The Entering Class at Baystate Has a Decidedly Regional Feel
Dr. Margo Rockwell says she recently came across a journal she kept while winding her way through the eighth grade.She said she just happened to open the book to an entry that today seems loaded with prescience — and irony.
“I hurt my ankle playing soccer, and so I came to the hospital,” she said, paraphrasing what she put down on paper 17 years ago. “I talked about going up to the NICU [neonatal intensive-care unit, where her father, Gary, worked as a neonatologist], where my dad showed me around, and I saw all the babies. And I wrote, ‘maybe someday I’ll be able to work at the NICU — I think that would be fun.’”
Well, that day is here. Sort of.
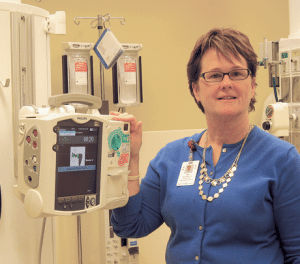
Rockwell is now a pediatric resident at Baystate Medical Center, and will undertake a rotation in the NICU sometime within the next year. She’s also one of an unusually large number of people who grew up in this region who are part of the new class of residents at Baystate and started work just about a month ago.
Indeed, Rockwell said she found her journal after “moving back home,” a phrase that many at Baystate are using this summer. In some cases, it means back to the house they grew up in, while for others it simply means Western Mass.
BusinessWest talked recently with four of these local residents — a phrase that certainly has a double meaning — three of whom are in the same field, pediatrics, or ‘peds,’ as it’s called. Their stories vary in some respects, but the common denominator is that on March 15, ‘Match Day’ for thousands of medical students across the country, they were thrilled to get the news that they would be coming back to this region.

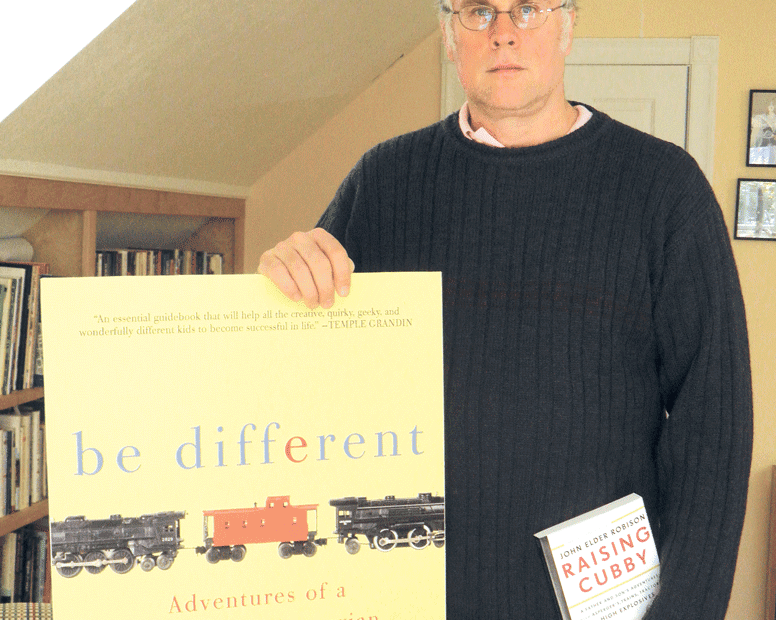
Dr. Adam Kasper, who recently moved back into his childhood bedroom, says Baystate was his first preference when ranking hospitals for his residency.
As Kasper opened his, he was confident he’d be staying in this time zone — eight of the 12 teaching hospitals he interviewed with are in the Northeast — but was pleasantly surprised to read simply ‘Baystate Medical Center.’
“I’ve got my old bedroom back,” he said, describing his parents’ home as an intermediate-term living plan. “I plan on moving out in the fall, but it’s very nice to be at home; it made the transition from medical school to residency so much less stressful.”
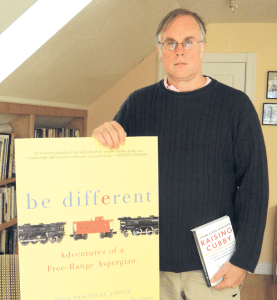
Dr. Elizabeth Langmore-Avila won’t be moving back to her childhood home, but she will be returning to the area where she grew up — she was born in Blandford — and has already worked professionally in the behavioral-health field.

Dr. Elizabeth Langmore-Avila says she finds work in behavioral health, and especially with those battling substance abuse, to be professionally rewarding.
Revisiting Match Day, she said she had interviewed at hospitals on both coasts, but Western Mass. was her preferred landing spot.
“I realized that it has a lot to offer in terms of what I’m looking for,” she said, listing both professional opportunities and quality of life. “And I decided I wanted to come back.”
That goal became reality when she woke up after a long night’s work in an emergency room to see a message on her phone left by someone with the prefix 413. It was the director of Baystate’s Psychiatry program offering her a welcome.
For this issue, BusinessWest revisits four such message deliveries and what they meant to those who received them, but also looks ahead with those individuals at where their current experiences in the place they call home might take them.
Meeting Their Match
As Dr. Laura Koenigs, director of the Pediatric Residency Program at Baystate, talked about Match Day, she referenced what she called the “computer in the sky.”
Others we spoke with used similar language, calling it simply “a computer” or “the computer,” or “a very complicated logarithm.” What it is, where it is, and what it’s called, no one seemed to know.
What they did know is that the software program in this computer would somehow determine their fate — for the next four years and possibly for the duration of their careers in medicine.
It’s called Match Day, because that’s when thousands of matches are announced, said Koenigs, adding that both medical students and teaching hospitals that interview them send their preferences for various specialties to that aforementioned computer, which ultimately analyzes a host of factors and determines where each medical-school graduate will go next.
“You rank programs, and the programs rank you, and you get matches — that’s what the computer does,” said Langmore-Avila, adding that med school students first learn if they’ve been matched (and more than 80% are), then must wait five agonizing days to find out which hospital they’ve been matched with.
Teaching hospitals like Baystate will weigh everything from academic performance to Springfield’s climate — “the cold and the dark can really impact some people,” said Koenigs, referring to the region’s long winters — when they submit their preferences. Meanwhile, medical-school students, some of whom will apply to a few dozen hospitals, will have their own criteria and priorities.
This year, the pediatric program took on 12 new residents, with half of them calling Massachusetts home, and four from the Pioneer Valley.
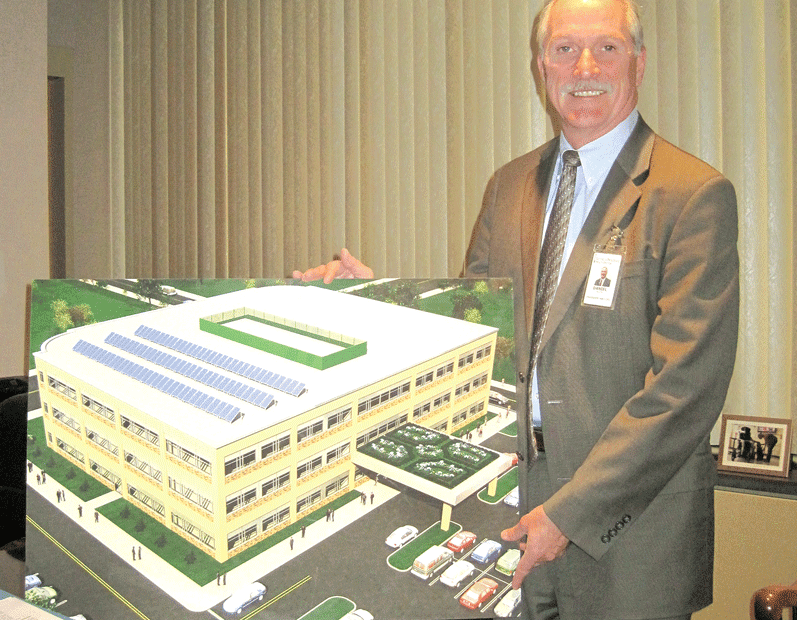
Dr. Shannon Rindone is among them.

Dr. Shannon Rindone says she gravitated toward pediatrics because she finds the work challenging and rewarding.
“I’ve always been surrounded by it,” she said, referring to the world of medicine. “My mother always said I could be whatever I wanted, and when she would bring me to work, I just loved it — I enjoyed talking to the doctors, the nurses, and the patients, and then I wound up working at Mercy myself as a patient-care technician.”
She said she was first drawn to pediatrics, or what she called “the little people,” while working at Cambridge University Hospital in England as a midwife care assistant. (She went overseas to be with her then-fiance as he worked toward his MBA at Cambridge.) She would go on to attend medical school at Nova Southeastern in Fort Lauderdale, Fla., and is now a DO, or doctor of osteopathic medicine.
On Match Day, she remembers being nervous and also somewhat jealous when a friend attending another medical school received her news a full half-hour before she did. When the e-mail finally arrived, she saw several words, including her name, but the only one she read, or cared about at that moment, was ‘Baystate.’
“The real preference was to come back home, and this is home,” she said, noting that she interviewed at many institutions, including a few in Florida.
She doesn’t, and couldn’t, know what tackling the rigors of a residency 1,000 miles from home, family, and friends would be like, but she acknowleged that having a support system close by (her mother and Mercy Medical Center are a half-mile away) is comforting.
“But at the same time, after a 16-hour day, sometimes you just want to put your head on a pillow, and your sister may want you to come over for dinner,” she noted. “And that can sometimes be difficult, because it’s hard for everyone to understand that you’re exhausted; you’re home, and they want to see you.”
She told BusinessWest that her career could take one of a number of paths, but she has developed a passion for pediatrics, and has shifted her focus there from her original pursuit, the ob/gyn field.
“I realized that the reason I liked obstetrics and gynecology was because of the family interaction and the baby, the product, at the end,” she explained. “And I really fell in love with just dealing with kids of all ages.”
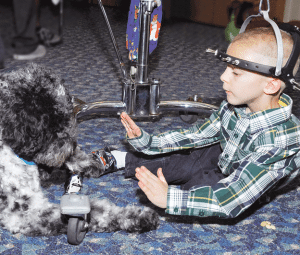
Currently on the rotation known simply as ‘the wards,’ or the ‘floors,’ Rindone said this involves seeing and treating patients in the Children’s Hospital, and represents a steep learning curve.
On the wards, she encounters children suffering from everything from meningitis to seizure disorders to fever. “It’s hard to see them when they’re like that, but it’s wonderful to know you’re helping them and easing the parents’ anxiety.
“Working with kids makes me smile every day,” she went on, “and you can’t complain about a job that makes you smile.”
Close Calls
Kasper can relate.
He said he was drawn to pediatrics while moving through the core clerkships during his third year of medical school at Temple. These also included internal medicine, surgery, family medicine, ob/gyn, and others, with pediatrics somewhere in the middle.
“I just found that I was more interested in the material,” he said of his chosen specialty. “I actually didn’t mind going home and reading about the topics as much as I did some of the other rotations. I just found that I enjoyed going to the hospital a little more each day — I knew this was where I was supposed to be.”
Elaborating, he said he liked the “patient population,” found his personality is better suited for that field than others, and, overall, considered it both more challenging and more rewarding than other areas of practice.
“The potential impact that you have,” he explained, “is much greater than when you’re treating a 70-year-old who’s been smoking for the past 50 years and has no intention of changing anything he does no matter what you say.”
Currently on the genetics rotation, Kasper said behavioral development is next, and as he looks ahead, he’s eyeing each of the segments with equal amounts of anxious anticipation and “dread about how well I’ll perform in them, because I’m still getting my feet under me and getting used to working at this hospital.
“They’re equally exciting to me right now because I’m entering residency the same way I while I was in medical school,” he continued. “I don’t know exactly where I want to go in pediatrics, so each thing is a possibility.”
Rockwell said she’s in a similar state, one where the options are many and most have yet to be explored in depth.
She segued into medicine while majoring in geology and comparative literature at Hamilton College in New York. “You could write about rocks, I guess,” she said with a laugh when asked what one could do with those degrees, adding quickly that she always had medicine in the back of her mind, did pre-med work at Hamilton, and was an EMT on campus.
She enrolled at the University of New England Medical School in Maine, where, like Kasper, she zeroed in on pediatrics rather late in the game — it was her last rotation, and she found she enjoyed working with children and families.
On Match Day, she was in surgery at a hospital in New York City when the clock struck noon and the results are posted. “The surgeon let me scrub out,” she recalled. “I opened my phone, and it was there in an e-mail: ‘Margo Rockwell; Baystate Medical Center; Pediatrics.’
“You were waiting all year for that e-mail, so it was pretty exciting,” Rockwell went on, adding that pediatric endocrinology was her first rotation, and that two months in the NICU, November and May, lie ahead.
She said she might get to work with her father, although they will likely be on different teams. And in the meantime, he’s been a great resource. “I certainly ask him a lot of questions.”
Meanwhile, Langmore-Avila is working with much older patients in Baystate’s Adult Psychiatric Treatment Unit, the adult inpatient facility at the hospital, one of many rotations she’ll experience this year.
Many of those she sees each day as part of a team of professionals have substance-abuse issues, she said, adding that it was work in this realm several years ago at the Riverbend Medical Group that inspired her to go to medical school and pursue work in that field.
“We admit patients, evaluate them, treat them as necessary, and monitor their progress,” she explained, adding that such individuals are then released either into the community or to a treatment facility.
This is work she finds rewarding on a number of levels, especially when she and other members of a team can change the course of someone’s life.
“I did a lot of substance-abuse treatment before medical school, and found it’s a field that I really like,” she said of her chosen path in healthcare. “It’s very much on the front lines, and it’s an opportunity to help someone who may have hit rock bottom. That’s a tragic state of being for a person, and if I can be there in the moment and try to help someone come out of that, get through that … that’s very important to me; it’s very meaningful.”
Local Flavor
As she walked with BusinessWest to the NICU for a few photos, Rockwell pointed to a small courtyard area where staffers can enjoy a meal or a quiet moment.
“That’s where I used to bring pizza for my dad,” she said, adding that she would often deliver him snacks when he was on call for stints that could last 24 hours or more.
Soon, the two might be sharing lunch or dinner there again, only this time they’ll both be wearing white coats and badges identifying them as doctors.
That journal entry logged all those years ago hasn’t officially come to fruition yet, but the younger Rockwell is a giant step closer to making it all reality.
For now, though, she’s another of Baystate’s local residents, and one of many happy to be back home.
George O’Brien can be reached at [email protected]