Aging in Place

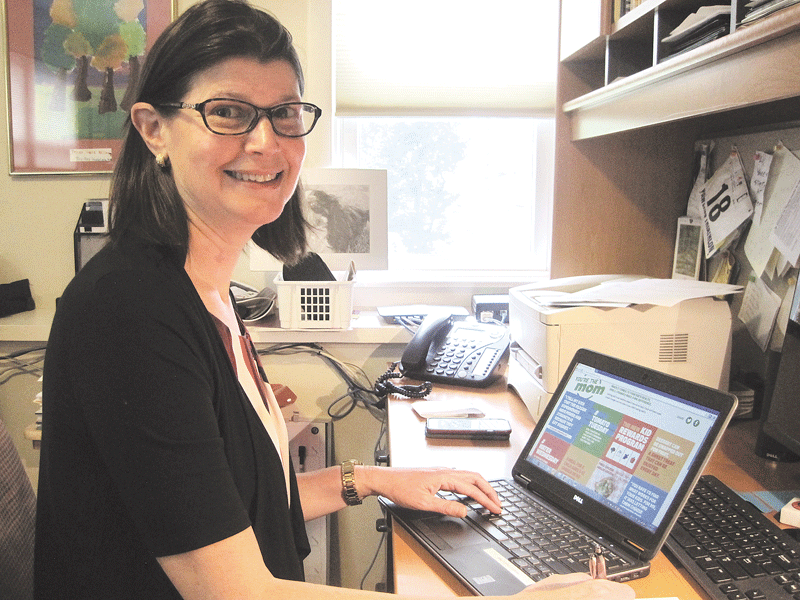
Suzanne McElroy says it’s important to match a family with the right caregiver to ensure there’s a comfort level on both sides.
As the Baby Boom generation continues to advance into the golden years, the demand for home care continues to rise, as families embrace a model that keeps seniors stay in their homes while helping them with everyday needs. That means the need for qualified caregivers is rising, too — and it’s not always easy to find them.
Home care is a far cry from, say, plumbing, Suzanne McElroy says. Sure, both careers require specialized skills, but not a lot of plumbers are turned away because they just don’t … feel right.
“I’ve often tried to compare this to other industries, and you can’t,” said McElroy, owner of Home Instead Senior Care in Springfield. “A plumber can come in and fix your pipes, and you don’t have to worry about what they look like or smell like, or how they talk; they just come in and fix your pipes. But I’ve had caregivers rejected for silly things, like a tattoo in the wrong place, or things I’m not legally able to consider, like age, race, or religion.”
Paul Hillsburg, owner and president of Amada Senior Care in West Springfield — who left financial services for a career in this fast-growing field — has observed similar difficulties matching caregivers to families, starting with his own life.
“I saw the challenges we had with my mom in finding qualified caregivers,” he said, noting that she utilized home care in the early stages of her dementia. “My dad fired the first seven. I realized that was an important part of providing care in the home — the personalities need to match. So we take a personalized care approach.”
After all, McElroy said, she has to consider things from the family’s perspective, and why they need a certain comfort level with someone who will be spending lots of time in the home. “It’s not like fixing pipes and leaving; they’re going to be staying and sitting with your mom.”
SEE: List of Home Care Options
The problem, both she and Hillsburg, noted, is that the challenge of making those matches, plus the surge of Baby Boomers into their senior years — around 10,000 are turning 65 every day, on average — are ratcheting up the pressure on home-care agencies to find and retain talent.
“More and more people want to stay at home, and hospitals are actually suggesting home care during discharge,” Hillsburg said. “People want to age in place, to be at home, where their family can come and visit, and where they feel more comfortable.”
Home-care services run the gamut from companionship and household help to assistance with ambulation and medical needs, and the popularity of this option continues to grow, creating worries that demand will eventually outstrip the number of qualified caregivers. That means competition among agencies, which are bringing myriad tools to bear with the goal of helping seniors live as independently as possible.
The Right Choice?
McElroy, who has lectured many times on the topic of choosing a senior housing plan, outlined several considerations that families must discuss, including:
• Physical needs, including activities of daily living — from shopping, cleaning, cooking, and pet care to more intensive help with bathing, ambulating, and eating — and medical needs, which could arise from a sudden condition, such as a heart attack or stroke, or a more gradual condition that slowly needs more care, such as Alzheimer’s disease.
• Home maintenance. “If you’re living alone, your current home may become too difficult or too expensive to maintain,” she noted. “You may have health problems that make it hard to manage tasks such as housework and yard maintenance that you once took for granted.”
• Social and emotional needs. As people age, their social networks may change, with family and long-time friends no longer close by, and neighbors moving away or passing on. At the same time, they may no longer be able to drive and have no access to public transportation. The desire to be around a community of friends and take part in social activities may be paramount.
• Financial needs. “Modifying your home and long-term care can both be expensive, so balancing the care you need with where you want to live requires careful evaluation of your budget.”
The answers to these questions may very well point to assisted living as a better option than home care, but others may be able to age in place, accessing home-care services to better manage activities of daily living, while still enjoying the comfort and security of a residence they have lived in for years or decades.
Aging in place is a less effective senior-housing option once your mobility is limited. Being unable to leave your home frequently and socialize with others can lead to isolation, loneliness, and depression. So, even if you select to age in place today, it’s important to have a plan for the future when your needs may change and staying at home may no longer be the best option.”
“You may also be able to make home repairs or modifications to make your life easier and safer, such as installing a wheelchair ramp, bathtub railings, or emergency response system,” McElroy said.
Home care is a good option, then, for people who can access transportation; live in a safe neighborhood and in a home that can be modified to reflect changing physical needs; don’t have an overwhelming burden of home or yard maintenance; have physical or medical needs that don’t require a high or specialized level of care; and, perhaps most important, have a network of nearby family, friends, or neighbors.
“Aging in place is a less effective senior-housing option once your mobility is limited,” she added. “Being unable to leave your home frequently and socialize with others can lead to isolation, loneliness, and depression. So, even if you select to age in place today, it’s important to have a plan for the future when your needs may change and staying at home may no longer be the best option.”
Individuals and families who do choose home care, Hillsburg said, still have to overcome that initial reluctance to invite a stranger into their home.
“When I meet clients, I do my own personal assessment, trying to link their personalities with the personality of the caregiver,” he explained. “And when the caregiver goes to the family’s home for the first time, I meet them there and introduce them to the family, make sure there’s a comfort level there.”
Hillsburg said his company, part of a national network of Amada franchises, also performs extensive background screening — credit history, DMV records, criminal records, sex-offender registries — to ensure client safety, and also assists people trying to figure out how to pay for care, whether that’s a long-term care policy, veterans’ benefits, reverse mortgages, even life-insurance policies that can be sold back, swapping death benefits for current care.

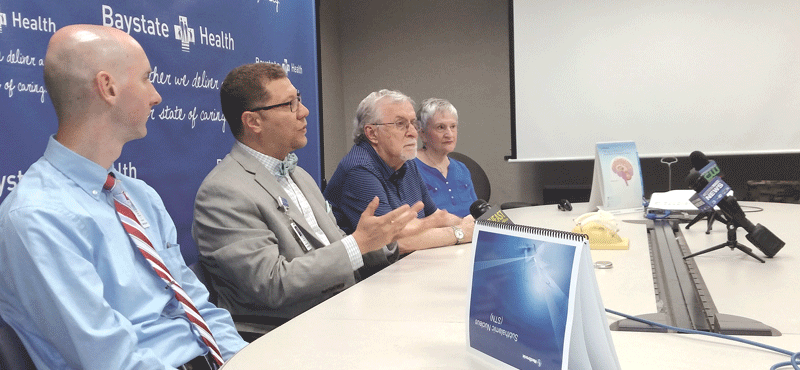
Paul Hillsburg says the biggest challenge for home-care companies is finding and retaining quality caregivers in an increasingly competitive arena.
But to build a team of reliable caregivers at a time when the competition for talent is becoming fiercer by the month, a company has to make sure they’re paid well and happy in their jobs, he told BusinessWest.
“It’s a very, very competitive field. The biggest challenge going forward is going to be finding and retaining good, quality caregivers. That’s why we provide 20 hours of free training, or more, if they want it, to all our caregivers, and we pay them while they’re in that training,” he explained. “They want to be treated like a person and respected.”
Cost is still a major consideration for families, McElroy said, especially when agencies have to pay their caregivers competitively. While lower-income services are available through Medicaid and MassHealth, home care still isn’t within reach of everyone who needs it. “That’s only going to change in importance when enough people feel this pain, or the right people feel this pain.”
High-tech, High-touch
At the same time, Hillsburg said, home care continues to absorb technological advances that make it easier for families and companies to assess results, from an online portal Amada offers called Transparent — which allows families to see which duties a caregiver has performed — to a GPS system that lets the company know whether caregivers show up at the right place and time.
Meanwhile, the company’s Discharge Admissions Reduction Team (DART) works with care managers to negotiate transitions between hospital and home care with the goal of reducing hospital readmissions.
“The need for care is going to continue to increase for the next 30 years before we hit the end of the Baby Boom generation,” Hillsburg said by way of explaining the ways companies are honing their services to meet the needs of this population.
Still, at the end of the day, McElroy said, families are most concerned with whether the caregiver increased their loved one’s quality of life. She recalled one client who requested someone versed in quilting, to help her thread needles and otherwise allow her to continue enjoying her favorite pastime.
“That’s the heart of what we’re doing. Yes, we’re helping them out of bed and into the shower, but if we can help someone live the live they want, that’s what’s driving the spirit of our business,” she explained. “It’s hospitality; it’s customer service. You have to love what you’re doing. You have to love the mission and love the work.”
After all, “whenever I have someone raving about a caregiver, it’s not because they came in for a few hours and got the job done; it’s because they made a difference in someone’s life,” McElroy said. “They can be doing the grossest thing ever, but when they leave, if the person takes their hand and says, ‘I don’t know what I would do without you,’ they’re flying. They can’t wait to go back.”
Joseph Bednar can be reached at [email protected]










 When Bec Belofsky married Lee Shuer, she had no idea he had hoarding disorder.
When Bec Belofsky married Lee Shuer, she had no idea he had hoarding disorder.


 SPRINGFIELD — In a time of change for what, until recently, was known as the Assoc. for Community Living, the organization’s passion and innovative spirit will remain constants, its executive director says.
SPRINGFIELD — In a time of change for what, until recently, was known as the Assoc. for Community Living, the organization’s passion and innovative spirit will remain constants, its executive director says.