Wave Dynamics

Since they started entering the world just after World War II, the Baby Boomers have influenced society in general, and the business community in particular, in all kinds of ways. The same is true when it comes to the healthcare sector, especially as the oldest members of this huge and proud generation turn 75. The impact of such a large and aging group can be seen in everything from hearing practices to the many facets of the long-term care system. And in some ways, COVID has provided a preview of what it is to come.
As she talked about the massive Baby Boom generation, how its oldest members turn 75 this year, and about how almost all the Boomers could now be classified as senior citizens, Dr. Maura Brennan summoned a phase she attributed to her mother, but which she uses often as well: “No one gets out of life alive.”
She used those words to convey the thought that, while this Baby Boom generation may in many ways be healthier than those that preceded it — fewer smokers and more exercisers, for example — and it has enjoyed access to better healthcare and innumerable advances in treatment, from artificial joints to improved cancer care, its members will eventually see their health decline, and they will need increasing amounts of care. And many already do.
“I don’t believe this generation, which I am part of, will readily tolerate limited access to the best care.”
While Brennan — a 70-year-old geriatrician and palliative-care physician — says people being able to live longer is in itself a success story, it has also become a challenge, for today, and especially tomorrow.
Which brings us back to those oldest Boomers, those born just after World War II, who turn 75 this year. That’s the age when, statistically, people begin to see their needs for healthcare increase, said Brennan, adding that, as one might logically assume, when a large number of people hit that threshold all at once, the system will be taxed — in all kinds of ways.
“As one might imagine, it’s going to impact virtually every sector and specialty, with the possible exceptions of OB and pediatrics,” she explained. “We’re going to see increasing numbers of older people; not all those folks are going to be frail and complicated, but there will be an increasing number of people with multiple medical problems.

Dr. Maura Brennan says the healthcare system is struggling to meet demand for direct-care workers, and the situation might get worse.
“The numbers and the complexity will rise,” she went on. “And it will impact every area of healthcare, with probably the biggest impact being in home care and nursing-home care because, personally, I don’t believe this generation, which I am part of, will readily tolerate limited access to the best care that’s going to allow them to stay in their homes and communities as long as possible.”
Mary Flahive-Dickson, chief operating officer at East Longmeadow-based Golden Years Home Care, agreed. She said the milestone age being reached by the oldest of Baby Boomers provides an opportunity to look hard at what’s in store for the healthcare system and ask the question: is it fully prepared for the challenges to come? And, if not, what needs to be done so it might be better prepared?
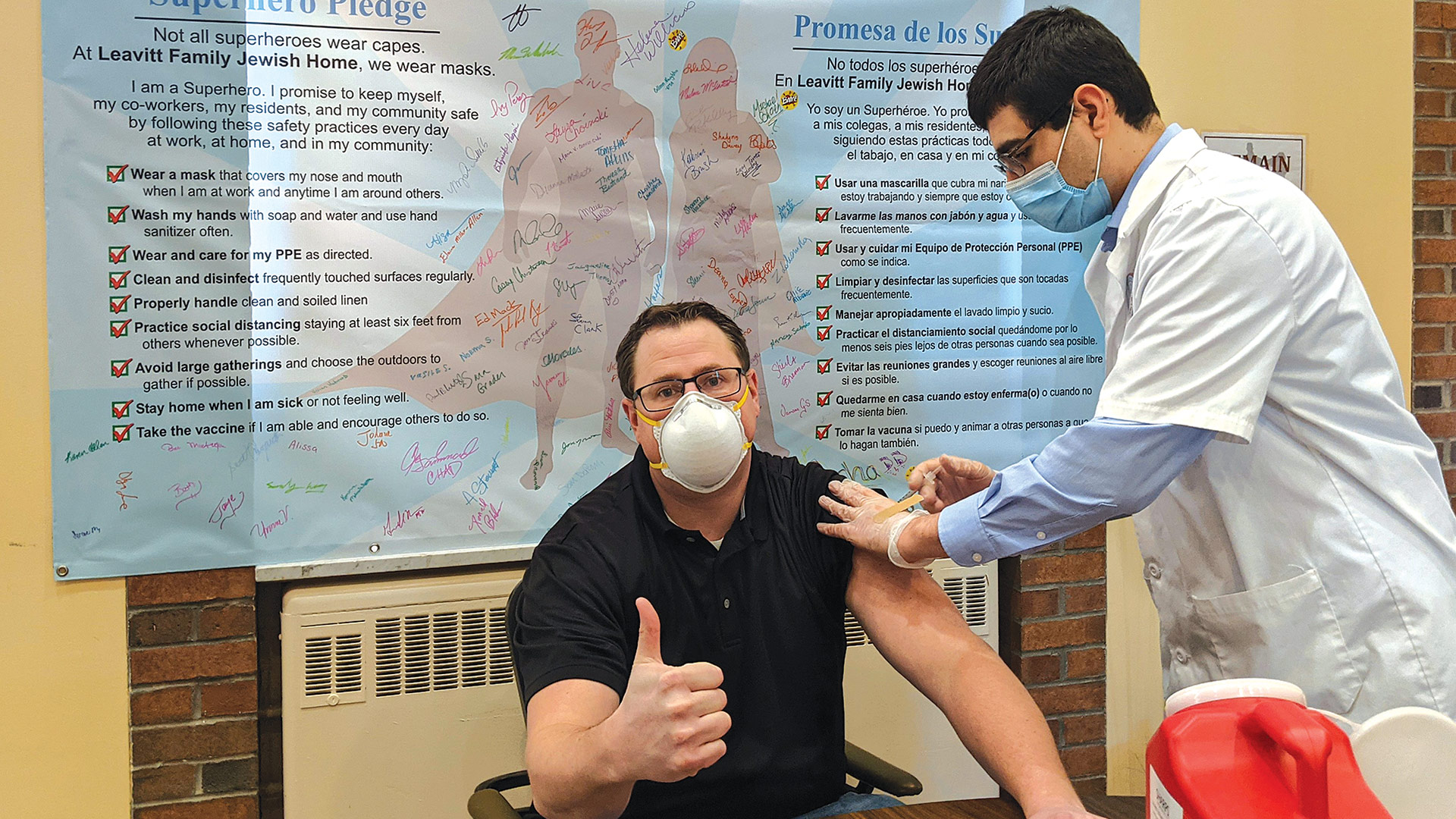
In many ways, Flahive-Dickson said, the COVID-19 pandemic has actually provided a preview of sorts for what’s coming as this large generation ages, with regard to everything from telehealth to the way the overall healthcare system was tested by sheer volume of cases and even vaccination efforts, to the manner in which the need for home-care services is growing.
During the pandemic, this need was fueled by growing fears of nursing homes and other senior-living facilities. Many of those fears still persist, but for Baby Boomers, by and large, the greater issue is simply wanting to remain independent — and in the home — as long as possible.
Eric Aasheim, a certified senior advisor and owner of Oasis Senior Living of Western Massachusetts, agreed. Aasheim, who assists seniors and family members through the complex process of transitioning from home to senior-living communities across this region, said the entire long-term-care sector will be tested by the aging of this generation.
“What I see, and what I worry about, is that the long-term-care system — and that includes in-home care, nursing homes, and assisted living — is just not ready for the sheer volume of patients and residents that they’re going to have,” he told BusinessWest. “And even though these individuals living longer and their resources are being depleted, there are so few places that have any kind of programs for low-income seniors. Unless something dramatically changes in terms of the number of assisted-living facilities that can serve low-income residents, there won’t be needed options for seniors.”
Meanwhile, besides sheer size and that sense of independence and not wanting to rely on others, the Baby Boom generation boasts some other characteristics as well, including what could be described as denial when it comes to getting old and admitting some aspects of their health have deteriorated.
“That’s not a disaster or a tsunami. That’s one of the greatest success stories in modern history; people are able to live longer and enjoy their lives better.”
And that’s why, even though she is generally seeing more patients than she was years ago, Dr. Susan Bankoski Chunyk, an audiologist, says she’s seeing a continuation of, and perhaps even an exacerbation of, an annoying trend whereby people will put off seeking help for their hearing years after they acknowledge they have a problem, due to lingering perceptions about hearing aids making people look old and feeble, even though modern technology has changed that landscape.
And that’s just one example of why there are still many question marks about how and to what degree this generation will present challenges and opportunities moving forward.
Age-old Challenges
Before getting into any real detail about the Baby Boom generation and its advancing age, Brennan wanted to set the proper tone for the discussion.
Indeed, she told BusinessWest that years, if not decades, of talk about a ‘silver tsunami’ have succeeded in casting discussion about the aging Boomers — and, again, she’s a proud, card-carrying member of that generation — in often-negative tones.

Mary Flahive-Dixon says most Baby Boomers want to age in place, in their own homes.
“This notion of the silver tsunami makes the aging of the population sound like an impending natural disaster over which we have no control that’s going to sweep everything away,” she said. “It feels to me, and most geriatrics leaders, like we’re framing things wrong; we’re setting this up as ‘us versus them’ — us young healthy, productive people against those old people who are going to overrun the system. These people are … us. They’re our neighbors, our teachers, our relatives.”
That said, a lot of ‘us’ are getting on in years. Indeed, maybe half or more of all Boomers can now get a senior discount at the movies, the golf course, and the pharmacy. And large numbers of them are now over 70, which means many aspects of the healthcare system — from eye care to urology; orthopedics to hearing care — are certainly already seeing an impact, and it will only grow as more Boomers reach 70, 80, 90, and beyond.
Restating the matter (again, she doesn’t want to classify it as a problem), Brennan said the Baby Boom generation is indeed large (it’s estimated that, by 2035, 10% of the population will be 85 or older; it’s closer to 6% now), and its members are living longer than the generations that preceded them, again, because of better health and better healthcare.
“That’s not a disaster or a tsunami,” she said. “That’s one of the greatest success stories in modern history; people are able to live longer and enjoy their lives better.”
That’s true, but so is what her mother said so often: that no one gets out of life alive.
“Some period of decline is going to occur for virtually all of us — unless we die in our sleep from a funny heart rhythm or get hit by a truck crossing Main Street,” she told BusinessWest. “And the causes of death in recent years have shifted; if you look back 50 or 80 years, the causes of death were frequently things like trauma, infection, death in childbirth — things that take you rather quickly when you were reasonably functional prior to that. That is no longer true. And with the successes we’ve had, and with people living longer, they are increasingly likely to die of multiple progressing chronic diseases.”
What does all this mean? Increasingly, Brennan said, people will need more care from more people as they age and approach end of life — a team-based approach, if you will.
“We’re going to have to think about care a different way because it’s not all about the doctors and the nurses,” she explained. “People will need hands-on home care, they’ll need symptom management, they’ll need direct-care workers who are grossly underpaid and overworked, and who churn through the system, with tremendous turnover.
“We’re struggling to meet those needs now, and it’s perceived to be, and is, a major problem,” she went on. “And if we do not alter the way we are paying, recruiting, supporting, and respecting those people, it will be infinitely worse. We’re going to need to restructure things, pay people differently, and offer them different kinds of professional development and career ladders that will make those positions more attractive; otherwise, we have a self-perpetuating situation. It’s the classic axiom — the system produces exactly the kinds of results it was designed to produce. If we don’t change the system, you get what you’ve got.”
Another issue that will have to addressed regards the number of specialists that will be needed to care for this larger generation of older residents, said Brennan, referring to geriatrics doctors, general nurse practitioners, social workers, pharmacists, and more.

Dr. Susan Bankoski Chunyk says people still put off seeking treatment for hearing loss due to outdated perceptions about hearing aids.
“As the number of older folks is increasing, the number of experts is not increasing, not one iota,” she told BusinessWest. “And, in fact, in some fields, such as geriatric medicine, the number of certified geriatricians has actually probably declined somewhat because we’re not replacing people who are retiring with equal numbers of new grads.”
The Shape of Things to Come
Flahive-Dickson agreed, noting that among the Boomers now in or approaching retirement are large numbers of healthcare workers. Replacing them and making the kinds of systemic changes Brennan mentioned will be just some of the many challenges facing the healthcare system moving forward.
Several of the others involve the growing trend of people wanting to age in place — and especially in their own home.
And this brings her back to COVID and what has been learned during the pandemic.
“More care was moving toward the home, basically as a result of general anxiety about facility care — about being in hospital, about being in a skilled nursing facility,” she explained. “Because of this crisis, we’ve seen more people want to get their care in the home.”
And this is a trend she expects will continue into the future as more people from this huge generation confront questions about the care they need and how and where they want it provided.
But questions arise from this supposition — many of them, in fact, including whether there will be enough providers to care for all those people who will want to stay in their homes, and also whether the payers are willing and able to adjust to a changing landscape of need and pay for services they currently don’t cover.
Again, Flahive-Dickson said the pandemic has provided an intriguing lens for looking at the problem — and the future as well.
“If COVID has done anything for us, it has previewed what is to come,” she told BusinessWest. “The pandemic has shown us that this surge in home care is a glimpse of the future. And it has provided this glimpse not only to healthcare professionals and the general population, but also to regulatory bodies, such as Medicare and Medicare Advantage.
“They have had to relax a lot of rules,” she went on. “As the Medicare population is continuing to grow, Medicare benefits haven’t caught up to that, and this is a huge problem. There are fewer than a dozen states that even offer non-medical home-care services to be paid for by a plan, and that plan is a singular plan, and that’s Medicare Advantage. In Western Mass., no one has a Medicare Advantage plan that offers the benefits of non-medical support, so it’s either out of pocket, or you have to qualify for one of the few programs that cover this.”
As for home-care workers, she said a number of demographic trends (Boomers generally had smaller families than the generations that preceded them) and other issues point toward individuals needing someone outside the family to care for them — and real challenges when it comes to having a steady supply of workers to provide that care.
That’s another lesson from COVID, she said, referring to the law of supply and demand, which was certainly exacerbated by a pandemic during which many had apprehensions about working in others’ homes.
“Fewer and fewer family members are capable of being a caregiver, either because there are fewer families, period, or … because family members might be on a different coast,” she explained. “Just because you grew up in Springfield doesn’t mean you stay in Springfield.”
Aasheim agreed, noting that these demographic trends are just some of the challenges facing the Baby Boom generation. Another is their own lack of preparedness for what is to come — financially and otherwise.
He said that only one individual in 10 has long-term-care insurance, and this is a matter to be addressed — just not when someone is 75 or even 65; those products have to be bought much sooner. Meanwhile, not enough members of this generation (and it’s not exactly unique in this regard) have their ducks in a row when it comes to needed documents — and needed preparation for poor health that often comes on suddenly and without much warning.
“What I try to focus on with the Boomers are the things they can do now, before that eventuality,” he explained. “This includes having discussions with your family about what your preferences are in terms of long-term care, gathering the documents together, getting power of attorney and a healthcare proxy, all those things. That’s what I hammer away with them — get that stuff done now, while you’re still healthy and you have the energy and the mental capacity to deal with it, so your family doesn’t have to handle it in crisis mode a few years down the line.”
Unfortunately, he said, many don’t heed this advice.
“They all nod when I talk to them in these presentations, but are they going home and getting that stuff together? My thought would be, probably not,” he went on. “Because most of the calls I get are from people who are in crisis mode.”
Bankowski Chunyk is another who wishes that more Boomers would heed some advice. Or at least listen to family members telling them they can’t hear as well as they used to, and should do something about it.
She told BusinessWest that the hearing industry talked a lot about the Baby Boom generation years (make that decades) ago, and how its size and advancing age would comprise a great opportunity for audiologists, one they should be prepared to seize.
Bankowski Chunyk did prepare, but she said the wave hasn’t been nearly as big as all those experts predicted it would be, largely because of … well, human nature, as well as lingering perceptions about hearing aids and what they say about those who wear them.
She said data shows that, between 1989 and 2019, the average age of an individual being fitted for a hearing aid for the first time fell from 66 to 65.
“I’m not sure a lot of progress was made getting people to address their hearing,” she said with some sarcasm in her voice, adding that, while there are certainly more people of that age than there were several years ago, sheer volume is not creating the immense opportunity that was predicted back in the ’80s and ’90s.
Whether it will materialize eventually or not, she doesn’t know — but she does know the Boomers are perhaps more vain when it comes to hearing aids than the generations that preceded them, so her industry has some work to do to change those perceptions.
Bottom Line
Perceptions are not the only thing that will have to change if the Baby Boomers, and those in the healthcare system who will care for them, will adequately manage this sizable demographic shift.
Brennan is right when she warns about this challenge becoming an ‘us versus them’ scenario, but she’s also right (and her mother was right) when she said that no gets through life alive.
As this generation ages, it will present enormous challenges to a healthcare sector that in many ways seems unprepared for what’s coming. That’s evidenced by the number of comments that began with the words ‘if things don’t change’ — comments referring to everything from workforce to accommodations for low-income seniors.
Only time will tell if things will, indeed, change. What is known is that the Boomers, as they have at every other phase of their life, will alter the landscape as they reach 75 — and beyond. And in all kinds of ways.










































































 The girl sits in her classroom and turns up the volume wheel on her hearing aid loud enough to hear her teacher. Suddenly, the classmate sitting next to her drops his book. She tries to turn her hearing aid down, but it’s already too late. A loud ‘bang’ echoes through her head, then ringing, and more ringing.
The girl sits in her classroom and turns up the volume wheel on her hearing aid loud enough to hear her teacher. Suddenly, the classmate sitting next to her drops his book. She tries to turn her hearing aid down, but it’s already too late. A loud ‘bang’ echoes through her head, then ringing, and more ringing.





































 Group classes — whether spinning or dancing or core workouts — are all the rage in the fitness world, and it’s easy to see why. Working out in a group provides not only socialization and support, but accountability and motivation to maintain one’s progress. Often, area gym owners say, the biggest challenge is just taking that first step — and learning that fitness classes are, quite simply, a lot of fun.
Group classes — whether spinning or dancing or core workouts — are all the rage in the fitness world, and it’s easy to see why. Working out in a group provides not only socialization and support, but accountability and motivation to maintain one’s progress. Often, area gym owners say, the biggest challenge is just taking that first step — and learning that fitness classes are, quite simply, a lot of fun.





