her work with Cooley Dickinson gives Nesteby a great deal of satisfaction. From training medical staff to policies to make the hospital more inclusive, she appreciates all the progress that’s been made so far.
“While there is still work to be done, there has been a cultural shift in Massachusetts on how we view our LGBTQ patients,” she noted.
Jeff Harness, director of Community Health and Government Relations for Cooley Dickinson, called Nesteby’s work critically important to the LGBTQ community.
“It is rare to find a primary-care provider who understands the unique health and social needs of LGBTQ patients,” Harness said. “It’s exceedingly rare to fine one who is so skilled, passionate, and caring.”
This month, Nesteby is leaving Cooley Dickinson to join Transhealth Northampton, a clinic that provides primary care for children and adults. Her role will be similar to her current one in providing primary care and hormone management for her patients. In her new position, she will continue to educate clinicians and will also focus on educating the general public about working with the LGBTQ community.
“I’m an advocate of asking people how they want to be addressed and what pronouns they use,” she said. adding that people often get nervous they might offend if they ask, but the conversation has to start somewhere. “If you are respectful and polite, people will usually respond in kind. They only get upset when someone is rude or asking for information that is gratuitous or not needed.”
In general, Nesteby would like to see a more welcoming and affirming atmosphere in medicine.
“Ideally, I’d like all providers to have some degree of knowledge about how to work with LGBTQ patients because within that there is more opportunity for people to specialize in that care.”
Harness credited Nesteby with making positive changes in the system while always providing excellent care to the person in front of her. “Aleah has improved her patients’ sense of well-being by showing them their medical provider cares about, understands, and welcomes them,” he said.
In her eyes, though, showing compassion is similar some ways to the old adage about a rising tide lifting all boats.
“If we are more open and understanding to folks in one group,” she said, “we tend to be more open and understanding to everyone — and that helps all of us.”
Health/Wellness Administrator
Medical Director, Holyoke VNA Hospice Life Care

Alicia Ross
This Administrator Has Been a Pioneer, a Mentor, and an Inspiration
By Mark Morris
Growing up in the Philippines, Alicia Ross always hoped to become a doctor. Her father, a dentist, had other plans and wanted his daughter to take over his practice.
“I didn’t want to go into dentistry, so I went into medicine,” Ross recalled. Shortly after graduating from Manila Central University and passing her medical boards, she emigrated to the U.S.
In 1971, Ross joined the staff of Holyoke Medical Center, specializing in hematology and oncology. At the time, she worked with cancer patients, with the single goal of healing them. But for patients with advanced cancers, doctors can often reach a point where there are no more treatment options. Ross understood those patients needed something else.
“It’s huge for the patient to be reassured they’ve done all they can do to fight their illness. It’s also just as important for family members because they will remember this for the rest of their lives.”
“We had to refocus our goal,” she said. “For those cases, instead of a cure, we would instead work toward comfort measures for the end of life and do our best to ease their pain.”
So began what could be called a new career for Ross, or at least a new, exhilarating, and rewarding chapter in a remarkable — and ongoing — career. In 1991, she would become the founding medical director of Holyoke VNA Hospice Life Care.
Over the past 30 years, she has changed countless lives, and not just those who come under her care. Indeed, as an administrator, she has been a leader, a mentor, and an inspiration to those she has worked with, primarily by challenging them to continuously find ways to bring comfort and, yes, quality of life to those in hospice care.
“Someone referred to Dr. Ross as a ‘pioneer,’ and I think that is a very apt term for her,” said Maureen Groden, director of Hospice and Palliative Care, adding that Ross has changed the way many think when they hear that word ‘hospice,’ and she has spent her career educating and innovating.

Alicia Ross says many people recoil at the idea of hospice without realizing what a benefit it can be.
Jennifer Martin, director of Operations and IT for Holyoke VNA Hospice Life Care, agreed.
“As medical director, Dr. Ross has always been our go-to; she is the backbone of the hospice program,” she said. “In our weekly team meetings, she goes above and beyond to make sure we provide the absolute best care for every patient and every situation.”
Those sentiments certainly help explain why Ross has been named a Healthcare Hero for 2021 in the always-competitive Administration category. Over the years, that honor has gone to those who don’t simply manage, but lead; those who not only care for those in need, but inspire others to reach higher and find ways to continually improve that care.
Ross certainly continues that tradition.
Life-changing Decisions
Getting back to that word ‘pioneer,’ it is used to describe those who break new ground and blaze a trail for those who would follow.
As Groden said, that term suits Ross because of the way she studied hospice care and adopted best practices, but also because she sought to keep raising the bar in all aspects of this field of healthcare.
Turning back the clock to the late ’80s, Ross said she traveled to England to study under Dr. Cicely Saunders, considered the founder of the modern hospice movement.
“Before we started our hospice services in Holyoke, I went to England to better understand how they did it,” she told BusinessWest. While she worked primarily with the doctor’s staff, Ross also met with and learned from Saunders herself.
Ross turned her knowledge into action in 1990, joining others in creating Holyoke VNA Hospice Life Care. They did so, she said, with a simple philosophy: that “dying is a part of living.”
With hospice care, it’s possible to bring dignity and acceptance to patients and families when they are making difficult decisions about end-of-life care. But it is never an easy conversation.
“We still see patients who have a strong negative reaction to the word ‘hospice,’” Ross said, adding that this is unfortunate because people who could benefit from hospice care are not always referred early enough to enable them to gain some benefit from it.
“In addition to nurses who provide pain relief, hospice also offers other services to make a person’s last days more comfortable,” she noted. “Home health aides, chaplains, social workers, even volunteers can all bring comfort to the patient.”
No matter what faith a person follows, she added, the chaplain’s role is part of providing comfort and pain relief. “During this time, many patients have emotional and spiritual pain. When the chaplain can reduce some of that emotional pain, it also eases some of the physical pain.”
Volunteers also play an important role. While COVID restrictions have curtailed in-person visits to patients, volunteers also make an important contribution in providing comfort.
“We try to match volunteers to the patient,” Ross said. “For example, if the patient is a veteran, our volunteer is a veteran.” By aligning interests, the volunteer becomes a welcome face and often develops a friendship with the patient.
Administering medicine is an important part of hospice, but there are often non-medical ways to ease a patient’s pain. Ross gave an example of how a patient with lung disease will regularly experience shortness of breath.
“While morphine is a good treatment, oxygen is too, so a fan blowing in the room can be very effective,” she said, adding that anxiety also contributes to difficulty in breathing. “Many patients feel they are burdening their family, so we work on lessening their stress and anxiety to help them understand they are not a burden on their family.”
According to Groden, family members often struggle and wonder if they’ve done the right thing in referring a loved one to hospice. She said Ross approaches that conversation by reassuring the family that, at this point in time, additional treatments would actually cause more harm than good, and that hospice is the most compassionate approach.
“It’s huge for the patient to be reassured they’ve done all they can do to fight their illness,” Groden said. “It’s also just as important for family members because they will remember this for the rest of their lives.”
While modern medicine can extend people’s lives, many still need hospice in their later years. Ross also pointed out that hospice is not just for the elderly. “We have a lot of illnesses that can affect relatively younger people, like Lou Gehrig’s disease, early-onset dementia, and, of course, cancer, which affects people at all ages.”
No matter the age, she noted, the goal of Hospice Life Care remains the same. “Our main purpose is to give patients comfort through the end of life, to make them as comfortable as possible, and treat their symptoms so they don’t suffer.”
After 50 years at Holyoke Medical Center, 30 of which were at Hospice Life Care, Ross has certainly seen many changes in healthcare. She listed electronic medical records and advancements in medication as two of the most significant.
While many physicians choose to retire rather than confront new technology, she took time to learn electronic medical records and embraced the advances in both technology and medicine. Her colleagues say she never misses a beat, one of the reasons she’s an effective leader and healthcare provider.
At the urging of her husband, Ross had planned to retire by 2015. But when he became ill in 2014 and passed away quickly, she decided to continue her work.
“I thought if I retired, I would only sit around the house and mourn, so a better choice was to keep working,” she said, adding that, with each life she impacts, she embraces that decision.
A True Leader
Martin observed that Holyoke VNA Hospice Life Care admits approximately 275 patients to hospice each year.
“When you multiply that number times 30 years, it gives you an idea of just how many lives Dr. Ross has touched,” she said, adding that her lasting impact is measured not in numbers, but in words, especially those used by family members of patients to describe the compassionate care they received.
Those words convey many things, including just how much of a pioneer she has been throughout her career, and how she has convinced so many that dying really is a part of living.
Mostly, though, they convey that she is a true Healthcare Hero.
Emerging Leader
Hospital Epidemiologist, Baystate Medical Center; Vice Chair for Clinical Affairs, Department of Medicine, Baystate Health
Dr. Sarah Haessler
She ‘Stands on a Wall Between the Community and Infectious Diseases’
Dr. Sarah Haessler has already been honored as a Healthcare Hero. Actually, a ‘Healthcare Superhero,’ to be more precise.
That was the unofficial title bestowed upon 76 fully vaccinated healthcare workers from across New England who attended the Super Bowl last February as guests of New England Patriots owner Robert Kraft. The group flew down on the Patriots’ team plane and got to see Tom Brady win his seventh Super Bowl — and promote vaccination while they were at it.
Haessler, hospital epidemiologist at Baystate Medical Center and vice chair for Clinical Affairs in the Department of Medicine at Baystate Health, was one of three from this region to be so honored; she was joined by Baystate colleague Stephen Boyle Sr., senior director of Hospitality; and Cherie Rodriguez, a respiratory therapist at Mercy Medical Center.
Haessler has many memories from that day, with only some of them involving the action on the field.
“It was the quintessential American experience,” she recalled, noting that healthcare workers from across the country were recognized at the game. “It was big. Everything about it was big. The music was loud, there were fireworks for everything, there were military flyovers, the jumbo screens had the president on them … America doesn’t do anything small. This was very big and very American.”
“Her role is to stand watch on the wall between our patients, our team members, our community, and the infectious agents that threaten their health. And she has successfully done this for more than a decade, not only in the face of a global pandemic the likes of which we have not experienced for more than 100 years, but every day of the year. Because in healthcare, those threats never cease.”
Haessler said pairs of tickets to the game were made available to various hospitals, and she was chosen by officials at Baystate to attend; she’s not sure how or why.
Matters are a little more clear when it comes to her being chosen as the winner in the intensely competitive Emerging Leader category for BusinessWest’s Healthcare Heroes awards. She has been chosen in large part for her many efforts to prepare those at Baystate for what was coming in early 2020 and for her ongoing work throughout the pandemic to plan, educate, and help carry out all the operations of a hospital during extraordinary circumstances. But there is certainly more to the story. Indeed, COVID-19 wasn’t her first experience with a highly infectious disease, and she acknowledged, with some resignation born from experience in her voice, that it won’t be her last.
Meanwhile, she has taken on more leadership roles over the years, serving as interim chief medical officer at Baystate Noble Hospital and currently sitting on the board of the Society of Healthcare Epidemiologists of America.
Her work in her chosen field, and her status as an emerging leader in Western Mass. and beyond, is best summed up by Dr. Andrew Artenstein, chief physician executive and chief academic officer, incident commander, COVID-19 Response, at Baystate Health, who nominated her for this honor.
“Her role is to stand watch on the wall between our patients, our team members, our community, and the infectious agents that threaten their health,” he wrote. “And she has successfully done this for more than a decade, not only in the face of a global pandemic the likes of which we have not experienced for more than 100 years, but every day of the year. Because in healthcare, those threats never cease.”
In a candid interview, Haessler talked about that harsh reality, her work at Baystate, her chosen career in epidemiology, and the many kinds of rewards that come with it.
At the Top of Her Game
When asked how she chose epidemiology as a specialty, Haessler started by saying that, during her residency at Dartmouth, she was interested — make that fascinated — by all aspects of medicine. It soon became clear to her that she needed to pick something broad that would cross all other specialties.
“When I sat down to pick one, I ultimately decided that the specialty where the cases that kept me up late or got me up early in the morning to learn more and read more and try to figure out what was wrong with this person — these puzzles — were the cases that were most interesting to me, and the most satisfying and challenging. And that was infectious disease,” she told BusinessWest.
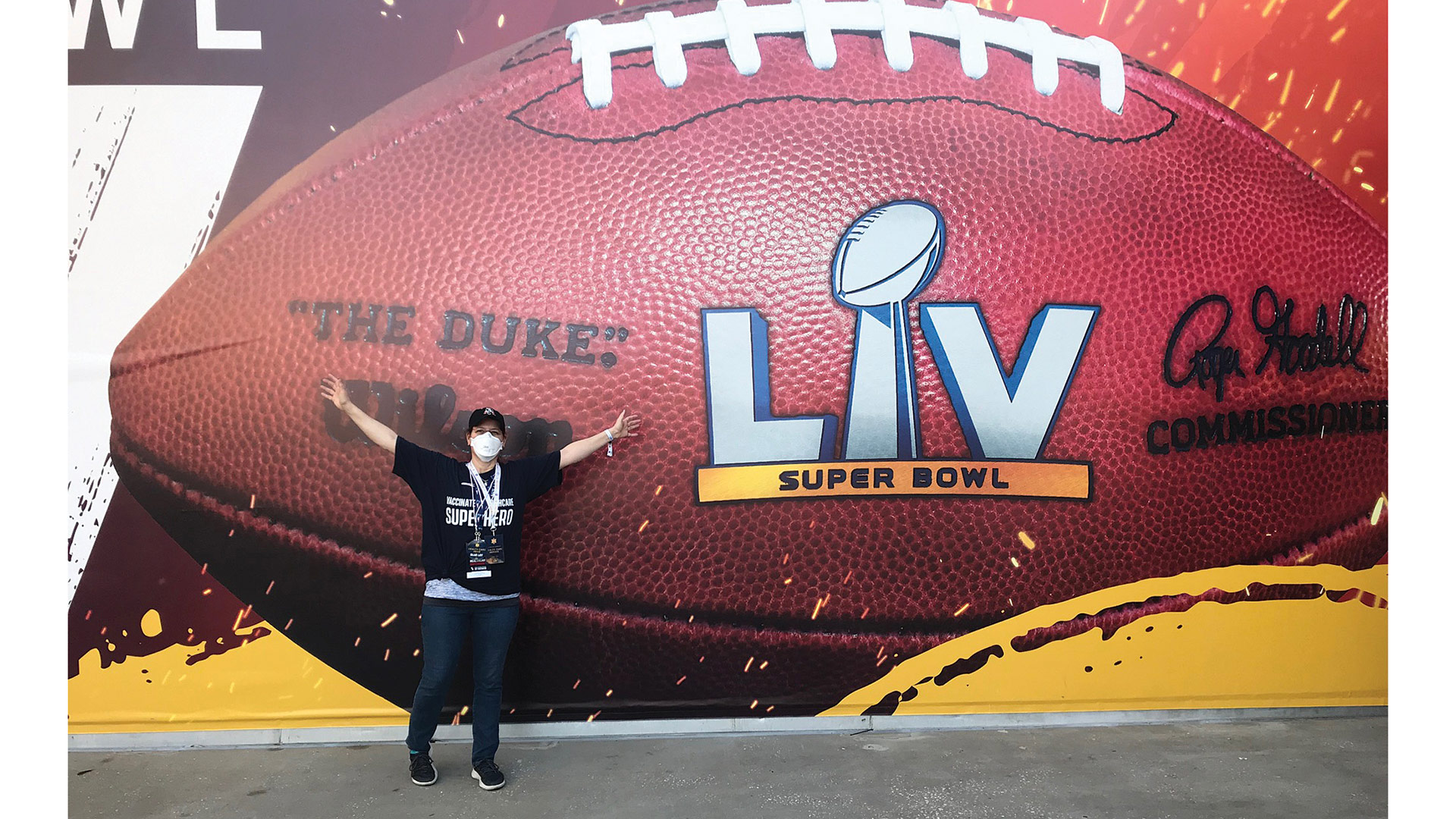
Dr. Sarah Haessler was one of many ‘Healthcare Superheroes’ in attendance at last February’s Super Bowl in Tampa.
“I’ve never looked back — I’ve always loved it,” she went on, adding that, in this field, she does get to interact with specialists of all kinds. “It’s been an interesting career — I’ve never been bored. And the other thing about it is that it just keeps moving. I’m a high-energy person — I keep moving — so it suits me very well.”
Things were certainly moving in the latter days of 2019, said Haessler, noting that the information coming to her from hospital epidemiologists in China, and later the state of Washington, made it clear that something ominous was on the horizon.
“We saw the pandemic potential for it because it was so swift and had created a huge influx of patients in those hospitals in Wuhan,” she recalled. “It essentially overwhelmed those hospitals immediately, and the fact that China’s approach was to put the area in lockdown … that is the kind of organism, like SARS, that causes a pandemic.”
She said Baystate was ready, in large part because it had gone through this before with other infectious diseases and had learned many valuable lessons. And she was at the forefront of these efforts.
“We had been through H1N1, and then we had been through the Ebola epidemic,” she explained. “And this really created an impetus, and a framework, across the United States for preparedness for the world’s most contagious diseases.”
Because of Ebola, Baystate had created a Special Pathogens Unit to manage extremely contagious patients, said Haessler, who manages this unit and the team that operates it. And as part of that team’s work, it created protocols and procedures for how it would manage patients, took steps to ensure that there would be adequate supplies of PPE, put in place scenarios for how patients would be cared for and where, determined if, when, and under what circumstances elective surgeries would be halted, and much more.
In short, as Artenstein noted in his nomination, Haessler was the point person for preparing the medical center for what everyone could see was coming.
“Her work provided great comfort to all, knowing that we had such an expert in such a key role,” he wrote. “Her team’s magnificent work in collaboration with employee health services led to the earliest possible recognition of infectious contacts and allowed us to limit the risks for patients and staff during a time of great uncertainty and fear.”
While the past tense is being used for most of these comments, the work battling COVID is obviously ongoing, said Haessler, adding that the Delta variant brings a new and very dangerous thread to this story.
When asked about what the past 18 months has been like, personally and professionally, she said, in essence, that it’s been the culmination of all her training and hard work.
“It’s been one of biggest events that I’ve had to participate in, and while it’s been challenging, it’s also been very gratifying, because Baystate has been an incredible organization, rising to the occasion in this. I’m so proud of Baystate; I’ve never been more proud to work at this organization and to be part of the leadership team.
“The responsiveness, the focus on what was important and what remains important, has been incredible,” she went on. “It’s been a laser focus on the safety of the healthcare workers, and protecting our patients and our healthcare workers from getting and passing this disease, getting the resources we needed to enable safe management of these patients, and staying really, really focused on what’s important here has been a phenomenal experience and an opportunity for tremendous personal and professional growth.”
Passing Thoughts
Returning to Raymond James Stadium and Super Bowl LV, Haessler said she had the opportunity to meet with healthcare workers from across the country who had been, at that time, battling with COVID for roughly a year.
“It was an opportunity to meet with other people, commiserate, and just be among kindred spirits — people had been through so much,” she said, adding that, seven months later, the fight continues, and in some ways, it has escalated.
In the future, there will be other fights against infectious diseases, she said, adding that the best hospitals and healthcare systems can do is try to be prepared, because, as Artenstein noted, these threats never cease.
That, in a nutshell, is what her career has been all about. Her ability to exceed in that role and many others has made her a Healthcare Hero — and a ‘superhero’ — as well as an emerging leader in Western Mass. and her chosen field.
George O’Brien can be reached at [email protected]
Patient/Resident/Client Care Provider
Doctor and Owner, DeCaro Total Foot Care Center

Dr. Louis J. DeCaro
This Specialist Has Helped Patients of All Ages Take Huge Strides
Dr. Louis J. DeCaro is firm of the opinion that no one actually has good feet.
Rather, experience tells him that everyone has one of 24 variations of bad feet.
“That includes high arches, low arches, no arches … people come in and they think flat feet are the only bad feet,” said DeCaro, owner of Hatfield-based DeCaro Total Foot Care Center, referencing a chart of what he calls the ‘24 Foot Structures.’ “But you can have an arch that causes not foot pain, but back pain. So often, high-arch people have back pain, but they don’t realize it’s coming from their feet.”
This chart, and DeCaro’s extensive use of it to explain problems people are having now — or might have later — is just one of many reasons why he was named the Healthcare Hero for 2021 in the always-competitive Provider category. Indeed, he has made pediatric podiatry his specific specialty, and throughout his career he has helped people of all ages, but especially children, make great strides, both figuratively and quite literally.
“To get a hug from a parent who tells me that their child is finally walking or is able to run or keep up with their friends … that’s really priceless.”
He has done this through everything from education to complex surgical procedures, to the development of new orthotic products, such as littleSTEPS, orthoses created specifically for young people and designed to improve coordination, balance, pain, posture, and strength, while aiding in the development of a more stable and functional gait.
He even makes an impact through his photography. DeCaro, who travels often with his family and through his work, photographs animals wherever he goes and winds up selling prints of some of his best shots, with the proceeds going to help families in need offset the cost of orthotics.
Thus, his work can be — and often is — described as life-changing, and that’s why he finds all facets of it, but especially his work with children, so rewarding.

Dr. Louis DeCaro, seen here with his children, Eliza and Lucas, and wife Jamie, says foot issues impact people of all ages, starting with the very young.
“People often ask me why I do pediatrics,” he said. “And I tell them that one of the wonderful things I get to experience is when a child follows up who couldn’t walk, and I helped them walk; that’s got to be one of the most rewarding things in the world. To get a hug from a parent who tells me that their child is finally walking or is able to run or keep up with their friends … that’s really priceless.”
Over the years, DeCaro has received many hugs like that, and that just begins to explain why he is one of the Healthcare Heroes for 2021.
Positive Steps
Like many in healthcare, DeCaro said that, while he ultimately chose his specialty, in many ways, it chose him.
Relating the story of how he ventured into podiatry, he said he had just finished his junior year at Stony Brook University on Long Island and was on a path to a career in allopathic medicine when he got a letter from someone at Barry University, a podiatry school in Florida.
“I didn’t know anything about podiatry at all,” he recalled, adding that the school was impressed with his MCAT scores and offered to fly him down for a visit. He took them up on their offer and came away impressed with the school, the specialty, and the opportunities it presented.
“Podiatry seemed like a wonderful profession because I could specialize in whatever I wanted — I could do surgery if I wanted to, I could treat kids if I wanted,” he said, adding that he wound up skipping his final year at Stonybrook and getting on an airplane to attend Barry.
“It was the best decision I’ve ever made; getting into this specialty has been wonderful, “he went on. “It was an opportunity-knocks moment — and I opened the door to see what was behind it.”

Dr. Louis DeCaro photographed this bear while visiting Alaska. The image is one of many he has sold to help families pay for needed orthotics for their children.
To say that DeCaro has made the most of his opportunity and had a profound impact on patients and their families during his career in his chosen field would be a huge understatement. Indeed, as noted, he has been changing and improving lives in many ways — through education, treatment, and the development of new orthotic solutions, such as littleSTEPS.
DeCaro Total Foot Care Center now counts 30,000 active patients, with some of them coming from other states and the four corners of Massachusetts.
“Besides Boston Children’s, which is two hours away, there’s really no other pediatric specialist in this state for foot care,” he explained. “So we get patients all the time who travel two or three hours to see me, just because of the lack of pediatric specialists.”
He said podiatry is regarded by many as a specialty focused on the elderly and the diabetic, and while many of the practice’s patients are in those categories, foot issues impact people of all ages. And many problems of the foot develop when people are young.
DeCaro said he treats many children on the autism spectrum with sensory-processing disorders, others with neuromuscular diseases like cerebral palsy, children who are late walkers or delayed walkers with low muscle tone, athletes with injuries that start with their foot structure, kids with growing pains, and those with other ailments.
“Often, orthopedic issues, especially in the pediatric population, are caused by poor mechanics in the foot,” he explained. “And it starts with the minute we walk.”
He said he sees roughly 20 patients a day, fewer than many specialists, because he enjoys spending time not only with his younger patients, but their parents as well, because they often must be educated about their child’s condition.
Similarly, when he sees a child, he will often then examine the parents as well because, by looking at their respective foot structures, he can often gain some perspective on where that child might be headed when it comes to overall foot health. “Like hair color and eye color, foot structure is genetic,” he explained.
As noted earlier, treatment of his patients is just one of the reasons why DeCaro has become a standout in his field — he has been listed among the 150 Most Influential Podiatrists in America by Podiatry Management magazine — and why he will join seven others as Healthcare Heroes on Oct. 21 at the Log Cabin. He’s also an educator who lectures often; pens articles such as one called “Assessing the Role of Gait Analysis in Pediatric Patients with Flatfoot,” which appeared in Podiatry Today magazine; and teaches the ‘24 Foot Structures’ to many of his colleagues.
Within the 24 different foot structures there are six distinct foot types or categories — A to F — and given each names, like ‘John Wayne.’ “You actually turn your legs out and walk like a gunslinger,” he explained, adding that there are fun names for each category, and they are designed to help patients understand their feet and the treatment being given them.
He’s also an entrepreneur; in addition to littleSTEPS, he and business partner Roberta Nole have also developed the RX24 Quadrastep System, a state-of-the-art alternative to traditional custom orthotic management.
There’s also his photography — and philanthropy, by which he uses his hobby to help children and families in need.
The walls of the rooms in his office are covered with photos — his favorite is one of a puma he “met” in the rain forest of Costa Rica, although he’s also fond of a bear he photographed in Alaska — primarily his feet (paws), which are prominently on display.
When asked how he gets so close to his subjects, he quipped, “big lenses.”
Toeing the Line
In many ways, DeCaro has spent his career helping patients, and especially the younger ones, understand the proverbial big picture when it comes to their feet and how they are never to be overlooked when it comes to one’s health, well-being, and quality of life.
Suffice it to say that he has made the most of that opportunity-knocks moment when he got on a plane bound for Florida and podiatry school. He found a profession that has been rewarding in every way imaginable.
But the real winners from that decision he made are his patients, who have benefited from his compassion, his desire to educate, and even his ingenuity and prowess as an entrepreneur.
His ability to change their lives has made him a Healthcare Hero.
George O’Brien can be reached at [email protected]
Community Health
Counseling and Testing Prevention and Education Program Director,
New North Citizens Council Inc.

Richard Johnson
He Has Made a Career of Being There for People Who Need Help, Direction
Richard Johnson has a simple and laudable philosophy when it comes to those seeking help. And it goes a long way to explaining why he’s a Healthcare Hero for 2021 in the always-competitive Community Health category.
“When people who are in need find the fortitude to step out of themselves and ask for assistance, there should be somebody to respond,” he told BusinessWest. “That’s because it takes a lot sometimes for many people to ask for help. And so, I like to make sure that, if I’m able, I can be that person to respond.”
For more than two decades now, during a lengthy career in public health, most recently as Counseling and Testing Prevention and Education Program director for the New North Citizens Council Inc., Johnson has been able — and ready — to respond and provide that help, in the many forms it can take.
His title is a mouthful, and there is a lot that goes into it.
Indeed, from his office at the Deborah Hunt Prevention and Education Drop-in Center, Johnson helps those in the Mason Square area of Springfield and beyond cope with issues ranging from HIV and sexually transmitted diseases to opioid and other addictions; from sickle-cell anemia awareness to treatment for mental-health issues.
And with the arrival of COVID-19, that list has only grown, with new responsibilities including everything from securing PPE for those in need to educating residents about the importance of vaccination. In short, he and his team have been helping people live with everything else going on in their lives and COVID.
“When people who are in need find the fortitude to step out of themselves and ask for assistance, there should be somebody to respond. That’s because it takes a lot sometimes for many people to ask for help. And so, I like to make sure that, if I’m able, I can be that person to respond.”
“We wanted to provide an education for these individuals so they could limit or at least mitigate some of their risk factors for contracting COVID and other things,” he explained. “So 2020 became COVID-intense. Our focus changed; our priority was educating people on how communicable this disease was, and saying to them, ‘yes, I understand that you have addiction challenges and housing challenges, but you really need to pay attention to how to prevent contracting COVID, and then we can work on some of the other things.’”
A day in the life for Johnson takes him to the drop-in center, but also to the neighborhoods beyond for off-site presentations and testing at various facilities on subjects ranging from substance abuse to prevention of communicable diseases to overdose prevention and Narcan distribution. These sites include the Friends of the Homeless facility, Carlson Detox Center, Opportunity House, Bowen Center, and Valor Recovery Center.

Richard Johnson, center, with many of the team members staffing the Deborah Hunt Prevention and Education Drop-in Center in Mason Square.
COVID has reduced the numbers of such visits, but the work goes on, he said, adding that it is highly rewarding in many respects, because through it, he is helping not only individuals but neighborhoods and the larger community become more resilient.
This has become his life’s work, and his devotion to that work, that mission, has made him a Healthcare Hero for 2021.
Source of Strength
As he talked with BusinessWest in the tiny lab set up in the drop-in center, near the Rebecca Johnson School, Johnson said the facility lives up to every word over the door.
It is, indeed, a drop-in center, where one can find testing, counseling, education, and help with prevention. There is a team of individuals working there, but Johnson is the leader, in every aspect of that word. Meaning, he sets a tone for the work there, one born from experience working with this constituency and trying to meet its many and diverse needs.
He first became involved in community health in 2002, when he volunteered for an agency called Northern Educational Services, funded by the Massachusetts Department of Public Health.
“There were a number of folks I knew who were impacted by substance use and HIV,” he explained. “So this provided an opportunity for me to be directly involved in trying to navigate them to some sort of care.”
After this stint as a volunteer, he joined Northern Educational Services as a relapse counselor, and from there, he went from relapse prevention to HIV case management, starting first as an assistant and then working his way up to senior case manager. Ultimately, he became the director of Counseling and Testing Prevention and Education Services.
“Much of my work as a case manager centered on really just helping people to adjust to a new reality with regard to being diagnosed with HIV and confronting some of the stigmas associated with that,” he told BusinessWest. “I helped them understand that there are treatments that were effective, and helping them to communicate with their physican or medical provider as to what their concerns were and how their lives worked in terms of some of the stigmas associated with it and being able to talk to loved ones about their new status.
“That was really challenging for some,” he went on. “And so, case management at that time was a very hands-on thing; we made a great difference in the lives of those who were living with HIV, but equally so those who were unaware of how it was transmitted, and what prevention methods could be deployed by them, and that it was OK to have dinner with someone who was living with HIV, as opposed to some of the rumors, stories, or myths that they’d heard.”
Elaborating, he said that, for many, substance use and HIV went hand-in-hand, and efforts focused on helping people find recovery through detox and treatment facilities and helping these individuals understand that it was OK to live substance-free and face and confront some of their challenges involved with having a diagnosis that was highly stigmatized.
In 2010, he assumed that same title — director of Counseling and Testing Prevention and Education Services — with the New North Citizens Council, and has been continuing that challenging but needed work to counsel those in need and help with the medical and social aspects of HIV, sexually transmitted diseases, and substance abuse, while connecting people with healthcare providers.
“We’ve been very fortunate to have built relationships with medical providers that lend themselves to understanding that when we have an individual, that service, that treatment, needs to be provided, and they’re willing to provide it,” he said, listing Baystate Medical Center, Mercy Medical Center, and the Caring Health Center among the providers he and his team work with.
Over the years, Johnson has become involved with a number of community groups, boards, and commissions, including the Mason Square C-3 Initiative, the Massachusetts Integrated Planning Prevention Committee, Baystate Health’s Mason Square Neighborhood Health Center Community Advisory Board, the Baystate Health Community Benefits Advisory Council, and the Springfield Food Policy Committee.
As noted earlier, COVID has added new layers to the work and the mission for Johnson and his team. While helping individuals and families cope with what would be considered everyday matters, there is also a once-in-a-century pandemic to contend with.
Work to distribute PPE and other needed items, from masks to hand sanitizer, socks to toothpaste, goes on, said Johnson. “We still go about daily and provide PPE to people who are on the margins and often don’t have ready access to such items.”
Critical work on vaccination goes on as well, and comes in many forms, from education to dispel myths and misinformation to getting shots in arms. He mentioned a clinic at the drop-in center the day before he talked with BusinessWest, at which nine people received their second shot and two more got their first.
“Vaccination has been a challenge because there is a lot of information out there, and not all of it is accurate,” he explained. “There’s a significant amount of resistance based on information that individuals have received, so it’s really about re-educating people and helping them achieve a level of comfort receiving new information. As great and wonderful as the internet and social media are, sometimes it doesn’t provide both sides of a story.”
Bottom Line
Helping individuals and families achieve a needed level of comfort with many aspects of their lives — from living with HIV to battling substance abuse — has long been the best way to describe Johnson’s work and his commitment to the community.
As we noted that at the top, he fully understands just how hard it is to seek help. And that’s why it’s been his mission to be there for those who find the strength and fortitude to take that step.
His unwavering commitment to that mission has made him a Healthcare Hero.
George O’Brien can be reached at [email protected]
Amid the Crisis at the Soldiers’ Home, This Small Army Answered the Call

The Staff of Holyoke Medical Center
It was coming up to noon on Friday, April 4, and the staff at Holyoke Medical Center was frantically working to ready facilities there for the arrival of residents of the nearby Holyoke Soldiers’ Home, who needed to be relocated in the midst of a tragic COVID-19 disaster that would make headlines across the country.
Carl Cameron, HMC’s chief operating officer, who was overseeing that work, was on the phone with his boss, hospital President and CEO Spiros Hatiras, who was telling him that some promised National Guard personnel would likely soon be arriving from the Soldiers’ Home to help with the massive and complex undertaking.
Cameron’s response more than sets the tone for a truly inspiring story that most still haven’t heard, but certainly should.
“I told him that at that point not to bother,” he recalled. “Because we had our own army of people. And it was absolutely outstanding and amazing how that team came together and got this done.”
“We had our own army of people. And it was absolutely outstanding and amazing how that team came together and got this done.”
Indeed, HMC’s small army, which would grow in numbers in the coming days and weeks, as we’ll see, came together in every way imaginable to bring 39 residents of the home into a hospital that was in the early stages of the COVID-19 fight itself. An acute-care hospital, HMC was not in the business of providing long-term care. But, to borrow a phrase from hockey, it shifted on the fly, and essentially got into that business.
There was a learning curve — staff members were certainly not used to people in HMC’s beds making requests (better make that demands) for their favorite brand of beer — but they did learn, and they made the veterans/patients/residents feel at home at an extremely difficult time.
They decorated the hastily created living spaces with flags and red, white, and blue ornaments. They found the soldiers television sets. They provided much-needed information and comfort to those soldiers’ family members, many of whom had no idea where they were. They’ve helped a few of their guests celebrate 100th birthdays since their arrival. Outpatient physical therapists were taken off furlough to become veterans’ liaisons, helping the Soldiers’ Home residents with daily functions as well as helping them maintain connections with loved ones. Office assistants stepped in to assist with patient care.
Summing it all up, Hatiras said his staff came together, as perhaps never before, amid a crisis that tested the medical center on every level imaginvable — and earned the designation of Healthcare Hero for 2020 not only from BusinessWest, but from the Huron Studer Group, one of only four such awards that organization issued across the entire U.S.
Spiros Hatiras
“Everyone put their roles aside and said, ‘all hands on deck.”
“Everyone put their roles aside and said, ‘all hands on deck,’” Hatiras noted, summoning still more military language as he praised every department in the hospital, from Plant Operations to Communications to Environmental Services, for the specific roles they played. “And what we’ve learned, aside from all the bonding and being more comfortable in different roles, is that we’ve technically become much more astute. We’ve learned things from a technical standpoint that would allow us to respond to a second wave or other kind of pandemic, because now we’ve got it right; we know how to convert rooms under pressure, we know how to isolate people, we know how to shift things around, we know how to use alternative ways. We’ve learned so much by going through this.”
As several of those involved with this herculean effort talked with BusinessWest about it, much of the discussion focused on that first day and night — and for a reason.
The hard work of setting up spaces for the soldiers — an outpatient cardiac-services unit and a maternity unit that has seen declining volume for several years — had been completed by mid-afternoon — as noted, without the help of the National Guard.
As he talked about the mad dash to get the rooms ready, Angelo Martinez, a member of the Plant Operations team, spoke for everyone in the room when he spoke of those who be staying in those rooms.
“At end of the day, I was tired, but it was a good feeling,” he said. “Because these veterans did a lot for us, and we owe them for all they’ve done.”
Those units were ready by 3 p.m., the end of a shift for many of those involved. But just about everyone stayed until those soldiers finally started arriving by van in the early evening. And they stayed on until the last of them arrived around midnight. And still they stayed on until the soldiers were settled into their new quarters.
Kaitlyn Nadeau, a surgical technologist, was one of them. She told BusinessWest she was unaware that the hospital was taking on the veterans because it had been a busy day in the operating rooms. When she learned, around 3 in the afternoon, she and others went about setting out a welcome mat.

Korean War Veteran Richard Madura, seen here with recreational therapist Mary Argenio, is one of 39 veterans who found a new home at Holyoke Medical Center.
“We made hearts to put on the walls because … it’s a basement, and it’s white walls, and it’s kind of scary when you walk in,” she explained. “So we decorated it like we were going to stay there. Because if it were my grandparents coming in … most of these people are confused as is, and they’re coming to this facility they’ve never been to.
“So we decided we were going to stay there,” she went on. “Hours went by, and they still hadn’t arrived because it’s quite the process to get them here. Finally, I said, ‘let’s get more people down here.’ My boss just started grabbing people from everywhere; people from the command center showed up, and managers from other departments, and CNAs … everyone just came together, including people I’d never met before in my life, to welcome them here and get them settled in.”
This coming together as a team during that first 24 hours or so set the tone, but it was really only the first chapter in a story that, seven months later, is still being written.
Indeed, soon after the veterans arrived, some began showing signs of the virus, meaning more space would have to be readied for these guests, and single rooms would be needed to slow and hopefully stifle any spread.
Also, the hospital, and especially its nursing staff, had to pivot to providing long-term-care services.
“Being an acute-care hospital, we’re not normally planning things out for long-term-care residents,” Nurse Manager Christina Straney said. “But many of our nurses have worked in long-term care, so they stepped up and said, ‘let me take this, let me run with this, let me show you what we do in nursing homes and how we care for patients.’”
Meanwhile, some of the certified nursing assistants had worked at the Soldiers’ Home and recognized some of the patients, she went on, adding that this helped create a fluid, almost seamless transition for the veterans.
Likewise, the furloughed physical therapists stepped into their new roles as veterans’ liaisons, a role that came about out of necessity, Hatiras explained.
“We had the matter of individual preferences,” he said. “I would get on a Zoom call, and I would have family members say, ‘remember, Ed doesn’t eat eggs, and he doesn’t like mayo, and he takes his tuna fish this way, and he likes his newspaper every morning’ … and I’m like, ‘whoa, how am I going to remember all this stuff?’”
The solution was to assign liaisons to each of the veterans. Jeff Ferriss is one of them. He was furloughed on a Friday and called back to work the following Monday to serve in this unique role.
“My father was a veteran — he spent 20 years in the Air Force. My brother spent four. And I’m also a veteran — I was in the National Guard and the Air Force Reserves,” he said. “So this was the perfect transition for me; I was happy to come back and help out. Our job was to keep the family members informed, but being therapists, we tried to goad them into therapy too. Some of them may not have wanted to do that, but over time, they needed to — they were stuck in their rooms, and we were trying to keep their minds going and keep them going physically. It’s been an honor to serve these people.”
Veterans like Richard Madura. A Korean War vet, he will tell you (without much prodding, by the way) that, through his 85 years, he’s been fortunate enough to be in the right place at the right time — on most occasions.
Indeed, the long-time Chicopee resident arrived in Korea just as the truce between the warring factions was being signed. And when it looked like he was ticketed for taking up a gun and maintaining the peace along the DMZ, an officer who noticed on his résumé that he had musical experience and had been part of some polka bands, let him take up a clarinet in an Army band instead. To make a long story shorter, his band entered a string of talent contests, ultimately won first prize, and wound up on The Ed Sullivan Show.
Madura told BusinessWest that this habit of being in the right place extends to his current, but certainly not permanent, mailing address at Holyoke Medical Center.
“They take really good care of you here,” he said, not wanting to compare the facilities to those he left just up the hill at the Soldiers’ Home, although he did hint that the desserts are better — and larger — at HMC. “I’m fortunate to be here; we all are.”
Indeed they are. A small army answered the call last April, and it is still answering the call, making the staff at HMC a true Healthcare Hero in a year when there are many to celebrate.
George O’Brien can be reached at [email protected]
His Efforts to Coordinate the Region’s Pandemic Response Saved Lives

Mark Keroack
Dr. Mark Keroack doesn’t feel like a Healthcare Hero. But he’ll gratefully accept the honor on behalf of everyone who does deserve the award.
In his estimation, that’s a lot of people.
“Whenever some new challenge comes up, it’s been our tradition to step up and play a leadership role in Western Mass.,” said the president and CEO of Baystate Health. “I wish I could convert my award into an ‘unsung heroes award.’ So many things happened behind the scenes to enable us to step up.”
And so many people stepped up. Like Dr. Sarah Haessler, an epidemiologist who has long had a keen interest in emerging infections. “She got us to construct an ebola-treatment unit in 2014, and she put together a small team of people interested in unusual infections,” Keroack said. “That team reassembled this year, in early January, when they started issuing alerts looking out for anyone traveling from China.”
Or Dr. Lauren Westafer, an emergency medicine physician who helped determine, early on, that not rushing to place patients on ventilators actually decreased COVID-19’s mortality rate. “We were far ahead of the curve on that,” Keroack said.
Or Baystate Medical Center President Nancy Shendell-Falik, a former nurse who understands patient flow, he said, noting that Baystate, on an average day, has about 720 patients, but was able to open up hundreds more beds by postponing elective surgeries and finding other creative ways to open up space and redeploy staff.
Or Dr. Andrew Artenstein, the system’s chief physician executive — and, like Haessler, an infectious-disease expert — who led Baystate’s Incident Command Center. In addition to his day-to-day role coordinating the system’s pandemic response, he drew national attention after penning an account of a rendezvous at a small mid-Atlantic airport, where he and his team brought a $3 million check to purchase a large shipment of face masks and N95 respirators — and were temporarily accosted by the FBI.
“We realized we were on our own,” Keroack said of those early days, noting that the health system also received PPE donations from the construction trades and local manufacturers, who had shifted to making such equipment. It was a lesson to the region that local players could produce what they needed and not have to depend on a fractured global supply chain.
“I wish I could convert my award into an ‘unsung heroes award.’ So many things happened behind the scenes to enable us to step up.”
But he mostly applied the ‘hero’ designation to every frontline provider who continued to push past their health and safety anxieties and do their jobs. “They were able to do the right thing in spite of their fears, and are heroes in my book.”
That book includes story after story of collaborations Baystate forged in support of prompt community outreach, testing, education, and information, all with the goal of limiting the spread of COVID-19 and helping make Massachusetts — one of the hardest-hit states in the pandemic’s early days — an eventual model of how to control it.
On the local level, Keroack participated in Springfield Mayor Domenic Sarno’s weekly COVID-19 press briefings, leading the mayor to note that “Dr. Mark Keroack’s leadership and medical insight has truly been a great benefit for our city of Springfield as we have worked together to defeat and mitigate the spread of this virus.” Baystate also tested the homeless population and expanded testing to key neighborhoods in the city at the request of the state and local officials.
Keroack also convened calls with Westfield Mayor Don Humason regarding clusters of positive cases in Westfield’s Russian community and possible spread beyond its borders. Meanwhile, he conducted weekly calls with the Western Mass. legislative delegation and other area hospital CEOs, while crafting a plan with state officials on how Baystate would provide surge beds for the region.
“I set up an independent command center, and every day at 7:30, we’d call a group of people who included hospital presidents, heads of medical groups, people from infection control, supply chain, finance, communications … 15 people got on the Zoom meeting every day,” he said, adding that information from those sessions would be distributed as a bulletin at 11 a.m. “It was the most widely read thing at Baystate. Everyone knew every day where we were.”

Mark Keroack (right) and U.S. Rep. Richard Neal take part in an outdoor roundtable on COVID-19 issues in the spring.
Keroack also served as the only Massachusetts hospital CEO appointed by Gov. Charlie Baker to the state’s Reopening Advisory Board. “The Reopening Massachusetts plan needed to balance restarting commerce while avoiding a surge of virus cases,” said Mike Kennealy, Secretary of Housing and Economic Development. “Dr. Keroack’s medical expertise and healthcare-sector experience, and his perspective as a resident of Western Massachusetts, helped to ensure those dual objectives were addressed.”
For his part, Keroack praises the state’s phased approach, which has understandably been frustrating to business owners.
“We’re using data to move from one phase to another, and we’ve had good coordination between authorities and scientists, as opposed to some states, where they butted heads with each other,” he added. “In Massachusetts, there hasn’t been any daylight between what science is telling us and what local and state officials are saying.”
If there was an unseen ‘hero’ amid all the named ones, Keroack suggested it may have been a public that understood its role, and today still largely adheres to guidelines around social distancing, mask wearing, and other protocols.
“I’m proud of how we worked together and came together as a community,” he told BusinessWest. “Parts of the country were at loggerheads, fighting with each other about masks, getting their hackles up about personal liberties. I look at that craziness and think, thank God we didn’t have to go through that.”
On the other hand, the community’s responsibility was clear. “We had the advantage of knowing what happened in Italy and New York, so we didn’t have to twist people’s arms to take this seriously. The public understood the issue around shutting down.”
At the same time, he’s proud of Baystate’s role in working with local boards of health and the Department of Public Health around contact tracing. “In six months, from the announcement of the first case, we have gone from having to beg to get a person tested to being a regional testing center that does 1,000 tests a day,” he said, with the total tests approaching 100,000 toward the end of September.
About a third of those tests, he added, have not even been Baystate patients, but patients from other hospitals and folks living at nursing homes, assisted-living facilities, and homeless shelters. “We got outside the walls of our own system into the community and really played a role in public health.”
While the pandemic is far from over, Keroack already recognizes some of the changes that might emerge from it, from an expanded role for telehealth to a better understanding of where society’s safety nets have proven inadequate.
“This has kind of exposed some of the shortcomings of our healthcare system and of our social support system, like the number of people in this country who don’t have paid sick time, and go to work even when they’re sick,” he said.
Some of the long-term impacts of COVID-19 are still emerging, he added, but Baystate — and the team of heroes with whom he insists on sharing his honor — will continue to, as he said, step up and play a leadership role.
“Every time a pandemic hits society, people who live through it are changed forever. That’s true of every pandemic throughout history,” Keroack said. “We’ll look at the world differently in terms of healthcare as a right, or childcare and sick leave — we’ll look at these issues very differently than we would have just a few years ago. At least, I hope we will.”
Joseph Bednar can be reached at [email protected]
They Moved to the Front Lines at the Height of the Pandemic
 Lydia Brisson was out for a hike with her young son on the mountain behind their home late last March. The objective was to get some exercise, but for Brisson, there was another purpose to this trek.
Lydia Brisson was out for a hike with her young son on the mountain behind their home late last March. The objective was to get some exercise, but for Brisson, there was another purpose to this trek.
Indeed, while walking, she was also talking … and trying to prepare her son for the very real possibility that she might soon have to go on the road, if you will, and move from behind-the-scenes work as a clinical liaison for Berkshire Healthcare Systems (BHCS) to the front lines of an emerging pandemic.
And within minutes after returning to the house, her cell phone rang.
On the other end was Lisa Gaudet, vice president of Business Development & Marketing for BHCS, who was asking if she would be willing to pack up, travel across the state, and serve for an indeterminate amount of time as a floor nurse at BHCS’s long-term-care facility in Danvers, on the North Shore.
Lydia Brisson
“Then, families are calling constantly because they want to know if their loved ones are OK; things were changing day to day and even moment to moment.”
Brisson didn’t hesitate in responding with a solid ‘of course,’ and that same response was also given by Christopher Savino and Emeline Bean, Western-Mass.-based BHCS clinical liaisons who got similar calls from Gaudet.
Soon, the three would be together in Danvers — out of their territory, away from their families, and smack in the middle of a crisis; there were nine active cases at the facility on the Saturday when those calls were made, several staff members had become ill, and many others had stepped away from their roles or refused to come to work.
As executive leaders at BHCS worked every possible lead and angle to find more nursing staff, Gaudet put out calls to these three members of her team who were nurses. They all said ‘yes,’ but admitted to having no real idea what they were getting themselves into.
So began a truly inspiring story, one that would bring these three closer together — or even closer, in the case of Savino and Bean, who went to high school together and worked side by side. Over the course of a dozen or so days in Danvers, they would get well-acquainted with Bagel World, become very tired of pizza, recall crying in the shower after watching one of their patients — a phrase that takes on special meaning, to be sure — die from COVID-19; vividly remember taking phone calls from family members desperate for information about a loved one, and come to really appreciate some rest at the Residence Inn in Peabody after 15- or even 18-hour shifts.
Christopher Savino
“Berkshire’s mission and values state that we’re here to serve the population that needs us, and that was a population that needed us. We’re clinical liaisons, but we’re also nurses; we went to nursing school for a reason.”
As the three talked about their experiences with BusinessWest at BHCS’s facilities in the Cubit Building in Holyoke, they all stressed that, for them, volunteering for this assignment was a no-brainer; saying ‘no’ wasn’t something that really entered their mind — although, as clinical liaisons, a role in which they focus on evaluating patients for placement at one of BHCS’s facilities, they are a long way from the front lines.
“I didn’t really give my husband much of an option,” said Bean, who has a young child herself, as she recalled that phone call from Gaudet. “The need was there, and this is why you take that oath.”
Savino agreed. “Berkshire’s mission and values state that we’re here to serve the population that needs us, and that was a population that needed us. We’re clinical liaisons, but we’re also nurses; we went to nursing school for a reason.”
Those nearly two weeks on the road were learning and growing experiences on every level imaginable, they said, adding that they will never forget any of this, but especially what they encountered upon arriving.
“There were nurses who wanted to hug us — but couldn’t — because they were desperate for help,” Bean recalled. “And there were scared people; everyone was like, ‘what do we do?’ The state was changing guidelines every day.”
“This was completely different from what we did every day. And it’s given me a new and different perspective on my job. Since we were on the outside in our day-to-day work, this experience reminded me of what those on the inside are challenged with on a day-to-day basis, when all the cards are stacked against you.”
Savino noted that he and Bean, who followed each other to Danvers, arrived a day ahead of Brisson. Their first assignment was the dementia unit.
“You take a dementia patient — they don’t really know already what’s going on,” he told BusinessWest. “Now you tack on a mask, goggles, and essentially you look like a Ghostbuster that’s coming at them with medications, oxygen … they were terrified. They had no idea what was happening, they couldn’t leave their rooms — it was a very difficult situation.”
And while tending to patients, the three were also trying to assist families, who were often desperate for information about their loved ones.
“We were going into an extremely sad situation — there were a lot of unknowns,” Brisson said. “And then, families are calling constantly because they want to know if their loved ones are OK; things were changing day to day and even moment to moment.”
Savino agreed. “Our first day on the dementia floor, I remember getting a call; a patient’s daughter called and said, ‘how’s mom?’ I said, ‘she’s still negative … I haven’t gone to see her yet, but I’ll get there.’ She ended up testing positive 24 hours later and dying a day after that. I remember just breaking down in the shower.”
The three went over as a team, and they recall supporting each other, and others they were working with, throughout their assignment away from home.
“Every night, the three of us would have dinner together,” Savino said. “Every single night, we would decompress. If one of us had an overnight shift, one of the others would get food and leave it outside that person’s door. We had each other, thankfully.”
When asked to put the experience in perspective and talk about how it impacted them and perhaps changed them, the answers were provocative.
“This experience fueled my fire,” said Brisson. “My real passion is direct-care nursing, and although my boss may not want to hear this, it did make me realize that that’s where I will make the greatest difference and help the most people.”
Added Savino, “we all became nurses for a reason — putting everyone else’s life before our own. This experience just reinforced why I became a nurse and why, no matter what, even if I’m in administration, I will always keep my nursing license.”
For Bean, the experience was somewhat different in that she had been at the bedside before. But those 12 days still had an impact on her, professionally and personally.
“It brought me back and made me miss that aspect of nursing,” she told BusinessWest. “This was completely different from what we did every day. And it’s given me a new and different perspective on my job. Since we were on the outside in our day-to-day work, this experience reminded me of what those on the inside are challenged with on a day-to-day basis, when all the cards are stacked against you.”
Returning to that day last March when she got that phone call, Brisson recalled a conversation afterward with her husband, who was naturally concerned and tried to convince her this was not her job and she didn’t have to go.
She recalled that she agreed — to the extent this wasn’t exactly within her job description at that specific moment in time. But as for not having to go … she respectfully disagreed. This was a big part of her job, a big reason why she chose this profession.
Her argument didn’t exactly persuade her husband, but it clearly explains why she, Bean, and Savino are all Healthcare Heroes.
George O’Brien can be reached at [email protected]
At a Time of Crisis, Collaboration Was Key to Meeting the Most Pressing Needs

Peter Reinhart, director of IALS.
In mid-March, when much of the U.S. was starting to hunker down, Peter Reinhart had a feeling he wouldn’t be — and neither would many of the people he works with.
“We didn’t want to be sitting at home watching this pandemic unfold without doing something,” said Reinhart, director of the Institute for Applied Life Sciences (IALS) at UMass Amherst, a facility launched in 2013 with the goal of accelerating life-science research and advancing collaboration with industry to shorten the gap between scientific innovation and technological advancement.
COVID-19 presented a unique opportunity to do exactly that, under time constraints that truly meant something, because people were dying every day. Take, for example, the work at IALS to develop a low-cost face shield for rapid production.
“We are a platform organization that caters to all departments on campus — nursing, computer science, natural sciences, public health, engineering,” Reinhart said, naming just a few. “Because our institute creates an interface across all these different organizations that are usually siloed, it’s much easier for us to pull together nursing staff, molecular biologists, and engineers, and say, ‘we need to make face shields in the next seven days. How can we do it?’ And they did.”
It took a few tries to get the design right, but the team eventually partnered with K+K Thermoforming of Southbridge to fabricate and distribute 81,000 face shields throughout the region. About 50,000 more followed in a second batch, all able to be shipped flat, 300 to a box, and assembled in 20 seconds by the user. Partly because of the logistics of billing and partly because the need was so pressing, IALS essentially gave the shields away.
“The differentiator between UMass and every other organization I’ve ever worked at — in both industry and academia — is this spirit of collaboration,” Reinhart told BusinessWest. “I’ve been at organizations where it’s very hard to get collaborations working across departmental boundaries. It’s much more self-contained, focused on individual greatness as opposed to collective greatness. That’s the difference I see at UMass Amherst — people across organizational boundaries will jump in and help you.”
When the pandemic hit, IALS’ culture and understanding of interdisciplinary work was especially valuable, and eight or nine response teams began working on individual projects, he explained, “some with greater and some with lesser success, but all of them with the best of intentions: to make a difference with the problems that were facing us as a society, using whatever resources we could apply to them.”
“We didn’t want to be sitting at home watching this pandemic unfold without doing something.”
One early project took aim at a worldwide mask shortage. Not all face masks can be safely sterilized and reused, but Professor Richard Peltier’s team demonstrated that hydrogen-peroxide sterilization for N95 respirators does, in fact, work. Using state-of-the-art pollution instruments to measure whether microscopic particles can pass through the mask after it’s sterilized, the results showed no real difference in filtration between a new mask and a sterilized one.
In another project, Baystate Health resident physician Dr. Mat Goebel and respiratory specialist Kyle Walsh contacted the College of Engineering for help with ventilators. Regular, 10-foot ventilator cables were on extreme back order, and longer cables, which would provide added safety to staff by increasing distance and reducing the need for PPE, did not exist. UMass engineers were able to fabricate a 50-foot cable that was compatible with Baystate’s ventilators, and contacted Michigan-based Amphenol Sine Systems, who agreed to design and fabricate the longer cables.
“It’s a really intriguing model,” Reinhart said of the collaboration that went into each project. “It could be a model of the future, to allow interdisciplinary work to function on a campus that by necessity has these organizational boundaries.”
Another team set up local production of viral transport media (VTM) for COVID-19 clinical testing. As testing ramped up nationwide, the solution used to keep COVID-19 samples safe during transport was in short supply, and local hospitals contacted Reinhart for help.
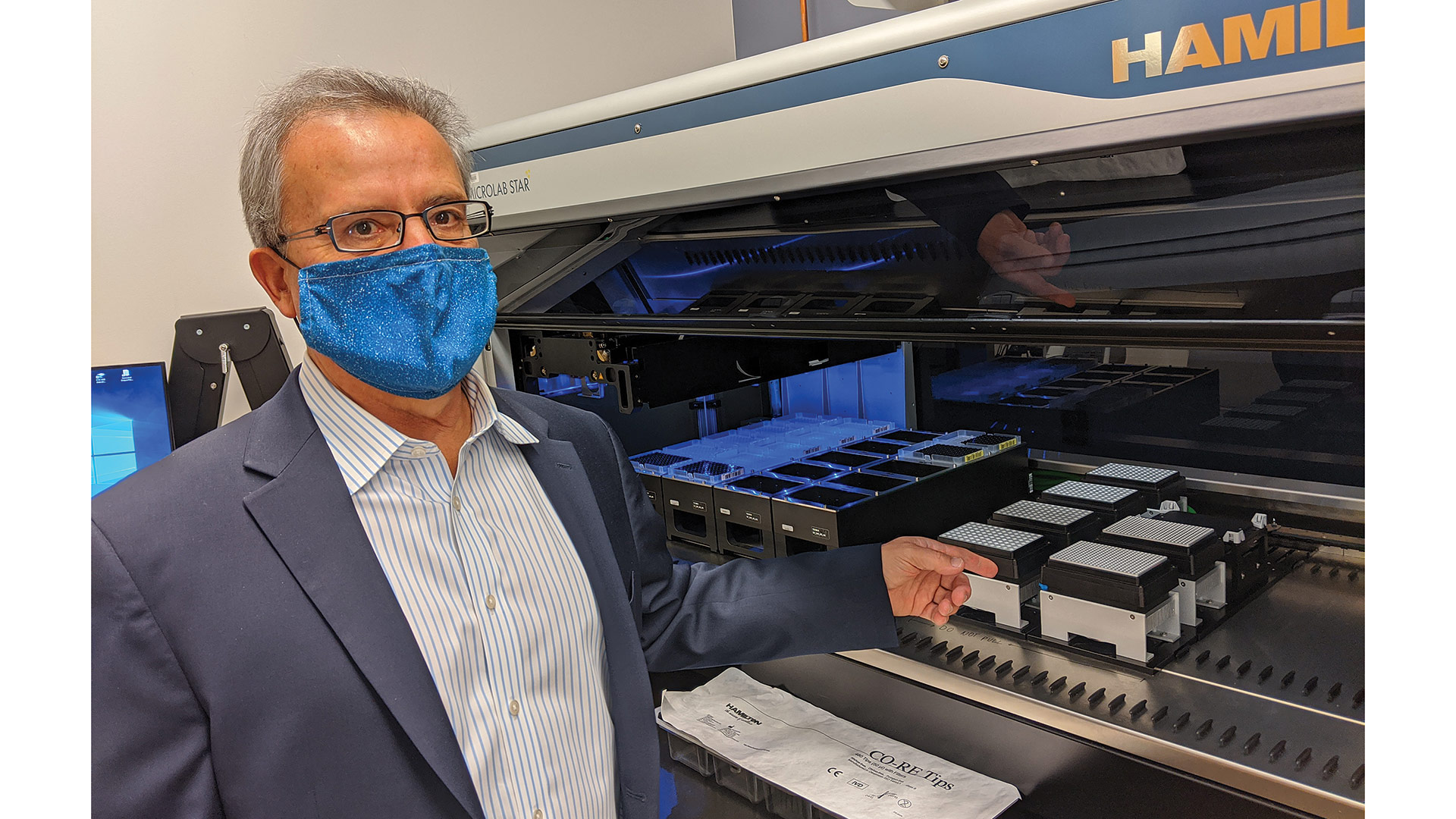
Peter Reinhart with some of the equipment that can process thousands of COVID-19 tests every day on the UMass campus.
Within one week, IALS had produced, tested, and distributed enough VTM to test 600 patients, before scaling up production and delivery to meet the needs of frontline workers across the state. The campus has enlisted more than 60 volunteers who produce, test, package and distribute VTM, and have provided hundreds of thousands of vials to seven regional hospitals and healthcare facilities and the Massachusetts COVID-19 Response Command Center.
“That project has grown because the need was much larger than anticipated,” Reinhart said. “It was good to see we had so many people prepared to put in their time to help, and great to see that people who had run out of the ability to test were back doing testing. We ended up doing a good thing.”
The latest project is a high-throughput testing facility where IALS can generate up to 5,000 COVID-19 tests per day, enough to have all students, staff, and faculty tested at least once a week.
“We hope this becomes a regional resource that serves the community with rapid testing,” he said, noting that a regional testing bureau charges between $120 and $160 per test, or between $2 million and $3 million per week at the volume UMass can now conduct in-house.
“Imagine what that does to your campus finances,” he went on. “We can do it at 10 cents on the dollar if we do it ourselves. Obviously, you need a major investment in staff, space, and equipment, but once we’ve made that investment, we can do much less expensive tests, they’re completely under our control, the turnaround time is super fast, and we can quickly put people into quarantine and do contact tracing.”
“The differentiator between UMass and every other organization I’ve ever worked at — in both industry and academia — is this spirit of collaboration.”
As time goes on, Reinhart said, IALS — and all the departments at UMass with which it collaborates — will continue to look for places it can make a difference. One ongoing effort involves the development of a clinical testing lab that can identify individuals with antibodies that can neutralize the COVID-19 virus. “Students can donate a sample, and we’ll tell them whether we’re making antibodies or not.”
These efforts to address the COVID-19 crisis — and other projects yet to be determined — will continue, he added, because the pandemic is “far, far, far from over.”
While Western Mass. has been fortunate with its infection numbers, the virus is still spreading at the same rate it was in March, he went on, and a combination of the upcoming flu season and “PPE fatigue,” among other factors, may yield a second spike of some kind. “I think we’re in for a period of increasing difficulties.”
That said, it’s been an immensely gratifying seven months at IALS.
“Everything was gloom and doom, everyone was at home, and it seemed that every news item you picked up was another downer on how dire things were,” he recalled of the situation back in March. “Creating a few feel-good stories and giving our students and faculty a chance to contribute to something positive was very helpful to them. I know it was for me.”
But it’s not how these dozens of unsung individuals feel personally that makes them Healthcare Heroes. It’s the difference they’ve made in the fight against a virus that has proven a persistent, resilient foe.
“We weren’t good at logistics; we were engineers,” Reinhart said of efforts like distributing those tens of thousands of face shields. But that effort demonstrates collaboration, too. “It was exciting. People were excited about throwing their weight behind a project that had immediate impact.”
Impact that will only continue as a truly challenging 2020 turns an uncertain corner into 2021.
Joseph Bednar can be reached at [email protected]
This Administrator Has Become a Calming Voice in the Midst of the Pandemic

Maggie Eboso
Maggie Eboso was in the grocery store when the first text message came in on the evening of March 26.
Soon, there were three more, and as her phone kept pinging, it became increasingly clear that her job as Infection Control coordinator at Mercy Medical Center was about to change substantially, and that she and the hospital were entering uncharted waters.
Indeed, the first suspected COVID-19 patients — two young women who had recently returned to the area from China — had arrived at Mercy, and there were questions that needed to be answered. Lots of them.
So began an ultra-intense period that has tested Eboso in all kinds of ways, but also taken her career to a new and different plane, one in which she has emerged as a Healthcare Hero.
Those frantic first days would set the tone for the weeks and months to come, during which Eboso would take on a number of responsibilities, many of them new — from coaching staff on the proper use of personal protective equipment (PPE) to helping all those at the hospital navigate a rough sea of changing guidelines and constantly changing information; from advocating for adequate supplies of PPE and working with colleagues to be good stewards of that precious equipment to providing a much-needed sense of calm amid a crisis unlike anything Mercy had seen before.
Her work during the early stages of the pandemic took her to every corner of the hospital, and also far outside its walls. Indeed, she taught PPE donning and doffing, hand hygiene, and infection-control practices to staff at the Hampden County Correctional Center in Ludlow.
Summing it all up, she said this has been a learning experience — one that is very much ongoing, and one that has helped her personally and professionally in innumerable ways.
“I’m a better nurse, and I’ve grown my knowledge base,” she explained. “And I now have a closer working relationship with many of the people here. Initially, I was joking that, when COVID is done, I’m going to change my cell-phone number and disable Halo [a messaging system used in healthcare] on my phone, because of all those calls I was getting. But through all those conversations and close meetings, we’ve become closer and have stronger relationships.”
Turning back the clock several years, Eboso said she took a somewhat winding route to her role as Infection Control and Prevention coordinator.
She came to this country from Kenya with the intention of studying business, but quickly segued into healthcare at Springfield Technical Community College and soon landed a summer internship at Mercy. When it was over, she was asked if she wanted to stay on as a nurse’s aide, and replied with a strong ‘absolutely.’ In many ways, she’s never left.
She went from nurse’s aide to nurse to clinical nurse supervisor to administrative nursing supervisor on weekend nights, a position that was eventually eliminated in 2015, prompting her to leave the Mercy system for close to a year.
She was offered a chance to return, and remembers the vice president of Nursing offering her her pick of positions.
Eboso chose Infection Control, something she had never done before, but intrigued her. She recalls her husband noting she was a quick study and saying, “If someone offers you an amazing opportunity and you’re not sure you can do it, say ‘yes’ —then learn how to do it later.” He also sent her an inspirational quote from Richard Branson to the same effect.
But no words, from her husband or Branson, could likely have prepared her for what her role became starting early this year, and especially after she started receiving those texts in the supermarket.
“The biggest thing that we saw with this whole thing was the fear. We were all thinking, ‘yes, we’ll take care of you, and we’ll treat you,’ but at the end of the day, we all had families and children that we were going home to. So while, yes, we all signed up for this, and this is what we do, people were still afraid — they wanted assurances that they could do their jobs and still go home and not bring this back to their families.”
They came from the Emergency Department director, the ED charge nurse, and the nurse tending to the patient directly. She put the shopping aside, was at the hospital in 10 minutes, and began addressing a situation that would become a microcosm of all that would come over the ensuing weeks and months.
“We had to call the Department of Public Health and get approval for testing because hospitals couldn’t do the testing themselves,” she explained. “So it was now calling the epidemiologist, waiting for a call back, talking to the physicians and nurse, looking at the patient, and waiting for DPH to call you back.”

Maggie Eboso’s work during the pandemic took her to every corner of Mercy Medical Center — and far beyond its walls.
“Information was changing almost every day,” she went on, while discussing what those first few weeks and months were like. “So as you’re building systems into your computer, you’re writing policies and going out in front of your staff to educate them on the new and updated information — and that was happening sometimes several times a week.”
One of her primary roles focused on educating staff on how to use PPE and become good stewards of that equipment, but also to help them separate fact from conjecture or assumption on what equipment was needed and, above all, how to keep themselves and their families safe from infection.
“The biggest thing that we saw with this whole thing was the fear,” she explained. “We were all thinking, ‘yes, we’ll take care of you, and we’ll treat you,’ but at the end of the day, we all had families and children that we were going home to. So while, yes, we all signed up for this, and this is what we do, people were still afraid — they wanted assurances that they could do their jobs and still go home and not bring this back to their families.”
And the onslaught of information coming from the media certainly didn’t help, she went on, because this information was often contradicting what she and others were telling staff members.
“When we told them, ‘all you need is a regular mask,’ they’d see people on TV wearing haz-mat suits, and they would ask, ‘why are they wearing haz-mat suits, and all you’re giving us is a mask?’ she recalled, adding that was this was just one of many “clashes and contradictions,” as she called them, that had to be dealt with.
“We had to call the Department of Public Health and get approval for testing because hospitals couldn’t do the testing themselves. So it was now calling the epidemiologist, waiting for a call back, talking to the physicians and nurse, looking at the patient, and waiting for DPH to call you back.”
While taking on this role of educator within the medical center, she also carried it out within the community as well, including several visits to the correctional facility in Ludlow, where she provided lessons in everything from how gloves provide a false sense of security — that’s why hand washing is still very important — to how to don and doff PPE.
Today, one of her concerns involves battling complacency and what she and many others are now calling “battle fatigue” — both inside the medical center and within the larger community.
She used the nurses’ lounges at Mercy as an example. “People are tired … people want to celebrate a birthday with a cake or share a pizza; they want to eat lunch with their friends,” she explained, adding that it’s part of her job to keep these employees diligent — and safe — by keeping the numbers down in those lounges and making sure there is adequate social distancing.
She joked that people are wary of even thinking about letting their guard down because, if and when they do, “Maggie will be walking in the door at just that moment.”
That mindset, real or not, is just one of many ways of explaining why she has become a Healthcare Hero during this very challenging year.
George O’Brien can be reached at [email protected]
She Became a Guiding Light at a Time of Pain and Darkness

Rabbi Devorah Jacobson
Rabbi Devorah Jacobson came to JGS Lifecare as its director of Spiritual Life in 2001. And, for the first 19 years or so, she came to work each day knowing exactly what her job was and how it would be carried out.
But when the COVID-19 pandemic reached this facility last March … well, she still knew what her role was, but she had to continually revisit that question about how to carry it out, because the answer had the potential to change seemingly every day.
“Every day, I would ask, ‘what does it mean to be a chaplain in a long-term facility during this time?” she told BusinessWest. “In the midst of the pandemic, when many of our residents are sick, many are going to the hospital, and many are dying, and staff are being called upon to work long hours and do things they weren’t necessarily doing before, like post-mortems, and where they’re risking their own health and lives every day they walked into the building … I’m observing all this and asking myself, ‘what is my role as the spiritual leader of this institution?’”
To say she would find new — and impactful — ways to answer that question would be an understatement.
Indeed, over the course of the past seven months, Jacobson has been a source of comfort to a number of constituencies, including staff members, residents, and their families. And she has done this through a number of means, everything from donning PPE and visiting sick and dying residents with COVID to rallying community organizations to send staff members meals of gratitude; from enlisting crisis therapists and mental-health counselors to offer staff free confidential counseling to creating prayer and inspiration cards for spiritual support; from helping raise awareness and funds for JGS’s Employee Assistance Fund to moving furniture, on at least one occasion.
“I’m part of the team,” she explained. “And I made a pretty quick decision — to be truly part of the team, 365 days a year, we do what we’re called upon to do.”
It is sentiments like this that prompted Susan Halpern, vice president of Development and Communications for JGS, who nominated Jacobson, to write that “our heroes are people we look up to and admire for their extraordinary actions and achievements. They are people we wish to emulate. Devorah’s countless acts of caring and loving-kindness, her concern for others, her efforts seeking justice for all, make her a standout candidate for the prestigious Healthcare Heroes award.”
“I’m part of the team. And I made a pretty quick decision — to be truly part of the team, 365 days a year, we do what we’re called upon to do.”
Indeed, as she talked with BusinessWest at a small table outside the Julian J. Leavitt Family Jewish Nursing Home — a nod to the precautions being taken to keep all those inside the facility safe — Jacobson repeatedly pointed toward the building and said, “the real heroes are in there.”
She was referring to the frontline workers who confronted a ferocious outbreak of COVID-19 in the early spring that would ultimately claim 66 lives and leave staff members fearful of what might happen to them, but still committed to carrying out their jobs.
In many ways, she pivoted within her role, from spending the bulk of her time with residents and families — handling everything from Jewish programming to pastoral care, including one-on-one visits — to now devoting most of it to those staff members fighting the COVID battle but also confronting the many other issues of the day.

A plaque has been placed outside the Julian J. Leavitt Family Jewish Nursing Home to honor those residents of the facility who lost their lives to COVID-19.
“Yes, I was continuing to meet with residents, although they were very frail and very sick, and yes, I was continuing to be in touch with family members, because they were unable to come into the building — I was able to give them a sense of how their loved ones were doing,” she recalled. “But much of the focus shifted to the staff.”
And it has remained there, months after the height of the tragedy, because the need remains — and is significant.
“I was just involved in a conversation with a nurse,” she said while speaking with BusinessWest. “She took me aside and said, ‘now that COVID has passed, many of us are dealing with PTSD [post-traumatic stress disorder]. I’m not sure what kind of help we need, but we need some help.’”
She has been providing such help, and in several ways, one of them being help in securing counseling for the many staff members impacted by the crisis.
“It was quite clear, as I was visiting the units and talking to staff, that there was a lot of trauma,” she recalled. “So what I wound up doing, with the help of a lot of great friends in the therapy world, was put together a therapy initiative for our staff. I had a list of about 30 mental-health counselors, trained in trauma and crisis counseling, who made themselves available for phone, Zoom, or otherwise, to be available for up to six hours, for free.
“I started making matches,” she went on, adding that maybe 20-25 staff members took advantage of the program. “Some of these people got sick, so for some of them, it was when they got back and had gone through all they had gone through with their own illness.”
Each day, she would arrive at the facility and ask herself how she could carry out her role, how she could help. And seemingly each day, there was a different answer.
It might be creating a new prayer and inspiration card — one of them says simply, “be the change that you wish to see in the world.” In response to George Floyd’s death and the Black Lives Matter movement, she held an all-campus moment of silence and urged individuals and the organization as a whole to seek ways to defeat bigotry and racism. In response to an on-campus arson attempt, she spoke up against hate crimes and anti-Semitism. On more than a few occasions, she helped box up the belongings of residents who had died as a result of COVID-19.
While Jacobson’s recollections of the past seven months and thoughts about her work certainly resonate, comments from others about the comfort and support she provided speak volumes about her impact during this time of crisis.
“My only regret was that I could not hold my mother’s hand. Devorah held her hand for me. She let me say goodbye to my mother … she was there to bridge the gap. It is because of Devorah that my journey was so peaceful.”
Halpern forwarded this comment from a family member: “Devorah went in to see my parents every day and she called me every day to give me updates. My only regret was that I could not hold my mother’s hand. Devorah held her hand for me. She let me say goodbye to my mother … she was there to bridge the gap. It is because of Devorah that my journey was so peaceful.”
Halpern also shared an e-mail from Lola White, an LPN and unit manager at the Leavitt Nursing Home, which was sent to her unsolicited. “Throughout this pandemic,” it read, “Devorah has always been there and ready to help in any way she could.
“One day, I was attending to a resident who lost the COVID battle,” it continued. “She immediately asked me, as she always did, if I was OK. Next thing I know, she was suited and booted, by my side, helping me. Before she helped me, I felt defeated. Her acts of compassion for me and every other staff member in the facility made it easier to cope … She set up meals, counselors, and even called and texted staff that were out sick or had a sick family member … I am looking for a way to thank her for everything.”
Needless to say, many people share that sentiment.
George O’Brien can be reached at [email protected]
This College Student Stepped Up and Passed an Important Test

Jennifer Graham
Jennifer Graham enrolled in the pre-medical sciences program — with a minor in psychology — at Bay Path University with the long-range goal of becoming a doctor.
But the events of the past seven months have changed her outlook — and her career pursuit — in a very meaningful way.
“I now want to go into nursing school,” she told BusinessWest. “Dealing with COVID as a whole and seeing what we’re going through as a country, I just want to pursue nursing and help people more. Doctors don’t get that one-on-one all the time, that patient contact, as much as a nurse does. After working with COVID and seeing what people really go through with sickness and even death, I want to be there — I want to be there to support these patients, help them out, and make them feel better as an individual with what they’re going through.”
What prompted this change? Some time on the front lines of the pandemic as a home health aide working for O’Connell Care at Home, a part-time job that became far more than that when she returned from a cruise — yes, a cruise — during spring break in mid-March.
Upon coming back to Western Mass. from that voyage to the Mediterranean, her job with O’Connell changed in a number of ways — everything from how care was provided in the home during a pandemic to where.
Indeed, in addition to going into the homes of the clients assigned to her, she was one of the first (and one of the few) to volunteer to provide care to the homeless at an outdoor COVID-19 triage facility established to care for potential positive cases among the homeless.
When asked why she signed on for this risky, month-long assignment in the middle of a pandemic, she replied simply, “there was an obvious need, and I just thought I could help — I thought I could do my part.”
“After working with COVID and seeing what people really go through with sickness and even death, I want to be there — I want to be there to support these patients, help them out, and make them feel better as an individual with what they’re going through.”
These comments from Michael Hynek, an HR generalist at O’Connell who nominated her to be a Healthcare Hero, echo that sentiment and put her work during the pandemic in its proper perspective.
“Having an aide like her, who is willing to accept any challenge, is vital when servicing our at-risk members in the community,” he wrote. “She makes everyone feel welcome and safe when administering care. Jennifer also enjoys the opportunity to learn about healthcare in many unique settings. Working outside of a hospital or facility can be very challenging, but she has embraced every challenge that has come her way.”

Jennifer Graham says her experiences during the pandemic, especially her work with the homeless, has prompted her to change her career goals; her new ambition is to become a nurse.
COVID-19 has provided her the opportunity to learn on many levels, and about many things. And it has also given her a new perspective on everything from the homeless population to her own career aspirations.
To tell this story properly, we need to go back to end of that spring-break cruise, which started and ended in Gotham. Suffice it to say the world, and Graham’s world, were much different places.
“While we were in the Bahamas, my phone was going off like crazy, and I was thinking, ‘look what we’re going home to,’” she recalled. “When we docked, New York was a complete ghost town; they took our temperatures and asked us a series of questions; if you had a fever, you had to stay on the cruise ship for two weeks. But no one had a fever.”
As for Bay Path, the campus was now closed, and it would not reopen for the balance of the spring semester. “There were no labs, no nothing; everything was remote.”
Then there was her day job, as she called it.
Looking for something that would provide both a paycheck and some rewarding work in what was becoming her chosen field, she became intrigued by the comments of some friends who worked at O’Connell’s who told her it was a great place to work. She applied late last fall, and started in December.
By the following March, she had settled in; she had a few clients assigned to her and also filled in when a colleague was out.
When she came back from vacation, that world changed as well. She was still seeing many of the same clients she did before COVID struck, but now, the work was different. It now entailed social distancing, mask wearing, and being extra diligent when it came to keeping the client and family members — and herself — safe.
“It was quite challenging at first — having to wear a mask all day was … different, and it was a new environment,” she recalled. “But after a little bit, you got used to it. And for the clients, it was difficult for them, because it was hard for them to understand what you were saying. I was thinking, ‘now we have to think differently and respond to them differently. I have to be much louder and slow my words; clients don’t like the mask.’
“Having an aide like her, who is willing to accept any challenge, is vital when servicing our at-risk members in the community.”
“I’ve been double-gloving,” she went on, referring to the practice of wearing two sets of gloves in the homes of those clients she has to help physically. “In some cases, they tell you not to double-glove, because it’s easier for your gloves to rip, but double-gloving for me has been a life saver.”
The bigger, even more significant change came with her decision to volunteer for work at the triage center created to care for the homeless population, work that became almost full-time as the spring semester ended and her schedule opened up.
“Anyone who had the virus or felt they had the virus came into these two large tents — they were essentially living there,” she explained, adding that individuals were tested on site and placed in two categories: PUI (patients under investigation), and the “COVID side,” where residents were housed in designated quarters based on whether they tested positive or negative.
Elaborating, she said there was an intake process, testing, and then the aides would bring them into a tent, make up a bed for them, get them something to eat, and help in any way they could. “If they needed anything, we were there for them.”
While a few people volunteered for work at the triage center, Hynek told BusinessWest, Graham’s commitment stood out.
“She really stepped up the plate when it came to transitioning away from the elderly care and into the homeless care and serving that vulnerable population,” he noted. “She took on a brand-new challenge, and I don’t think a lot of people would step up to the plate in that situation.”
As noted earlier, this work was a learning experience on many levels, and it also changed her perspective on the homeless population.
“This experience changed my mind on how I look at them,” she explained. “Being younger, I would look at a homeless person and say, ‘why don’t you just get a job?’ Working with them completely changed how I felt; I got to understand what it’s like for them — how much of a struggle it is for them on a daily basis.
Graham is back in school now, taking classes remotely while returning to the Bay Path campus for labs. She still works at O’Connell at a part-time basis, taking care of a few clients and double-gloving as always. The COVID-19 fight is far from over, but she has already absorbed a number of lessons that have helped her grow personally and professionally and given her that new perspective on what she wants to do with her life.
If this was a test — and she would say it has been, on a number of levels — then she has certainly aced it, becoming, in the process, one of the many Healthcare Heroes of 2020.
George O’Brien can be reached at [email protected]
Dedicated Team Rose to the Occasion and Took Care of Those in Need

The Nutrition Department at GSSSI
Several areas at the Greater Springfield Senior Services Inc. facility on Industry Avenue in Springfield are still sporting St. Patrick’s Day decorations.
They were put up early last March, and they remain there … well, because those who put them up haven’t been back to take them down.
Indeed, as the pandemic closed in and the state-ordered shutdown went into effect just before that holiday, the vast majority of GSSSI’s 250 employees began working remotely — and they have remained off site. But for some, working at home simply wasn’t an option. That’s because it’s their job to essentially provide nutritious home-delivered meals, or HDMs, as they call them, each day.
This small team of 10 essential employees stayed on and weathered the storm, if you will, and devised and executed a comprehensive plan to ensure those who need these meals get them, even though the senior-dining sites that were in operation had to shut down due to restrictions on large gatherings, and all meals have to be delivered to the home or picked up at designated ‘grab-and-go’ sites.
The creation of that new grab-and-go program underscores just how quickly — and effectively — the Nutrition Department at GSSSI was able to respond to this crisis situation.
“We knew we couldn’t leave people behind. There were people in need, and we had to come up with a plan to get them their meals.”
Indeed, the initiative involved everything from securing new caterers, including one that could prepare medically tailored meals, to establishing the sites; from partnering with the PVTA to deliver the meals to putting in place the protocols needed to ensure that meals were picked up safely.
Doing all that might normally take four to six weeks, said Heather Jolicoeur, community coordinator for GSSSI and a member of that team. Instead, they did it all in under two weeks.
All that sounds difficult enough, but remember, this was carried out in the middle of a pandemic, so there additional challenges and assignments on top of those one might expect:
• One of the food resources was shut down due to COVID-19, forcing those at GSSSI to track down a reliable and appropriate food source for Kosher meal recipients;
• A corps of volunteers had to be assembled, with CORI checks run on each individual due to the nature of the work;
• Temporary Meals on Wheels drivers had to be hired to fill in for regular drivers who had pre-existing conditions and couldn’t safely deliver meals every day;
• New policies for delivering meals with the least amount of contact from the drivers were put in place, further complicating the process; and
• As the crisis continued, new needs emerged, and HDM recipients were soon also receiving toilet paper, hand sanitizer, and other items, supplied by those in ‘chase cars’ following those delivering meals.
Jill Keough
“Each one of us felt very responsible about whom we were serving‚ and we were responsible to one another. So we really took social distancing very seriously. Many of us didn’t go to the supermarket for months because we didn’t want to risk bringing the virus into work.”
“Every day, there are emergencies; every day, the conditions change; every day, new policies and procedures are developed, implemented, and changed,” said Jolicoeur, putting the accent on the present tense. “Every day, all 10 of us work together calmly and focused on serving as many seniors as possible.”
As they talked about their experiences and what it meant to be part of this effort, those who are involved gave some unique perspective on all that has transpired over the past seven months, and underscored why this group is part of the Healthcare Heroes class of 2020.
“We knew we couldn’t leave people behind,” said Jill Keough, executive director of GSSSI, as she summed up the situation that unfolded in mid-March and the Nutrition Department’s detailed, and imaginative, response to the problem — or problems, to be precise. “There were people in need, and we had to come up with a plan to get them their meals.”
Before getting to this plan, though, Mary Jenewin Caplin, the now-retired Area Agency on Aging director, set the stage. Before COVID-19, she explained, GSSSI served more than 900 clients who rely on HMDs each day. Prepared by caterers each day, the meals were delivered to some homes, but also to 14 senior-dining sites across the region, where clients could not only dine, but enjoy one another’s company and camaraderie.
When the pandemic struck, those dining sites had to close, for obvious reasons, but the need remained, and now, meals had to be delivered to the home, requiring the hiring of more volunteer drivers and new ways to get meals into the hands of those who needed them.
The plan that emerged came together very quickly, out of necessity, said Mike Young, an HMD supervisor, and it would have to incorporate a number of changes to how things had been done, but could no longer be done in the age of COVID.
“The biggest concern was that clients didn’t even want to open their doors anymore,” he explained. “We had to worry about how we would see them, how we would get them the meals, how would we keep the clients safe, how would we keep the drivers safe. Our drivers were used to going into someone’s house, putting the meal in the refrigerator, giving it to them on the couch, or putting it on the kitchen table. Now, we’re trying to get a driver to give them a meal, stay six feet apart, and maybe not even have the door open; there were a number of challenges to overcome.”
“None of the drivers could fit all that food into one car. We had some people call and say, ‘stop, I have no more freezer space”
Tracy Landry, another HMD supervisor, agreed, noting that, to keep both drivers and clients safe, a series of new protocols were put in place, including single-use plastic bags for deliveries, masks, hand sanitizer, and other steps.
“We had more meetings than you can imagine when we first this started,” she recalled. “Every day was different, and each day it seemed that there was a new challenge.”
Indeed, and as new challenges emerged, this small but dedicated team found ways to meet them. At the top of the list of challenges was keeping everyone safe, and for this team of 10, that meant taking extraordinary measures themselves.
“Each one of us felt very responsible about whom we were serving‚ and we were responsible to one another,” said Keough. “So we really took social distancing very seriously. Many of us didn’t go to the supermarket for months because we didn’t want to risk bringing the virus into work.”
As noted, one of the real concerns for the Nutrition Department team was keeping the drivers — most all of them older and in the high-risk category — out of harm’s way.
“My concern the whole time was the drivers — they’re all in that danger zone,” Young said. “Every day, they were asking, ‘what’s going on?’ You could tell they were concerned, and I was concerned for them. The last thing I wanted to see was someone catch something. To me, they’re the real heroes in this; they were out there every day doing it.”
At the height of the crisis, additional volunteer drivers had to be hired to handle what became larger deliveries, said Landry, noting that those at GSSSI were determined to help seniors stock up on frozen meals to make sure they had enough food in the home.
“None of the drivers could fit all that food into one car,” she explained, adding quickly that these efforts to help clients stock up were more than successful. “We had some people call and say, ‘stop, I have no more freezer space.’”
And, as noted, the help being provided soon extended beyond food. Indeed, as calls came in from the public asking how they could volunteer and help serve the seniors, some were pressed into service following the food-delivery vehicles in so-called chase cars stockpiled with toilet paper, hand sanitizer, and other items the client might need.
But food was the primary focus, said Kate Senn, Nutrition program director, adding that the creation of a grab-and-go program certainly helped GSSSI effectively meet that growing need. To put the matter in perspective, she noted that, in January, prior to COVID-19, GSSSI was providing 3,352 meals for congregate dining sites. In August, it was providing 4,581 meals via the grab-and-go program.
Those numbers help tell the story, but only a little. The tireless work and dedication to serving clients — while also keeping everyone safe at a time when similar programs in other states and other parts of this state had to shut down because of positive cases — are what really make this story happen.
The 10 that stayed behind have left the St. Patrick’s Day decorations up, perhaps thinking they will be appropriate in a few months again anyway. But more to the point, they just haven’t had any time.
They’ve been too busy getting HDMs to all those who need them. They’ve been too busy doing the work of true Healthcare Heroes.
George O’Brien can be reached at [email protected]
This Administrator Provided a Steady Hand in Rough Seas

Helen Gobeil
Helen Gobeil had recently relocated to Western Mass. from the other side of the state, and was looking for work.
She remembers seeing the small, as in small — maybe two lines — ad in the paper for an administrative assistant at Visiting Angels in West Springfield, a home-care provider, and becoming intrigued enough to apply — and prevail in that search.
She would eventually grow into the position and became adept at handling the many responsibilities within the job description, said her boss, Michele Anstett, president and CEO of the company, adding quickly that this was a good thing because all those talents would be needed when COVID-19 arrived in Western Mass.
Indeed, every aspect of this job, from recruiting caregivers to consulting with new clients; from matching caregivers with these clients to scheduling regular care and coordinating care in emergency situations, would become more difficult. Much more difficult.
And there would be new responsibilities added to that already-long list, including the daunting task of providing PPE for those caregivers and providing a compassionate ear to family members coping with something they would struggle to get both hands around.
Anstett summed up Gobeil’s work during this ultra-challenging time by describing her as a “hidden hero of COVID-19.”
By that, she meant she worked mostly, but not exclusively, behind the scenes and not on the front lines. But her contributions to what is an ongoing fight to carry on business in the middle of a pandemic, while keeping both employees and clients as safe as possible, are worthy of that adjective ‘heroic.’
“Not only has she handled this crisis with extraordinary competence and resilience,” Anstett wrote in her nomination, “she has remained a positive force in the lives of clients, their families, and caregivers.
“Not only has she handled this crisis with extraordinary competence and resilience, she has remained a positive force in the lives of clients, their families, and caregivers.”
“COVID-19 has not only presented physical challenges, but also mental ones, including severe anxiety and depression and exacerbating loneliness, isolation, and sleep problems, particularly in the senior population,” she went on. “To this end, Helen has not only served to protect the health of seniors across Western Massachusetts, but she has also given peace of mind to the families, seniors, and caregivers.”
To put these phrases ‘positive force’ and ‘peace of mind’ in their proper perspective, we turn back the clock to last March 23, when Gov. Charlie Baker imposed his lockdown. At Visiting Angels, staff members packed up and prepared to work remotely for what would be three months. But as they did that, Gobeil, in particular, had to develop detailed plans for providing care in the middle of a pandemic, at a time when people, and especially seniors, were wary about letting people into their homes.
For many, though, home care is an essential need, so they had to let people in. But before anyone went in, Gobeil and Anstett would conduct a risk assessment for both clients and caregivers within a given match.
“We would go down the list, and give each client a number — ‘1’ being the least at risk, and ‘3’ the highest,” Anstett noted, adding that there are more than 60 clients on average at any given time. “We would talk about each caregiver and each client and discuss how to keep them safe; if there was a facility that had COVID, we wouldn’t go into that facility.
“Helen stayed on top of all this,” she went on. “She would talk to every single caregiver and find out where they were going, where they had been, whether they had another job … and she would just cut it right down, every day.”

Helen Gobeil with Michele Anstett, president and CEO of Visiting Angels West Springfield.
Meanwhile, there would be new protocols concerning cleaning within those homes and other steps to control the spread of the virus.
“These were things we did all the time,” Gobeil explained. “Caregivers just had to be extra, extra cautious about what they did.”
And she had to be extra cautious and extra diligent about who else was going into these homes. With that, she relayed a story that brings this element of her assignment into perspective.
“The daughter of one of our clients showed up from Florida — and that was an event,” she recalled. “She didn’t tell anyone she was coming, and went into the home to a bedbound client with our caregivers in the house. She didn’t quarantine — she went from the plane to this home.
“This was a 24/7 case, and we pulled out of that house immediately,” Gobeil went on. “I said, ‘it’s her or us; until she’s gone, we’re out!’ She went to a hotel that night and left the next morning. Another daughter went in and cleaned top to bottom.”
Beyond delivering some tough love in situations like that, she has also been providing some compassionate outreach to family members of clients, including one who had to cope with the death of a loved one at a time when the grieving process, like everything else, was made different by COVID-19.
“Often, I tried to bring them to a peaceful moment,” she explained. “In this woman’s case, her mother was dying, and she was very anxious about the whole thing. I said to Michele one night, ‘I’m going to see the client, and I’m going to take some time with the daughter,’ and I did. And after her mom passed, she came here, stood in the doorway, said said, ‘please tell me I can come in — I just owe you a big hug.’”
There have been myriad other tasks and challenges as well, including the matter of simply securing needed PPE for her caregivers. It was very difficult to procure items such as masks and gowns in the beginning, and it’s still a challenge, she said, adding that Visiting Angels and other providers have certainly been helped by Gowns 4 Good, the national effort to collect graduation gowns.
“As we started to get them in, the stories that accompanied them … they were incredible,” said Gobeil. “Notes from high-school graduates, class of 2020, including some from West Springfield, who couldn’t have their own ceremonies — they were heartwarming. We were crying.”
“Often, I tried to bring them to a peaceful moment.”
Meanwhile, another stern test, especially after the federal stimulus package was passed, was hiring caregivers. Indeed, many solid candidates for such jobs were in a position where they were making far more in employment than they could as a caregiver — so they stayed unemployed.
“In the beginning, we couldn’t get anyone to answer our ads,” she recalled. “But we made it through that rough patch, and now, a lot of people are eager to get back to work.”
One of her priorities now is to keep both her caregivers and their clients diligent as the pandemic enters its eighth month of impacting virtually all aspects of life as we know it.
Summing up what it was like — and is still like — she said, “it just multiplied the concern and the vigilance, and the stress was unbelievable, every day. And it is still like that. Every day.”
Coping with all this was certainly not in whatever job description was part of that tiny ad she saw more than a dozen years ago now. And it is certainly not what she signed up for.
But as this job changed with COVID, Gobeil rose to the occasion, accepting each new challenge with diligence and ample respect for her ultimate responsibility — the health and well-being of both her caregivers and clients.
Call her a ‘hidden’ hero if you like, but her hard work and dedication are certainly not lost on anyone she has been involved with during this pandemic.
George O’Brien can be reached at [email protected]
While This Shelter’s Protocols Changed, Its Mission Never Did
 The metaphor is an easy one to draw.
The metaphor is an easy one to draw.
“If COVID was the invading army, all of us here — every one of us — had to set the wall and hold the wall and make sure folks were going to be safe,” said Keith Rhone, Operations director at Friends of the Homeless in Springfield, a program of Clinical & Support Options (CSO).
The reality, however, was much more complex. In its dorms, its kitchen, and places where clients meet therapists, clinicians, and other staff one on one, FOH was tasked, back in March, with implementing social distancing and a host of other protocols aimed at keeping everyone safe — both those delivering a broad range of services and those receiving them — while never shutting those services down.
That they did so, and how, makes the entire team true Healthcare Heroes.
“People have to gather here, so we’re potentially a hot spot. All the credit goes to the people who kept it from being that.”
“In some ways, we can’t do anything differently,” Clinical Director Christy O’Brien told BusinessWest. “We’re never going to shut down; we’re never not going to be here. Despite the social distancing we had to do, we’re never not going to be close to our people — not necessarily physically, of course, but we still need to know how they’re doing, how we can help, all those things. Where other places were forced to move to telehealth, that’s never going to work for us. The needs are still the needs.”
Those needs encompass not only shelter, but clinical services, such as mental-health and substance-abuse recovery coaching and therapy; housing — FOH has a number of lease-holding tenants; three meals a day; clothing and toiletries as necessary; transportation and delivery services; prescription pickups; case management … as Rhone put it, “the job here is whatever it takes.”
COVID-19 didn’t arrive at an ideal time, said Bill Miller, vice president of Housing and Homeless Services — not that there’s ever a good time for a global pandemic.
“We were coming out of a winter where we served more people and were more full than we had ever been in our history,” he recalled. “So it was a tough winter, and what the pandemic required was a complete shift in our mindset because our inclination and our mission has always been the same: how do we serve as many people as possible? So we wanted to continue to serve in the same way, but we had to adopt a whole new style.”
Among the changes, picnic tables and tents were erected outdoors — spaced apart — to accommodate distanced meal lines. Volunteers, who are instrumental in the service of FOH meals and other activities, were temporarily suspended. In the dormitories, some beds were removed, with overflow space employed in the dining room. Partitions went up, and guests were arranged head to toe when sleeping.

Some of the leadership team at Friends of the Homeless, who had to quickly figure out new protocols in the spring while continuing to serve clients at the same level as before.
Additional temporary staff were hired to more regularly and thoroughly sanitize spaces, and hand-sanitizer stations were mounted throughout the campus. Dozens of donors and staffers designed and sewed homemade cloth masks so that each shelter guest would have reusable, washable masks.
Meanwhile, from the pandemic’s earliest days, before on-site testing became available, temperature screenings and interviews were conducted to alert the team to early signs, and as the situation progressed, Baystate and Mercy medical centers were quick to work with FOH on testing.
CSO also staffed and managed large tent facilities, which were erected in partnership with the city of Springfield and served as emergency accommodations in the event of positive cases (see the related story of another Healthcare Hero, page xx). When another shelter in the city needed to close due to guests testing positive, the CSO team was able to quarantine those who had been at risk and refer those who ended up testing positive to state-run MEMA isolation sites. FOH further assisted many of those individuals once their isolation periods were completed.
Why was all this critical? Simply put, while COVID-19 has swept through homeless populations in Boston, Worcester, and other cities, homeless individuals in the Greater Springfield region have been largely spared, thanks to the quick — dare we say heroic — work of the team at Friends of the Homeless.
“People have to gather here, so we’re potentially a hot spot. All the credit goes to the people who kept it from being that,” Miller said, adding that “there wasn’t one person who backed out, who wasn’t going to show up for work. We have a dedicated team who have been here for a long time. It was just incredible how everybody showed up.”
“I like the fact that we work in an environment that cares about people.”
It wasn’t lost on Miller that many people working at Friends of the Homeless fall into high-risk categories when it comes to COVID-19. “To have people come into work anyway is just striking.”
“Everyone came in and suited up and did the work,” added Delphine Ray, manager of Case Management Services. “They didn’t hesitate. This is our home away from home, and, by the grace of God, we managed to pull through.”
Dave Ware, men’s shelter manager, said he had many concerns about to manage the social-distancing aspect of the pandemic at FOH. “They really came together to figure out how to manage that in the dorms and kitchen. They came up with a good strategy to handle the social-distancing part.”
It wasn’t always a top-down strategy, Miller added. “There was a fad in business management some years ago — idea-driven organizations. That meant the ideas came from staff at all levels. That’s what we saw here. ‘What if we try this?’ ‘OK, let’s do that.’ Because this was something we’d never seen before, and we didn’t know what to do. And it ended up going well. Everybody was on high alert, and everyone had ideas.”
O’Brien also praised clients of Friends of the Homeless for taking the pandemic seriously and getting tested in the early days, before much was known about the virus and they were already preoccupied with some very real concerns, from mental health to lack of housing. “COVID wasn’t a primary concern for a lot of people. But they jumped on it when informed.”
He recalled warm moments, too, among upsetting ones — “incredible moments of humanity, seeing people come together in a time of crisis and fear. It was very genuine.”
That said, the need for the broad array of services provided by Friends of the Homeless to hundreds of people every day remains persistent, as does COVID-19 itself, as the cold weather approaches — not that those needs go away in the warmer months, Miller said.
“There may be peaks and valleys of needs; it’s not predicated only on cold weather. We used to see more of a lull in summer, but not so much anymore. And when times are hard economically…”
He didn’t have to finish that thought to register his point, which is, the tougher a community’s social and economic challenges, the more necessary FOH becomes.
“I like the fact that we work in an environment that cares about people,” Ware added. “When you look nationally and globally, you see so many people suffering, homeless, without food. We’re just a small place that takes care of those needs, but nationwide, so many people are suffering in this way. I’m proud to work in a place that takes care of people who need it. We’re one of the only places around here that does it on the level we do.”
As noted earlier, this is not an organization that can just shut its doors to the ‘invading army’ of COVID-19.
“We’re home for many people,” Miller said.
“And if we don’t do it,” O’Brien added, “who will?”
Joseph Bednar can be reached at [email protected]
Healthcare Heroes 2020 to Honor the Heroes of COVID-19
Since the phrase COVID-19 came into our lexicon, those working in the broad healthcare field have emerged as the true heroes during a pandemic that has changed every facet of life as we know it. And over the past several months, the world has paid tribute to these heroes, and in all kinds of ways — from applauding in unison from apartment-complex windows to bringing hot meals to hospital and nursing-home workers; from staging parades in front of these institutions to donating much-needed personal protective equipment (PPE).
BusinessWest and its sister publication, the Healthcare News, will pay tribute in their own way, by dedicating our annual Healthcare Heroes program in 2020 to those who are have emerged as true heroes during this crisis. We invite you to nominate one, or several, for what has become a very prestigious honor in Western Mass. — the Healthcare Heroes award.
Here are some examples of those heroes:
- Doctors and nurses;
- ER nurses, orderlies, techs, triage, reception;
- EMTs;
- Police and firefighters;
- Nursing-home staff
- Administrators leading the efforts to battle the pandemic;
- End-of-life care providers;
- Individuals and groups from our community who have stepped up to help healthcare workers with everything from hot meals to PPE;
- Companies that have pivoted and commenced production of materials such as PPE to help those in healthcare confront the pandemic; and
- Scientists working behind the scenes to develop a vaccine or new types of PPE.
These are just a few examples, and there are a myriad of others.
To assist those thinking of nominating someone for this honor, we are simplifying the process. All we desire is a 400-500-word essay, and/or video entry explaining why the group or individual stands out as an inspiration, and a truly bright star in a galaxy of healthcare heroes. These nominations will be carefully considered by a panel of independent judges, who will select the class of 2020.
Judging
The judging process will commence July 2020 and be completed by end of July 2020. Nominees cannot serve as awards judges. All eligible nominations received will be judged by a panel of health care industry experts whose evaluations will determine winners of the “Healthcare Heroes” Awards from among the nominees under consideration.
Nominations
Nominations must be submitted via the designated online form. Mail-in nominations will not be accepted. Nominations may be submitted beginning December 2019 and must be received no later than 5 p.m. Eastern Standard Time on July 1, 2020.
Notification and Recognition
BusinessWest plans to notify the winners of the “Healthcare Heroes” Awards by August, 2020 and will be profiled in the September 14 edition of BusinessWest and September issue of Healthcare News. Winners will be invited to attend the “Healthcare Heroes” Awards gala scheduled for Autumn 2020 at the Sheraton Springfield One Monarch Place Hotel.
Eligibility
- Nominees must work in either Hampden, Hampshire, Franklin, or Berkshire county and organization nominees must have offices in Hampden, Hampshire, Franklin or Berkshire county (may be for-profit or not-for-profit).
- Nominations may be self-nominated or nominated by another person.
- Nominees cannot be a member of the judges’ panel or member of the judges’ immediate family.
If using mobile device to submit nomination, please make sure your phone is in Portrait view mode.
Submitting multiple duplicate nominations does not enhance your chances of winning.





























































































































































































































































































































































































 Since BusinessWest and its sister publication, the Healthcare News, launched the recognition program known as Healthcare Heroes in 2017, the initiative has more than succeeded in its quest to identify true leaders — not to mention inspiring stories — within this region’s large and very important healthcare sector.
Since BusinessWest and its sister publication, the Healthcare News, launched the recognition program known as Healthcare Heroes in 2017, the initiative has more than succeeded in its quest to identify true leaders — not to mention inspiring stories — within this region’s large and very important healthcare sector.