Heat of the Moment
 The rising temperatures are a great reason to have fun outdoors. But those summer activities pose myriad dangers, from sunstroke to tick-borne illnesses to drowning. Fortunately, most of these risks can be reduced and even eliminated through proper planning and common sense.
The rising temperatures are a great reason to have fun outdoors. But those summer activities pose myriad dangers, from sunstroke to tick-borne illnesses to drowning. Fortunately, most of these risks can be reduced and even eliminated through proper planning and common sense.
It’s not exactly news that kids spend too much time indoors, sedentary, in thrall to their electronic devices. The warm weather of summer should be an antidote, providing plenty of opportunity for exercise and recreation that doesn’t involve a screen.
On the other hand, the outdoors poses other types of hazards.
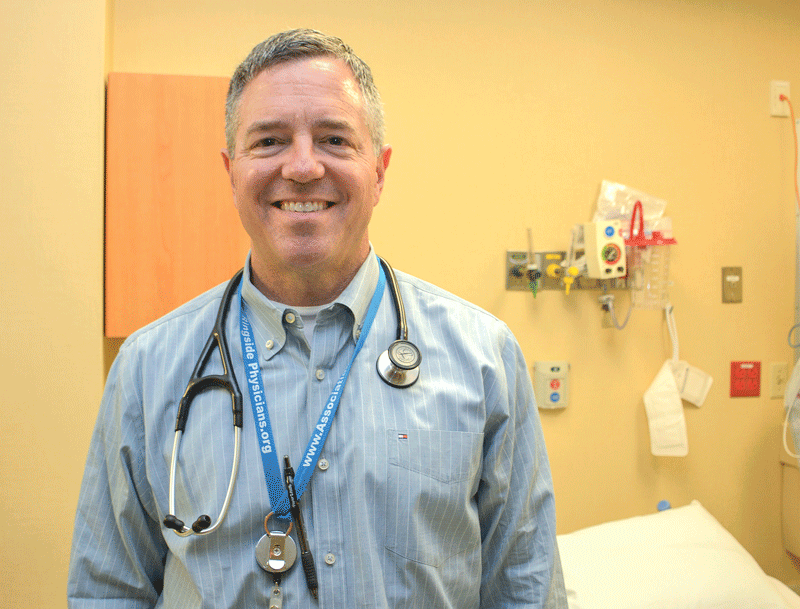
“Any time there are extremes in temperature, we start seeing things, and during the summer, there’s a big increase in minor stuff as well as some major stuff,” said Dr. Louis Durkin, director of the Emergency Department at Mercy Medical Center. “That’s the reality. So while it’s good to get the kids out of the house, where they’re not playing video games and watching TV, you take the danger with the benefits.”
Many issues, as he noted, are indeed relatively minor, from sunburns and poison ivy to overexertion injuries to weekend warriors who spent the cold months indoors and then overdo it with sports or home projects once the weather warms up.
However, Durkin continued, “on the bigger, more tragic side, we see an increase in drownings, people diving into the shallow end of pools and sustaining neck fractures, even violence. Usually, on the first hot days, when people get outdoors and have more exposure to each other, we see an increase in violence.”
The good news, he said, is that most summertime health and safety hazards, from heatstroke to trampoline injuries, are preventable. For this issue’s focus on summer safety, BusinessWest examines several common summer dangers — and strategies for reducing the risk of each.
It’s Getting Hot Out Here
Simply put, said Dr. Heba Wassif, “hot weather can be deadly.”
Wassif, who practices with the Heart & Vascular Program at Baystate Medical Center, noted that extreme heat — considered the number-one weather-related killer in the U.S. — affects people in different ways, and those at greatest risk include adults with existing heart and other chronic diseases, the elderly, and children.
“Sweating is the body’s defense mechanism to cool down, but at the same time, it results in the loss of more fluid than usual from your body,” she said. “This can cause your blood pressure to drop and your heart rate to increase to compensate for your fluid loss, so you may feel palpitations as your heart beats faster.”
Warning signs of an oncoming heat-related illness, she explained, could include excessive sweating, leg cramps, flushed skin, nausea and vomiting, dizziness, headache, and rapid pulse. Anyone experiencing such symptoms should get indoors or into shade and drink liquids, and, if they don’t better soon, should call a doctor or visit the ER.
In fact, Wassif went on, heat stroke can cause death or permanent disability, including damage to the brain and other vital organs, and requires immediate emergency medical treatment. Warning signs of heat stroke can vary, but may include body temperature of 103 degrees or higher, dizziness, throbbing headache, nausea, confusion, rapid pulse, and, in critical cases, unconsciousness.
Dr. Louis Durkin says emergency departments see an uptick of heat-, water-, and even violence-related incidents when summer arrives.
“The best advice I can give to anyone in the extreme heat, whether healthy or predisposed to any health conditions, especially cardiac disease, is to take it slow and easy and not exert yourself,” she said. “Try to stay out of the heat during the hottest part of the day, usually between 11 a.m. and 3 p.m., and stay hydrated by drinking plenty of water and sugar-free drinks while avoiding alcohol or caffeinated beverages.”
Dr. Joseph Schmidt, Baystate’s vice chair and chief of Emergency Medicine, noted that hot weather can affect certain medications as well.
“If you are taking certain medications, whether prescription or over the counter, sunlight may not be the best for you,” he said. “Certain drugs can impair your ability to deal with the heat and increase your sensitivity to sunlight, called drug-induced photosensitivity. As a result, your skin can burn at a much quicker rate than usual, even with a lower intensity of sunlight.”
Then there’s the issue of closed, overheated cars in the summer — a moment of carelessness that too-often kills children and pets, Durkin said. “Obviously, every year you hear about these tragedies, people forgetting about infants or pets in cars.”
Even many parents who would never leave their child alone in a hot car don’t have qualms about leaving their dogs there. But while humans cool themselves by relying on a system of sweat glands and evaporation, animals have a harder time staying cool, leaving them extremely vulnerable to heatstroke, according to the Animal Legal Defense Fund.
For example, on a day when it’s 70 degrees outside, the temperature inside a car with all the windows closed can approach 90 degrees in just 10 minutes, according to the American Veterinary Medical Assoc. On a particularly hot day, the temperature inside a closed car can shoot as high as 114 degrees in the same amount of time.
For that reason, it is legal in Massachusetts to break an animal out of a car, under certain circumstances. Specifically, after making reasonable efforts to locate the vehicle’s owner and notifying law enforcement or calling 911 before entering the vehicle, someone who believes entry into the vehicle is necessary to prevent imminent danger or harm to the animal, and plans to stay with the animal nearby afterward, may force their way into the vehicle to remove the animal, free from criminal or civil liability.

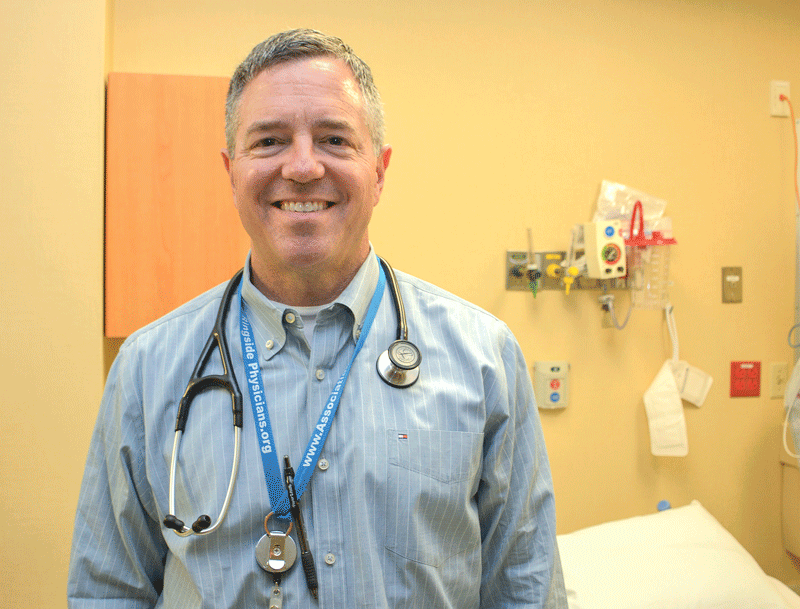
Dr. Michael Klatte
Children are especially at risk for acquiring RWIs since they usually play in the water for longer periods of time and swallow more water than adults typically do..”
Water, Water Everywhere
The other major summer killer after the heat itself is one of the ways people beat the heat: the water.
“Water safety is simple stuff,” Durkin said. “If you can’t swim, or if you’re out boating, wear a flotation device. Swim only in designated areas, and never swim alone. And if you have small children, put an alarm on the pool; those save lives.”
The American Red Cross lists several tips for enjoying the water safely, including:
• Swim in designated areas supervised by lifeguards, and always swim with a companion.
• Ensure that everyone in the family learns to swim well by enrolling in age-appropriate water-orientation and swimming courses.
• Never leave a young child unattended near water, and do not trust a child’s life to another child. Have young children or inexperienced swimmers wear U.S. Coast Guard-approved lifejackets around water, but do not rely on lifejackets alone.
• Set limits based on each person’s ability, do not let anyone play around drains and suction fittings, and do not allow swimmers to hyperventilate before swimming underwater or have breath-holding contests.
• Even if you do not plan on swimming, be cautious around natural bodies of water, including ocean shorelines, rivers, and lakes. Cold temperatures, currents, and underwater hazards can make a fall into these bodies of water dangerous.
• Install and use barriers around a home pool or hot tub. Safety covers and pool alarms should be added as additional layers of protection.
Drowning isn’t the only water hazard, however. Recreational water illnesses (RWIs) can pop up in both treated and untreated waters — from pools, hot tubs, and water parks to freshwater lakes, rivers, ponds, and even the ocean, said Dr. Michael Klatte, who works in Pediatric Infectious Diseases at Baystate Children’s Hospital.
RWIs are caused by germs and chemicals found in these waters, which can result in gastrointestinal, skin, and ear diseases, chemical irritations of the eyes and lungs, and, sometimes, neurologic and wound infections. The most commonly reported RWI is diarrhea, frequently caused by germs such as Cryptosporidium and E. coli. Otitis externa, commonly known as swimmer’s ear, is another common RWI. Those with weakened immune systems and pregnant women are at greater risk for more severe water-borne illnesses.
“Children are especially at risk for acquiring RWIs since they usually play in the water for longer periods of time and swallow more water than adults typically do,” Klatte said. He advises swimmers not to swallow water, to stay out of the water if they have diarrhea or an open wound, to shower before swimming, and to check diapers and change them in a bathroom or diaper-changing area — not waterside.
Clear Your Head
No matter what the activity, Durkin said, alcohol will invariably increase the risk of harm or death, so people need to monitor their intake. Alcohol impairs judgment and coordination, affects swimming and driving skills, and affects the body’s ability to regulate heat.
But having fun while sober is just one of many common-sense ways to enjoy the summer safely. Shriners Hospitals for Children recently got into the act with a program called Superheroes of Summer Safety, which offers tips to reduce the risk of injuries during the summer months.
“As a father and Shriner, I know that, within seconds, a fun-filled day can take a turn when an unexpected accident occurs,” said NASCAR driver David Ragan, the program’s spokesperson. “Shriners Hospitals and I want to provide families with simple ways to reduce the risk of childhood injuries so that kids can enjoy a safe summer.”
With the help of the National Assoc. of School Nurses, the national health system printed 125,000 safety materials to be distributed to kids and families. Advice includes playground tips like sliding feet first and swinging while sitting down; keeping children inside when lawnmowers are in use; keeping several feet away from firepits, campfires, or grills; and the usual warnings about sun protection and swimming with a lifejacket and a companion.
“At the very least, we can decrease the chances of bad things happening, if not outright prevent them. Most of this is common sense,” Durkin said. “Being active is good, but being active and smart is better.”
Joseph Bednar can be reached at [email protected]



 The rising temperatures are a great reason to have fun outdoors. But those summer activities pose myriad dangers, from sunstroke to tick-borne illnesses to drowning. Fortunately, most of these risks can be reduced and even eliminated through proper planning and common sense.
The rising temperatures are a great reason to have fun outdoors. But those summer activities pose myriad dangers, from sunstroke to tick-borne illnesses to drowning. Fortunately, most of these risks can be reduced and even eliminated through proper planning and common sense.