A chart of health and dental plans serving Western Mass.
Click HERE to download the PDF chart
Click HERE to download the PDF chart
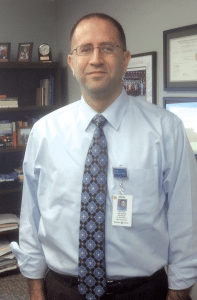
Dr. Jack Fanton says the increasing time kids are spending in front of screens may be coming at the expense of real-world social skills.
“In our clinical practice, we definitely see an overrepresentation of children who have difficulty with handling limits on screen time, especially when parents aren’t enforcing them,” said Dr. Jack Fanton, medical director of the Child Partial Hospital Program at Baystate Medical Center.
“We see children who have too much screen time, or devices are being brought into their rooms and are at the bedside and interfere with sleep continuity,” he added. “And lots of anecdotal evidence and research suggests this increased screen time is coming at the expense of real-world social skills.”
He cited a study at UCLA, published recently in the journal Computers in Human Behavior, suggesting that sixth-graders who went five days without exposure to technology were significantly better at reading human emotions than kids who had regular access to phones, televisions, and computers.
The researchers studied two groups of California sixth-graders, sending one group to an outdoor education camp, where they had no access to electronic devices, and making no changes to the media diet of the other group.
At the beginning and end of the study period, both groups were shown images of 50 faces and asked to identify the feelings being modeled. The researchers found that the students who went to camp were significantly better at reading facial emotions and non-verbal cues than the students who had access to their devices.
“Even after just five days, there was a measurable decline in their ability to recognize the emotions expressed on the faces, compared to a group of kids without any screen time,” Fanton said.
The study’s senior author conceded that the camp experience itself, fostering personal connections with other people, probably boosted that group’s scores as much as ditching technology, and she would like to expand the study to retest the camp group again, after they went home and spent five days with their smartphones and tablets. But the implication is clear that there is a measurable difference between human interaction and screen time.
And that worries pediatric experts who worry that a generation of kids may be growing up lacking sufficient empathy or emotional maturity.
“We’re acutely aware of how important it is to promote healthy social skills, and that emotional intelligence predicts more favorable outcomes than academic or intellectual intelligence,” Fanton told BusinessWest. “With cultural trends toward decreasing recess, music, and art, and then increasing screen time, neuroscientists worry that children are not exercising the circuits in the brain that are involved in emotional regulation. When kids are not involved in independent play and creative activities, when they’re not responding to social nuances, cues, and direct feedback, they’re not exercising the circuits involved in helping them nurture emotion and self-esteem.”
Healthy Choices
The American Academy of Pediatrics (AAP) has long advocated that young people up to age 18 restrict their screen time — including TV viewing, Internet use, video games, tablets, and smartphones — to no more than two hours per day, and that children 2 and under have no screen time at all.
“It’s not that media itself is bad, evil, or a pox on society,” Fanton said. “It’s that it’s coming at the expense of social needs and developmental processes critical to later success.”
The AAP cites studies that connect excessive media use with obesity, lack of sleep, school problems, aggression, and other behavioral issues, although Fanton stressed that any one of these correlations does not prove causation. Still, pediatricians fret over statistics showing that the average 8- to 10-year-old spends nearly eight hours a day with different media, and older children and teens spend more than 11 hours per day — much more than the recommended two hours.
Meanwhile, children and teens who have a TV in their bedroom spend even more time with media, and about 75% of 12- to 17-year-olds own cell phones, with nearly all teenagers adept in text messaging. The key, according to the AAP, is not banning all this activity, but directing it into a considered strategy.
“A healthy approach to children’s media use should both minimize potential health risks and foster appropriate and positive media use. In other words, it should promote a healthy ‘media diet,’” said Dr. Marjorie Hogan, co-author of the AAP policy (see sidebar, page 39). “Parents, educators, and pediatricians should participate in media education, which means teaching children and adolescents how to make good choices in their media consumption.”
Dr. Robert Leavitt, a Longmeadow pediatrician, tells parents that it is not a good idea to put a TV in a child’s bedroom, and advises them to set limits on cell-phone use before they give the child their own device. If they don’t do this initially, he explained, it may become difficult to enforce rules later on, and their teen may become sleep-deprived as they respond to non-stop text messages from peers.
Some parents will no doubt argue that familiarizing their kids with the latest technology is only preparing them for the world they will inhabit as adults, but Fanton said this philosophy ignores more critical needs.
“I would remind parents that kids are not little adults. Kids are still developing, and it’s not automatic they will develop these social skills as adults; they acquire these skills through innumerable hours and exchanges with other people.”
And there are societal consequences to raising a generation of young people who lack the ability to empathize and relate emotionally to their peers — skills that come in handy when dealing with bullying, for example.
“No one’s saying that not spending time with devices will help kids treat each other better,” he told BusinessWest, “but we want to promote a culture of tolerance and respect, where kids spend time with each other, and screen time interferes with that.”
Media and Message
The amount of time spent with screens is one issue, but content is another. Positive media can educate children — not just with hard facts, but in empathy, racial tolerance, and a wide range of interpersonal skills. However, it can also desensitize them to sexuality, violence, and negative attitudes.
Fanton cited a study conducted by the Joan Ganz Cooney Center, claiming that less than half the time kids between 2 and 10 spend in front of media is spent on educational programming. “It’s still being used for entertainment.”
Dr. Victor Strasburger, co-author of the AAP policy on screen time, noted that, “for nearly three decades, the AAP has expressed concerns about the amount of time that children and teenagers spend with media, and about some of the content they are viewing. The digital age has only made these issues more pressing.”
Dr. Laura Koenigs, a Springfield pediatrician who specializes in adolescent medicine, notes that violent programs, including cartoons, create their own host of issues. “Children who are exposed to violence experience long-term effects from watching it, even if it is not real,” she said, adding it can lead to aggressive play.
Still, Fanton said, some parents willingly accept a heavy dose of media exposure to the negative influences just outside their door.
For children in urban neighborhoods, for example, “the parents figure, ‘they’re not out on the street, getting themselves into trouble, so what’s the harm?’ Parents see these devices as safe. We have lots of families here in Springfield in these urban settings, and they don’t want their children in the neighborhood after school. Yes, it’s tricky.”
On the other hand, social media has been a boon to families who have moved away from their extended social supports, and their devices become proxies for face-to-face interaction. That’s why parents need to set their own limits, Fanton said.
“The truth is, we’re all addicted. It’s not going away. Kids are modeling at a fundamental level what they see us doing,” he said, noting that singling out an obese child and cutting off unhealthy snacks is likely to be counterproductive if the whole family isn’t modeling good nutrition.
“The same is true for screen time,” he said. “On one hand, there has never been more content, more ease of access through all these different platforms. But it’s up to adults to say, ‘we’re modeling this for the kids, too.’ They’re not little adults; they have different developmental needs that parents need to monitor and police and promote.”
In other words, put down that smartphone and engage with your child. It’s never too late to make emotional development a priority.
While media consumption can contribute to health risks, kids can still take positive lessons from media. The key is to teach children to make healthy choices.
To that end, the American Academy of Pediatrics recommends the following tips for creating a family plan for healthy media use.
• Take into account not only the quantity, but the quality and location of media use. Consider TVs, phones, tablets, and computers. The rules should be written down and agreed upon by all family members.
• Screens should be kept out of kids’ bedrooms. Insitute a ‘media curfew’ at mealtime and bedtime, putting all devices away or plugging them into a charging station for the night.
• Excessive media use has been associated with obesity, lack of sleep, school problems, aggression, and other behavior issues. Limit entertainment screen time to no more than two hours per day.
• For children under 2, substitute unstructured play and human interaction for screen time. The opportunity to think creatively, problem solve, and develop reasoning and motor skills is more valuable for the developing brain than passive media intake.
• Take an active role in your children’s media education by co-viewing programs with them and discussing values.
• Look for media choices that are educational or teach good values, such as empathy and racial tolerance. Choose programming that models good interpersonal skills for children to emulate.
• Be firm about not viewing content that is not age-appropriate in terms of sex, drugs, violence, and language. Movie and TV ratings exist for a reason, and online movie reviews can also help parents to stick to their rules.
• The Internet can be a wonderful place for learning, but it also is a place where kids can run into trouble. Keep the computer in a public part of your home, so you can check on what your kids are doing online and how much time they are spending there.
• Discuss with your children that every place they go on the Internet may be ‘remembered,’ and comments they make will stay there indefinitely. Impress upon them that they are leaving behind a ‘digital footprint.’ They should not take actions online that they would not want to be on the record for a very long time.
• Become familiar with popular social-media sites like Facebook, Twitter, and Instagram. You may consider having your own profile on the social-media sites your children use. By ‘friending’ your kids, you can monitor their online presence. Preteens should not have accounts on social-media sites.
• Talk to them about being good ‘digital citizens,’ and discuss the serious consequences of online bullying. If your child is the victim of cyberbullying, it is important to take action with the other parents and the school if appropriate. Attend to children’s and teens’ mental-health needs promptly if they are being bullied online, and consider separating them from social-media platforms where bullying occurs.
• Make sure kids of all ages know that it is not appropriate or smart to send or receive pictures of people without clothing or sexy text messages, no matter whether they are texting friends or strangers.
• If you’re unsure of the quality of the media diet in your household, consult with your children’s pediatrician on what your kids are viewing, how much time they are spending with media, and privacy and safety issues associated with social media and Internet use.
Joseph Bednar can be reached at [email protected]

Dr. John Schreiber says the collaboration between Baystate Children’s Hospital and Connecticut Children’s Hospital will create efficiencies and allow the hospitals to hire more specialists.
Elaborating, Schreiber, chief physician executive at Baystate Health, said this effort was sparked by numbers, specifically those involving the number of children on both sides of the border who need the services of a pediatric specialist, and the number of such specialists available to provide care.
Also, it’s about bringing the populations of the two areas — roughly 750,000 in Greater Springfield and about 1 million in Greater Hartford — together to create a patient pool that warrants the hiring of specialists in many areas.
“You could have specialists who live in between the two children’s hospitals who could serve both populations,” said Schreiber as he talked about how this collaboration could and probably will manifest itself. “And that would allow us to hire more specialists because the populations are bigger.”
Dr. Fernando Ferrer, chief physician executive at Connecticut Children’s Medical Center, agreed. He said the collaboration will allow both facilities to maximize asset utilization while greatly improving access to care by essentially bringing the physicians to the patients instead of forcing the patients’ families to travel to the physicians.
“There is a driving force right now in the healthcare marketplace to look for economies and efficiencies in the context of patient- and family-centered care,” he told BusinessWest. “The reality is that one of the guiding principles in family-centered care is that you make the care readily accessible and that you care for families and children close to home.
“It is better to have the subspecialists travel to the kids than have the families travel to the subspecialists,” he went on. “When you put the families and kids first, that’s really the best thing, as opposed to the normal territoriality where you have a program, I have a program, and they’ll compete.”
The collaborative effort will begin with a combined pediatric neurosurgery department — an initiative still in its early stages, said Ferrer — and likely expand to other areas, including ophthalmology (specifically eye care for premature infants), pediatric pulmonology, and pediatric urologic surgery, all areas where current provider shortages can make getting care difficult for patients and families.
Although this collaborative initiative is in some ways unique because it involves hospitals in different states and also involves children’s facilities, it is reflective of a movement within the healthcare industry to more effectively allocate resources to improve population health and continue a paradigm shift in the provision of healthcare from treating patients (in this case, children) when they’re sick to focusing on keeping them well, said those we spoke with.
“All across the healthcare environment right now, there are efforts to see what we can do together to become more efficient and serve the patient better,” said Schreiber. “Those discussions are everywhere, all across the country.”
And in many cases, cross-state collaborations like this one are more effective, potentially, because the institutions in question are usually not in a competitive situation.
“If you’re close together, as we are, you can create collaborations that serve both populations of patients with greater breadth and depth,” he said. “That’s really our intent with Connecticut Children’s, and that’s what is so exciting about our affiliation agreement with them.”
For this issue and its focus on pediatrics, BusinessWest takes an in-depth look at the collaboration between the two hospitals and how it is expected to improve access to care — and overall population health — on both sides of the state line.
No Boundaries on Potential
Schreiber told BusinessWest that discussions concerning the collaboration between the hospitals began several months ago, as officials at both institutions simultaneously realized the need for — and the potential benefits from — an affiliation agreement.
“There had always been good connections between Baystate and Connecticut Children’s because some of the faculty here trained there, and we also send people down there to train,” he noted. “We had been talking about trying to grow some of the specialty services for children in the area, and Connecticut Children’s seemed so logical because they were so close.”
Those discussions eventually focused on ways to meld the patient populations in Western Mass. and Northern Conn. into one, and then devise the most effective ways to provide care to that population, and bring benefits to patients, families, and pediatricians alike, said Ferrer.
“By working together, we can guarantee these people access close to home to some very sophisticated care in some specialties, including some where there are shortages nationwide,” he explained, noting that this is the first significant attempt at collaboration between the facilities. “That was the driving force behind this. There is a cultural similarity between the faculty of both facilities, so it makes looking at this as a team approach very appealing.”
When asked how this relationship would work and how those various constituencies would benefit, Ferrer and Schreiber started with changes and improvements likely to come about in the field of neurosurgery.
Pediatric neurosurgeons are in short supply, said Ferrer, adding that some regions of the country don’t have any. The problem is compounded when service populations are not large enough, and demand for services not steady enough, to fully support such specialists.
Through the collaborative initiative, the two hospitals are essentially providing specialists for a region (the Connecticut River Valley) rather than an individual institution.
“Rather than hiring two people for Baystate, when, quite frankly, the volume might not be there, or vice versa, hiring two people to be at Connecticut Children’s Medical Center for coverage purposes but not having the bodies there, we can do something that makes better sense,” he explained. “The more efficient use of the resources is to look at the region as a whole. You say, ‘these are the resources we need to take care of this whole population, and let’s have these individuals work collaboratively, so their overlapping skill sets can contribute, rather than having them work separately.’
“This would be a two-site model, because this is not about moving children from one area to another,” he went on. “With the two-site model, children in Massachusetts can get care in the Springfield area, and children in Northern Conn. can receive care in the Hartford area. The neurosurgeons would be the ones to move to those clinical locations and provide the care there.”
Such an operation, for lack of a better term, is something that will evolve over the next several months, said Schreiber, adding that there are a number of logistical matters to be worked out. And while that evolutionary process plays itself out, the two hospitals will look to extend that model to other areas, such as urology, pulmonology, and ophthalmology.
In the meantime, the facilities will explore ways in which the planned collaboration can be extended beyond clinical care delivery through possible expansion of a new pediatric accountable-care organization (ACO) being developed in Western Mass. by Baycare Health Partners, Baystate’s affiliated physician-hospital organization.
“We’re looking to create an ACO that would give the primary-care pediatricians in the region a better infrastructure to manage complicated children, to improve quality of care, and look at a population of children with an eye toward better prevention,” he explained. “We’re looking to work with Connecticut Children’s to create that model across the entire Connecticut River Valley, and we need to join forces to have enough pediatricians in the network to make it work.”
Another area of potential will be developing research collaboration between the hospitals in order to expedite discovery and treatment of pediatric conditions, said Schreiber, adding that, as needs arise, new avenues for working together will be explored.
Not Child’s Play
When asked if there is a model that this collaborative effort is based upon, both Schreiber and Ferrer said there are similar affiliations, most of them involving care for adults, but in many ways, this initiative is unique.
“I think we’re creating our own model,” said Schreiber. “There are lots of models with adult hospitals, but there are fewer children’s hospitals, and we’re honestly trying to create a new model, one aimed at serving the children better and also serving the primary-care pediatricians better.”
If they are successful in their efforts, the two hospitals will essentially erase the state line, create one service region, and bring new efficiencies at a time when changing conditions are making them a necessity.
George O’Brien can be reached at [email protected]
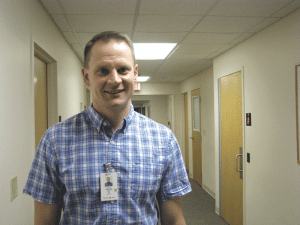
Dr. John O’Reilly says communicating with parents about their concerns is one of the most important parts of his job.
“Thirty years ago, pediatricians told mothers what to do; today, we give advice, but we also have true conversations. We are the experts in medicine, but parents are the experts on their child,” said Dr. Laura Koenigs, interim chair of the Department of Pediatrics at Baystate Children’s Hospital and a pediatrician who specializes in adolescent medicine. “It’s a change that has been good.”
Dr. John O’Reilly agrees. “Most of what happens to children takes place in the home,” said the general practitioner at Baystate Pediatric Associates and assistant professor at Tufts University. “The environment a child lives in has a profound impact on their health, and there are many areas to deal with in addition to medical care. Pediatrics is not just about giving shots. It’s only a small part of what we do.”
Indeed, the relationships that pediatricians form with families are critical to a child’s health, and Dr. Robert Leavitt says knowledge about a family’s history can help pinpoint concerns that may not be overtly expressed. For example, if a child has a persistent cough and the pediatrician knows their grandparent died of lung cancer that started with a cough, it allows them to alleviate fear that the parents may be harboring. “The more we know, the easier it is to help,” he said, adding that he opened Meadows Pediatrics, L.C. in Longmeadow in 1994 after working for Baystate Medical Center and a practice affiliated with the University of Rochester.
Many pediatricians see patients from birth through age 18, while others care for them until they graduate from college or are in their early 20s. “Young adults don’t always know where they will be living, and it can be difficult for them to find a primary-care doctor,” Koenigs explained.
But whether they are dealing with infants or young adults, education plays a critical role in their work as medical advances in areas such as brain development yield new information about topics ranging from the effects of screen time on children (see related story, page 38) to the ways in which poverty impacts health. In addition, doctors discuss developmental and behavioral issues that can be hard to deal with.
“Parenting is not a natural skill. It’s complex, difficult, and stressful, and different kids have different personalities that can be seen from day one. So we talk to parents about appropriate discipline, routines, and other things they are concerned about,” O’Reilly said. “Sometimes we can put a spin on problems that makes it easier for them to deal with. For example, when we explain that a tantrum is a way of showing independence, it helps parents get through the terrible twos.”
Leavitt says it’s also important to realize that children are not small adults.
“Things can be a big problem for them that would not bother adults. If an adult gets the respiratory syncitial virus, they will usually feel like they have a cold. But if a child under age 2 has the virus, they can develop bronchiolitis and may need to be hospitalized,” he said, explaining how it affects their tiny airways. “But kids are a lot of fun and are pretty healthy. They usually get better if they are sick, while adults tend to have more chronic problems and may have self-inflicted conditions.”
Koenigs concurs, and says children are a joy to work with. “I love what I do. It’s interesting, and it keeps me young. Kids have a wide-open outlook on life that makes you look at the world differently.”
Justifiable Concerns
One problem pediatricians face is educating parents who don’t want their child to be immunized against disease.
“Since we haven’t seen most of the diseases we vaccinate against for a very long time, people forget how horrible they are. They don’t remember tetanus and diphtheria or understand that a child can die from chicken pox or pertussis [whooping cough],” Koenigs said.
“Anyone who has seen these diseases would never want their child to get them, and with the exception of smallpox, they are all on the rise,” she went on, adding that a child with measles was treated at Baystate Medical Center last year, and a number of players in the National Hockey League were recently diagnosed with mumps.
Leavitt agrees. “These diseases are preventable, and parents who refuse the vaccinations are not making decisions based on scientific facts,” he said, citing the now-disgraced British doctor Andrew Wakefield, whose fraudulent study suggesting a link between vaccines and autism has contributed to plummeting vaccination rates.
O’Reilly agrees that immunizations are more important than ever as the world becomes more interconnected.

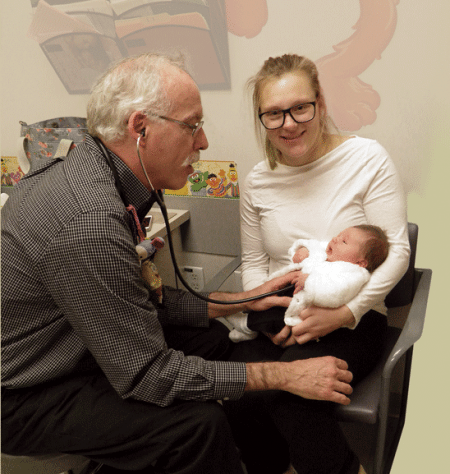
Dr. Robert Leavitt says pediatricians deal with issues ranging from irrational vaccine fears to childhood obesity to decisions about antibiotic use.
Koenigs said liberal state laws in Massachusetts also play a role in the problem. Although children are required to get certain immunizations before they can attend school, if parents sign a form saying they object to them, the requirement is waived.
Another pressing issue called ‘toxic stress’ can range from domestic violence to child abuse or a contentious divorce with ongoing conflict. The Center on the Developing Child at Harvard University says prolonged activation of stress-response systems in the body (especially the brain) have damaging effects on learning, behavior, and health across a person’s lifespan, but the effects often don’t show up until adulthood.
“We don’t understand why this happens, but studies show there is a direct correlation between toxic stress in childhood and high blood pressure, strokes, and obesity in adults. It’s also hard on the heart, even if children appear to have adjusted to the situation,” Koenigs said.
O’Reilly cited other, equally important research on the brain. “Some studies show that language develops rapidly during the first year of life, and the more words a child hears during that time period, the better they do in elementary school,” he told BusinessWest. “We do simple things in our practice such as giving every baby a book and explaining to parents that sitting with a child and reading not only helps with language development, but also helps them to focus, improves their fine motor skills as they turn the pages, and helps them with visual tracking and hearing. Many people think that education happens when children get to kindergarten, but parents can do things to build their child’s brains long before that.”
Environmental Factors
Diet is another issue that can certainly impact health, and Koenigs asks parents if they have enough food to last each month, because many don’t. “Nutrition is a problem for a lot of children who are not getting enough food or the right kind of food,” she said.
Play is also critical to development, and doctors are concerned that many children are falling short in this arena. “Children need to burn off energy, and kids are active in their natural state, which helps them to build muscle and focus better in school,” Koenigs said. “But many schools have gotten rid of recess.”
She added that exercise is also important for teens, and activities such as swimming, kayaking, hiking, bicycling, and kickboxing may interest them.
“If a child is very sedentary, it makes it difficult for them to become physically active when they get older. Exercise and eating habits are often established when children are young, and a lot of that depends on the parents,” Leavitt said, acknowledging that socioeconomic factors play into the equation, and some parents don’t live in neighborhoods where it is safe to let their children play outside.
Gun safety is another problem that affects children’s safety. “Seven to eight children in this country die every day from gunshot wounds,” Koenigs said. “You cannot educate children about guns. They need to be locked up because children are naturally curious.”
Overall, the relationship that parents form with their child’s pediatrician plays a critical role in whether they feel free to share concerns about their personal situations. For example, O’Reilly says many mothers suffer from postpartum depression, and it’s important for them to share how they are feeling because it can affect a baby’s development.
“If a baby is cooing and trying to get an adult to engage in an interaction and the parent is depressed, they may not notice or may have an abnormal response,” he said. “It’s also important for people to tell us if they don’t have enough food or money because things that happen in early childhood can lead to chronic disease in adulthood.”
He added that pediatricians can make referrals and help families access help, which ranges from family therapy to community support groups to early-intervention programs for children who are developmentally delayed.
Springfield suffers from a high rate of asthma, and housing in poverty-stricken neighborhoods can be related to the disease, as children can develop reactions to dust mites and become sensitized to antigens produced from exposure to cockroach droppings.
“Baystate has a program that sends home health workers to people’s apartments to help them improve the environment,” O’Reilly said. “Being a pediatrician involves far more than medicine. We have to do many other things. We are educators, but we are also coaches.”
Leavitt says partnerships mean shared responsibility, and doctors take parents’ requests seriously. “We used to routinely treat ear infections with antibiotics. If it’s a toss-up and the parent really wants the antibiotic, we can give it to them unless it is medically inappropriate,” he said, citing just one example. “But if you have developed a good relationship with the parents, they are more likely to agree to a let’s-wait-and-see approach.”
Moving Forward
Trust also comes into play when patients reach their teenage years. As children mature, pediatricians typically talk to them alone to provide them with the freedom they need to ask questions.
“It’s my job to help them navigate their way through adolescence and give them factual advice,” Koenigs said, explaining that, unless it becomes clear that someone is hurting them or they are in danger of hurting themselves or another person, these conversations are kept confidential. “Our job is not to drive a wedge between them and their parents. We are simply another link in their support system.”
Leavitt concurs, and says teens have told him they are depressed. “We see a lot of mental-health issues in teens. There is a lot of peer pressure in middle and high school, and as their social world becomes more complex, it can lead to anxiety or depression.”
Local pediatricians say they enjoy watching their patients mature. “We get excited about helping children get a good start in life and watching them grow through good times and bad,” Koenigs said.
Leavitt agreed. “We get to see how proud their parents are of their accomplishments. Plus, it’s rewarding to see medical problems get resolved or watch a child overcome challenges. It’s also rewarding to watch kids graduate from our practice and return to us with their own kids or go out into the world and do big things,” he said.
But the road to adulthood contains many roadblocks, and parents bring a variety of issues to the examining table.
“Being a doctor is like gardening; we plant seeds to weed out things that will be detrimental and help parents to make good choices,” O’Reilly said. “Sometimes being a pediatrician is pure medicine, and sometimes it’s purely behavioral. But our goal is help families so their children grow into healthy adults.”
Dan Moen understands that the closing of Hampden County Physician Associates (HCPA) is a big story in the region, but it’s just a part of a much larger story going forward.
“Physicians are concerned their reimbursement has been reduced by payers over a period of time, and their overhead, the cost of keeping up with all the administrative complexities, is also going up,” said Moen, president and CEO of the Sisters of Providence Health System (SPHS).
In short, he added, “I think physicians, to some degree, are feeling squeezed — not to say there aren’t some very successful physician groups out there, but in general, physicians are feeling they need to be part of a bigger entity, one that might have the resources to help them bridge that gap.”

The new building that houses several SPHS services, including physicians formerly affiliated with HCPA.
“We had a long, positive working relationship with Hampden County,” Moen said of the now-disbanded physician network. “When we heard from them that they were concerned about their future, we said, ‘this is too important to this community to let it just go away.’”
Thus, a month-long effort commenced to bring the doctors, plus two physician assistants and six nurse practitioners, into the SPHS-owned Mercy Medical Group, headquartered on the Mercy Medical Center campus in Springfield. Three business days after the bankruptcy proceedings forced all HCPA offices to close, the four practices that joined Mercy were back online in the same locations, in Springfield, East Longmeadow, Ludlow, and Feeding Hills.
“Everyone was professional through the whole situation,” Moen said, “and the end result is that the patients get to see their physicians, and none of that continuity was interrupted.”Similar negotiations ensued throughout October at Noble Hospital, which decided to take two HCPA practices into the Noble Medical Group. Two physicians who practiced in Westfield have moved to the Noble campus in the city, while five based in Southwick, along with a physician assistant and a nurse practitioner, will remain in their existing office.
“The decision was made for us,” said Noble President and CEO Ronald Bryant, speaking not literally, but in terms of the importance of physician access in his community. “Hampden County Physician Associates, by their dissolving, left a void in our market for primary-care physicians. Southwick and Westfield were already in our market, so not only was picking them up the right thing to do for our community and our patients, but it’s also the right thing for the physicians and staff, who will remain in the community for their patients.”
Other pieces on the board shifted as well. The Southampton Road office in Westfield, abandoned by the doctors who moved to Noble, was taken over by Mercy and will reopen in the spring, offering specialties including wound care, cardiology, hyperbaric therapy, and vascular medicine.
Meanwhile, allergists who had been part of Hampden County Physician Associates established their own practice, Allergy and Immunology Associates of New England, on the campus of Baystate Medical Center in Springfield. HCPA doctors who had practiced in nursing homes have also launched their own practice, Pioneer Continuing Care Providers. Finally, pediatrician and internal-medicine specialist Dr. Naomi Rosenberg has started her own practice.
Dr. Scott Wolf, senior vice president of Medical Affairs and chief medical officer at Mercy, said SPHS acquired the assets and equipment of the four practices as part of negotiations with HCPA. “Our primary goal from the outset was making sure nothing would change for patients, their relationships with their physicians would remain intact, and physicians would eventually welcome new patients into these practices.”
Bigger Pond
In its initial bankruptcy petition on Sept. 29, HCPA claimed it had lost doctors and was unable to recruit replacements. At the time, the physician group claimed $3.3 million in assets and $5.4 million in liabilities, while gross income across its network of practices had fallen from $39 million in 2013 to $25 million through the first nine months of 2014.
“There’s still a huge shortage of primary-care physicians in the area; we know that,” Moen told BusinessWest. “We’re seeing a lot of this happening these days across the country, where physicians are aligning themselves more closely with hospitals and health systems.”
The reasons have much to do with economies of scale and access to a fuller range of resources, he continued.
“Instead of working on their own, this gives them a bigger entity to work with. For example, we’ve got an IT team here at Sisters of Providence. That’s an automatic savings; they probably had to spend some dollars with an outside vendor and consultant, while we can do it inside.

Ronald Bryant said Westfield’s need for primary-care doctors practically made Noble Hospital’s decision to take seven former HCPA doctors into its network.
Wolf agreed that physicians will enhance their current practices by being part of a medical system. “They can coordinate care and leverage the infrastructure we have as a comprehensive health system, which will help us achieve the goal of overall population health, and will keep patients in their primary-care environment, where care should be delivered.”
He noted that a hospital with Mercy’s community demographics should average about 50,000 emergency-room visits per year, but the hospital actually averages about 80,000, partly due to a shortage of primary care. It’s also important for physicians to be more closely aligned with hospitals in this era of accountable care, a model that requires close coordination among hospitals, doctors, and other medical professionals.
“We’re moving away from fee-for-service,” Moen said. “People are starting to move toward risk-based contracts, flat-rate contacts, where the incentive is going to be for physicians and hospitals and other providers, like home care, to work even more closely together and be available to move patients along a continuum of care in the best possible fashion — to keep people well and out in the community. So it makes sense for physiciants to be more involved with hospitals in this care.”
Back to Work
Though most of the HCPA practices continued operations within a few days of the Oct. 31 shutdown, the group’s West Springfield office was shuttered, and doctors who worked there transferred to Mercy or the Feeding Hills practice. Meanwhile, the group’s urgent-care center in East Longmeadow was closed for the time being, its fate currently undecided.
Overall, though, Moen praised the transition that brought 19 new doctors into the Mercy Medical Group with minimal shutdown.
“We knew we’d keep this going,” he said. “It’s a great group of physicians and practitioners, and we never thought we wouldn’t make this move in some form or fashion.
“It’s just too disruptive for patients not to have their appointments,” he continued. “Simple thing like prescription renewals are so important. People booked these appointments months ago; it’s not like there are lots of openings in the schedule going forward. So we didn’t want more than a day or two of those schedules being interrupted. This is a talented group, in spite of the financial challenges, and we’re happy to have all of them get back to work doing what they love to do, which is taking care of patients.”
There were practical considerations for Mercy, too. “We knew we couldn’t afford to have this big gap in service for patients. We didn’t want them to look elsewhere for care. So this has been a success, from my point of view.”
Both SPHS and Noble stressed that patients would experience no insurance changes in the ownership transition. In fact, Wolf said, in some instances coverage will be expanded because of services provided under the Sisters of Providence umbrella.
Meanwhile, the system has been busy contacting some 60,000 patients to let them know how to find and contact their providers, and has set up a ‘coordinated care center’ telephone line to help patients navigate the changes. “This will be a transparent and seamless transition for patients as they maintain access to their physicians and other providers,” Moen said.
Wolf agreed. “All appointments are going off as scheduled, all practice sites up and running, our waiting rooms busy, and the physicians are busy seeing patients.”
Bryant reported an equally smooth transition of care, and said his biggest concern was making sure residents of Westfield, Southwick, and the environs were able to continue accessing the services they need.
“From our standpoint, the more important thing is that we’re here to provide care for the community,” he said. “These doctors were already located here in our market, so it’s a natural transition to join the hospital. There was minimal downtime and minimal glitches in the transition. They’re seeing a full schedule of patients.”
Eyes on the Future
Wolf noted that the 19 physicians who joined Mercy Medical Group already practiced at Mercy Medical Center, so their practices were never impacted that much. But their affiliation with the medical group helps Mercy build a foundation of primary care — a larger footprint, so to speak — and boosts its profile in recruiting efforts.
“This truly gives us an opportunity to recruit additional primary-care physicians in an area where they’re so desperately needed,” he said. “I think, with the reputation of the Sisters of Providence and Mercy Medical Center, it gives physicians comfort to be part of a bigger system and have access to the resources of that larger system.”
Moen agreed. “This gives us a base to recruit additional physicians. Having an established group, one that has a relationship with a strong hospital — that’s the kind of opportunity primary-care physicians are looking for, and we hope to be able to alleviate the primary-care shortage for the community.”
Doubling its primary-care pool from seven to 14 certainly won’t hurt Noble’s efforts, Bryant said, but “we did a pretty good job recruiting to begin with. What this allows us to do is enhance patient services. It makes it easier for them when they access our healthcare system; we’re able to provide a continuity of care, from primary care to specialist to the hospital, that might not have been present before. So I think it enhances the customer experience more than anything.”
In other words, the doctor is still in.
Joseph Bednar can be reached at [email protected]
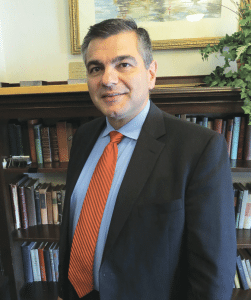
Spiros Hatiras says Holyoke Medical Center isn’t changing what it is and what it does — it’s just doing a better job of communicating it.
He goes on to note that he was a five-pack-a-day smoker and had long battled chronic obstructive pulmonary disease (COPD). His life changed, he implied, when a hospitalist at Holyoke Medical Center intervened.
“She just said, ‘you can fix this.’ You just felt like someone cared,” Morris said into the camera. “If it wasn’t for Holyoke Medical Center, I wouldn’t be going on tour with the Stones this fall.”
And with that 30-second message, now airing on several area television stations, Morris became part of an ambitious new marketing campaign launched by HMC this fall. This spot, like all the others, ends with another voice saying, “Holyoke Medical Center: experience the new standard in patient care.”
It’s not exactly a new standard, in the sense that the staff at HMC has always been caring and compassionate, said Spiros Hatiras, the system’s president and CEO. But it is new in the sense that many from this region, including some living in Holyoke and adjacent communities, are not familiar with the hospital.
This simple fact convinced Hatiras, who took the helm at the medical center 14 months ago, and others at HMC that they had to become more aggressive, and pointed, in their branding efforts.
“We’re not necessarily changing who we are — we’re just doing a better job of communicating it,” said Hatiras, who prefers the phrase ‘brand definition’ to ‘rebranding’ to describe what the system has undertaken. “The basic elements are still here — we are a solid, quality provider, and we’re a hospital of a size that is conducive to personalized care because it’s not very big and intimidating and confusing; we’re located in a great area, and we’re easily accessible. And at the same time, we’re big enough to have the services that most people would need.”
Elaborating, Hatiras said the basic goal of the campaign is to drive home the point that, in most cases, people in the Greater Holyoke area don’t have to drive past HMC on their way to Springfield, or anywhere else, to get the kind of quality care they want and need.
“There’s absolutely no reason, in my mind, why a resident of Holyoke, Chicopee, South Hadley, or Easthampton needs to go far away to another provider to receive the kind of care they can get here,” he explained. “Ultimately, what this campaign is aiming to do is let people know of the things we do and do well and what they can expect here, and keep people in the community.”
The marketing campaign includes a new logo (see page 29), television spots such as Morris’s, print ads (many of them in Spanish), billboards, banners within the hospital, and a revamped website. It’s all part of a multi-faceted initiative to raise HMC’s profile and increase volume, which also includes $2 million in upgrades to the Emergency Department and a new strategic plan.
 Overall, the system’s efforts are focused on putting out a new, stronger message, and then making sure it can back up those words ‘new standard in patient care,’ said Hatiras.
Overall, the system’s efforts are focused on putting out a new, stronger message, and then making sure it can back up those words ‘new standard in patient care,’ said Hatiras.
As for that logo, Hatiras told BusinessWest that it says different things to different people. To him, it speaks of both the region — through the use of the colors blue and green, representing water (Holyoke’s canals and the Connecticut River) and nearby mountains, respectively — and also a new beginning through its use of yellow.
“It’s a like a dawn, a new beginning, a bright day — that kind of feel,” he said. “That’s what we wanted to communicate.”
For this issue, BusinessWest takes an indepth look at this new beginning and the many forces that will shape it.
Ad Infinitum
“I’ve always looked at my patients, and cared for my patients, with the thought that that could be my mother, or that could be my grandmother, and I’ve always treated them as if they were mine, and I’ve treated them as I would want my family to be treated. I love being a nurse.”
That’s another of the 30-second spots airing on area television stations. It stars Lorimar Crus, a registered nurse who has been at HMC for three years. The sentiments she expresses reflect those of the system as a whole, said Hatiras, and sum up nicely both the message that is being sent through these various marketing vehicles, and the current focus of the system.
“While we’re not reinventing ourselves, I will say that we’re enhancing what we do and we’re focusing more on the experience that people have here,” he explained. “On the quality side, we do very well; we’re rated very highly. So what we’re really focusing on are those other qualities of the patient experience, or what people sometimes call the ‘softer skills’ — are we treating people with respect? Are we treating them with compassion? Are we treating people with empathy? Do we really care for people when they come in on a deeper human level?”
Hatiras said the work to revamp the system’s marketing efforts began almost immediately after he arrived last summer, because it was apparent that something needed to be done.
“We started talking about rebranding right away — at least started to think about how we needed to do significantly better in terms of communicating who we are, what we do, and what we do best,” he told BusinessWest, adding that these initiatives are being undertaken simultaneously with efforts to enhance (that’s a word Hatiras would use repeatedly) a culture of caring and compassion.
He said a market survey revealed that HMC’s primary problem wasn’t that people had a negative opinion of it, but that they didn’t have much of an opinion at all. Meanwhile, there was confusion, or ignorance, about the system.
“There were gaps in what people knew about us and about what we did; we still get confused with Holyoke Health Center, and frankly, there were people who didn’t know if we delivered babies here,” he went on, adding that the base of knowledge was broader in Holyoke, but much less so in surrounding communities such as Chicopee and South Hadley.
Hatiras believes HMC’s prior marketing efforts fell short for many reasons. For starters, there wasn’t enough of them, he said, adding that there was a also a lack of cohesion among messages sent by the medical center and its affiliates, River Valley Counseling Center, Holyoke VNA & Hospice Life Care, and Western Mass. Physician Associates, with each entity having its own logo, type style, and marketing strategy.
“No one could ever put it all together — no one really quite understood that the VNA was part of our system and River Valley was part of our system,” said Hatiras. “If your ads don’t all have a certain feel and look, they don’t resonate … if there’s nothing that ties it all together with the whole, it doesn’t make an impact.”
Part of the new branding initiative is broader outreach, especially to the Hispanic community, said Hatiras, adding that ads in Spanish are only a part of this effort.
For example, HMC was the lead sponsor of Holyoke’s annual Puerto Rican Parade in July. The hospital did not have much involvement with the event previously, he noted, and, ironically, Baystate Health was lead sponsor in recent years.
Care Package
But more aggressive marketing and greater outreach are only part of the equation, said Hatiras, returning to that phrase ‘softer skills’ and a recognized need to raise HMC’s game still higher.
“Even these have been core qualities of Holyoke Medical Center,” he said, referring to compassion, respect, and empathy. “What we’re doing now is putting a very significant internal focus on enhancing these qualities and making sure that we develop them further.”
The medical center is working with Pensacola, Fla.-based Studer Group, which, according to its website, “works to bring structure and focus to healthcare organizations through the creation of cultures in which people hold themselves accountable and help set them up to be able to execute quickly.”
HMC has ben working with the company for nearly a year now, and will continue to do so for at least three years, said Hatiras, adding that it takes time to make the kinds of fundamental changes the system is undertaking.
And there are several points of focus within this initiative, said Hatiras, listing everything from private rooms for all patients to revamped food service to valet parking for visitors. A common theme is to provide patients with a greater sense of control over their care.
“We started with some simple things, such as patient amenities,” he explained, “so that when people come here they feel safe, they feel they get treated the right way, and it’s a comfortable environment for them and their families.
“We’re converting all our rooms into private rooms so that there’s space for the family to visit and privacy, and we’ve revamped our food service so that people have choices in what they’re going to eat,” he went on. “When they get admitted, people have very little control over things, in general, and giving them the ability to have control is very important.”
Beyond these initiatives, HMC is also focusing on how the team administering care relates to patients and families.
“Studies have shown that, if physicians take the time to pull up a chair and sit next to the patient at eye level and communicate with them at that level, the interaction is much more meaningful, they get better information out of the patient, and the patient feels they’ll be listened to and understood a lot better than if someone stands at the foot of their bed,” he told BusinessWest. “By giving them that feeling of empathy, compassion, and respect, they heal better and faster.
“It’s just hard science — healing takes good medicine, and it takes good care,” he went on. “But it also takes that human touch, the compassion, the feeling of reducing the patient’s anxiety and making them feel safe.”
One priority for HMC is improving the environment in its Emergency Department, Hatiras noted, adding that the hospital was recently awarded $3.9 million by the Mass. Health Policy Commission to undertake renovations to the ER, and will launch a capital campaign to raise the balance of the projected $6-7 million project.
“The physical environment is very limiting and uninviting,” he said of the current emergency room. “It was built for 15,000, maybe 18,000 visits a year, and we’re doing 45,000.”
Brand Definition
Once the rebranding effort and other initiatives have gained traction, Hatiras said, HMC will conduct another market survey to see if attitudes, and overall awareness of the system and its services, have changed.
He suspects that they will change, and that verification will come in the numbers involving inpatient volume and, overall, the number of people driving elsewhere to receive care.
“The proof is in the pudding,” he said, adding that, while inpatient volume is down across the state, Holyoke’s rate of decline has been greater than in other areas. Reversing this outmigration, as he called it, will require a system-wide focus on not merely branding, but enhancing the patient experience.
And that’s what the system means by a ‘new standard in patient care.’
George O’Brien can be reached at [email protected]

Joyce Thielen says a significant shortage of nurses nationwide is on the horizon, with some specialties, like OR nursing, expected to be in particular demand.
At issue is the so-called nursing shortage, which made headlines 15 years ago but has receded somewhat since then, yet is expected to percolate again as Baby Boomer nurses finally move into retirement.
“I think, because of the age of our workforce right now, a shortage is going to happen,” said Joyce Thielen, associate dean of the Elms College School of Nursing, adding that many were ready to retire several years ago, but postponed that step when the economy went south in 2008.
“But as the market improves, as the economy improves, more people will start to retire. That’s the current thinking, anyway,” she noted. “There are specialties where that is particularly true. One example is the OR; many of the nurses in the operating rooms in area hospitals have been here for many years, and they’re predicting a shortage of them coming up.”
Nancy Craig-Williams, assistant dean of Nursing at Greenfield Community College, also sees plenty of opportunity, noting that all her school’s recent graduates who have passed the National Council Licensure Examination have received job offers in fairly short order.
However, “the opportunities may be changing from what people stereotypically think of as nursing,” she told BusinessWest. “Some students come in and expect to see the ER all the time, or they come into the nursing program and say, ‘I want to work in the hospital; can you guarantee me that?’ Well, no — we educate you to become a nurse and use the knowledge and skills you learn in school at a facility that needs those skills. Sometimes their ideas change once they’re in school.”
Some graduates, she said, don’t find themselves working immediately in their preferred environment, or working as many hours as they’d like, while about 20% of GCC’s nursing graduates move on from the two-year program and enroll in bachelor’s-degree programs elsewhere, reflecting a trend toward higher education for nurses in general.
“For them, this is a stepping stone as opposed to an end point,” Craig-Williams noted. “I think it has become more apparent to our associate-degree students that a bachelor’s degree will get them into positions, like acute care, that they want to go on to. Some of our graduates do go right to acute care, though, because they’ve been working at the facility or an opportunity presents itself.”
The Institute of Medicine (IOM), among other groups, has been calling for a better-educated nursing workforce, Thielen noted, especially at a time when a shortage of primary-care physicians is becoming more acute and nurses are being called upon to do more.
“Overall, we’re seeing a trend where associate-degree programs are highly encouraging their graduates to get their bachelor’s degree right away, and those with bachelor’s degrees are thinking about graduate schools,” she said, noting that fields like physical therapy, occupational therapy, and pharmacy are starting to require doctoral degrees for certain jobs, and nursing may not be far behind, especially at a time when the accountable-care model of care requires healthcare providers from various disciplines to work more collaboratively. “In order to be equal around the disciplinary table, nurses need to be better educated; it’s all about better patient outcomes.”
Still, she said, these trends shouldn’t scare prospective nurses from a field that’s sure to pose plenty of career opportunity over the next decade and beyond, at every education level. “It’s still a real phenomenon. It’s looking up. The last few years have been brigher, and opportunities continue to improve.”
Driving Demand
Healthcare economist Peter McMenamin told American Nurse Today recently that a combination of factors, from the aging of the nursing workforce to implementation of the Affordable Care Act, is driving rising demand for new nurses.
“Nursing is a good job,” he said. “Work satisfaction is high. If you look at the employment in U.S. hospitals for the last decade, month after month, there’s only a single month where employment went down. Hospitals have been continuing to hire during the recession.”
He cited U.S. Labor Department projections that 712,000 new jobs for registered nurses would be created between 2010 and 2020. “Everyone is expecting there are going to be more jobs. We’re hoping that there will be enough nurses to fill all of those jobs.”
The problem is that nursing schools are actually turning away applicants en masse, with capacity issues stemming partly from a long-standing lack of nursing professors.
From 2012 to 2013, for example, enrollment in bachelor’s-degree nursing programs increased by 2.6%, the slowest increase in five years. Meanwhile, nursing programs turned away 53,819 applicants in 2013.

Nancy Craig-Williams says the nursing profession provides a variety of opportunities and practice environments for graduates at every level of education.
“One of the trends is, we’re seeing hospitals offering residencies — they’re waiting for the right graduates to become licensed, and they’re offering residency programs that allows for a very intense orientation and helps with their entry into the practice,” Thielen explained. “And, again, we’re seeing a lot of graduates going to graduate programs earlier than ever. We’ve seen a lot of that because of IOM’s recommendation that nurses become a better-educated workforce. And the need for nurse practitioners is increasing because we have a decreasing number of primary-care providers. These are all trends.”
Craig-Williams agreed. “There’s a huge call for nurse practitioners right now. We do have students graduate from our program and transition to nurse-practitioner programs. In some cases, if they have other education or background, there are a lot of opportunities.”
Thielen also noted that a graduate’s chance of getting the job they want might depend on how willing they are to relocate.
“Our graduates are getting jobs, and they’re getting them right away if they go beyond New England,” she said. “We’ve had students go to North Carolina and other states — there are many more opportunities if you’re able to move out of the area. People staying in the area are taking a little more time; they may start out with part-time positions that grow into full-time positions or evolve into something else.”
According to the BLS, Texas, Florida, Washington, and Virginia ranked highest in job postings for nurses in the first quarter of 2014, while other states that showed significant growth over the last year include Georgia, Minnesota, and New Mexico.
“I believe that most of our national organizations, including the departments of Education and Labor, are saying we’re still looking at a nursing shortage,” Craig-Williams said. “Maybe it’s not as pronounced here in the Northeast, but it certainly is apparent in other areas of the country.”
Golden Years
Demographics — specifically, what’s commonly referred to as the aging of America — creates demand for nurses in two ways: by creating a wave of retiring older nurses, and by keeping people alive longer and needing more nursing care.
In fact, according to the American Medical Assoc. (AMA), adults 65 years and older represent the fastest-growing segment in American society, and this group is expected to surpass 40 million, or 13% of the nation’s population, in the next decade. America’s adult mortality rate, for men and women combined, ranks only 49th in the world.
At the same time, the AMA notes, chronic diseases account for 75% of American healthcare dollars spent, while more than half of Americans have some sort of chronic disease, like diabetes, heart disease, or cancer. Meanwhile, obesity has reached epidemic levels, with more than 72 million Americans, including 12.5 million American children, classified as obese.
The result is an American healthcare system approaching a state of dire need for many types of healthcare providers, nurses foremost among them — in all sorts of care settings, not just hospitals.
“Many of our students are getting positions in step-down, subacute units, long-term care, rehabilitation services. Some are working in the community, doing visiting-nurse or home-care placements. There are a few working in acute care,” Craig-Williams said, adding that a number of GCC graduates work at the Brattleboro Retreat, a behavioral-health facility just over the Vermont line, due to an ongoing relationship between the center and the nursing program. “Every year we do a rotation there.”
Overall, she told BusinessWest, nursing provides an abundance of opportunity for young people considering careers.
“We’re a small school, and we don’t graduate a large population of students, but our graduates are excellent candidates,” she said, adding that many are adult learners with bachelor’s or master’s degrees in other fields who considered nursing as a career later in life.
Whatever the case, she added, it’s becoming an increasingly good idea for many nurses to attain as much education as possible. “The research is pretty clear — a bachelor’s in nursing is going to increase your possibility of working where you want.”
Wherever that is, it’s important to remember that the greatest career benefit of nursing may be the ability to do something meaningful each day to help other people, Vicki Good, president of the American Assoc. of Critical Care Nurses, recently told nursezone.com.
“It may sound cliché, but we need to keep our eye on the ball, which is our patients and their families,” she said. “It’s so easy to become overwhelmed and distracted by the inevitability of change that we forget on whose behalf we do what we do.”
Joseph Bednar can be reached at [email protected]
 Dr. Doug Salvador says the push toward more efficiency in healthcare is working.
Dr. Doug Salvador says the push toward more efficiency in healthcare is working.
According to recent information from the Centers for Medicare & Medicaid Services (CMS), “healthcare spending trends have flattened, and some of the forecasts of spending from three, four, and five years ago have proven to be incorrect; we’re actually spending fewer dollars than we were,” said Salvador, vice president of Medical Affairs at Baystate Medical Center.
But the shift has been a challenging one, and no one expects it to get any easier.
For example, each year, the American College of Healthcare Executives (ACHE) surveys more than 1,000 hospital CEOs about their top concerns, including governmental mandates, patient safety and satisfaction, personnel shortages, care for the uninsured, physician-hospital relationships, implementing new technology, and other issues. For 10 years running, the broad category of ‘financial challenges’ has topped that list. In fact, it ranked far ahead of the number-two challenge — the tangentially related matter of healthcare-reform implementation — in the last three polls.
“It is not surprising that financial challenges and health-reform implementation are on the minds of hospital CEOs,” said Deborah Bowen, president and CEO of ACHE. “In addition, both government mandates and patient safety remain top priorities as CEOs and leadership teams work hard to improve patient care and redesign care delivery as they face a challenging reimbursement climate.”
Dr. Doug Salvador says healthcare reform is not simply about insurance — it’s also about controlling, and bringing down, the cost of delivering care.
“The ACA is designed to move us in that direction,” he told BusinessWest. “We are in a time of transition in healthcare, where to meet the goals of population health, we have to invest in taking care of patients outside the hospital. So we’re making some of these investments and, at the same time, have to preserve and improve the care we deliver in the traditional sense. That’s the transformation, and that’s what’s causing the results of these surveys.”
But keeping hospitals in the black while meeting patient needs and expanding services is not a new issue; hospitals have long lamented that their expenses constantly overshoot the reimbursements from public and private payers. But a decade-long shift to new, efficiency-based models of care seems to be having an impact on the industry that hospital leaders hope will make a positive difference in the long term.
Delivery Reform
Salvador noted that, when most people think about the ACA, they think of health insurance, which is only natural.
“There are two parts to ACA — one is insurance reform, and the other is healthcare-delivery reform. Insurance reform, insuring more of the uninsured, is what 95% of the press is about,” he explained. “But healthcare-delivery reform is really a set of experiments, of which Baystate was an early adapter.”
One is the move toward accountable care, which replaces the standard fee-for-service reimbursement model — under which hospitals are paid a fee for each procedure, plus additional fees for any complications that would require a readmission — with a system by which a group of different providers are paid a flat fee for keeping a patient healthy, which provides incentives to eliminate unnecessary costs, but also to make sure patients get the care they do need, because a major goal is to prevent rehospitalization.

Thomas Robert says Mercy Medical Center has implemented several protocols to achieve a balance between quality care and efficiency.
As outlined by the Institute for Healthcare Improvement, a Massachusetts-based organization that promotes innovation and safety in medicine, accountable care has three interlocking goals: improving the experience of care, improving the health of populations, and reducing per-capita costs of healthcare.
Those goals lay out in stark terms, Salvador said, why efficiency in healthcare doesn’t mean lower-quality care. “As care for individuals gets better, population health improves, and cost of care for the whole population decreases.”
The Sisters of Providence Health System (SPHS), which includes Mercy Medical Center, has been talking about accountable care for the better part of a decade and has realigned the way it structures care and payments.
“Through the ACO we have and other contracts we’re involved with, we feel that the future of healthcare is very much focused on population health,” said Thomas Robert, chief financial officer and senior vice president of Finance at SPHS. “Our readmission rates are among the lowest in the Commonwealth, and we are working to build a clinically integrated network with physicians in the community to be able to utilize these efficiencies for the benefit of the community.”
Mercy has implemented several protocols for achieving this balance between quality care and efficiency, from its high-tech Care Connect system — a sort of centralized air-traffic control for the whole hospital, ensuring that patients move through the system without delay — to an increased emphasis on arranging follow-up care, whether it’s home care, skilled nursing, rehab, or simply a primary-care visit.
“That has translated into a better patient experience but also reduced the length of stay, as we get them into a more proper setting, a more cost-effective setting,” Robert said. “And we follow up with the patient to make sure they follow up with these schedules. Again, that all leads to population health. So many times, patients get discharged without proper follow-up, and that’s where readmissions come from. We assist patients after they leave the hospital and make sure their care continues.”
The heart of accountable care, however, is how it’s paid for, and both Mercy and Baystate are participating in the model, backed by the Centers for Medicare & Medicaid Services, of bundled payments to multiple care providers for individual patients.
“We’re early adopters,” Salvador said. “For certain types of patient services we deliver, we agree with CMS to get paid for them on a 90-day bundle, which aligns the doctors, hospitals, and post-acute care providers. We’re all being interested in the same thing: making care the best and most efficient it can be.”
Big Plans
This new era of efficiency certainly doesn’t mean hospitals aren’t moving forward with expanded services and new technology; in fact, Western Mass. hospitals have been in a growth mode for some time. Baystate recently completed a $250 million expansion, Cooley Dickinson Hospital and Berkshire Medical Center are building cancer centers, and even smaller institutions like Noble Hospital have invested heavily over the past few years in equipment, services, and facility renovations (see related story, page 42).
“The financial pressures and challenges will not get easier,” Noble President and CEO Ronald Bryant told BusinessWest, “and it will continue to be a balancing act between costs we can support and our needs.”
Robert said SPHS has adopted a philosophy of “incremental investment” to make sure that Mercy and other elements of the health system grow as needed, but budgets remain under control.
“When we go through the capital planning process each year, we take all the wishes that are out there and really prioritize them according to quality and outcome for patients, patient experience, and increasing efficiency,” he explained. “We work closely with physician providers to help us prioritize those capital needs, and we target when we absolutely need to make the expense.”
A good example is Mercy’s recent conversion of its inpatient floors to private rooms. “We knew we couldn’t do the private rooms all at once; funds were not available for us all at once, and we’d also disrupt patient care,” Robert said. “So we started that process in 2011, in four phases, which we just completed. Now 80% of our rooms are private — a project that basically took three-plus years to complete.”
The system tries to be creative in other ways with its capital dollars, he noted, like its joint venture with Hampden County Physician Associates and Carew Chestnut Partners to build a $20 million outpatient medical office center at the corner of Carew and Chestnut streets in Springfield.
Because of the partnership, he said, “Mercy did not have to put up any capital dollars. We now have this very important access point on our campus without expending additional capital dollars. It’s really about trying to be creative.”
But efficiency also means tightening belts when it comes to care, Salvador said, and that’s something all hospitals have to deal with — as well as patients, who have become accustomed over the years to being offered any number of treatments and tests when admitted to the hospital.
“One of the interesting things for me is the link between the quality of care we deliver and how much the care costs,” Salvador said. “The challenge for hospitals with the ACA is to prove the value of all the care we deliver.”
From that challenge has sprung a national campaign called Choosing Wisely, led by the American Board of Internal Medicine Foundation with the support of close to 100 specialty medical organizations.
“They have identified a number of common practices that physicians have said we should question the value of — is the money worth the benefit of those practices? We’re seeing hospitals across the country — and Western Mass. is no different — really looking at some of those practices,” Salvador explained, and either justifying their widespread use or determining whether they may be of less patient-care value than they’re worth financially.
“One example is blood transfusions,” he continued. “They’re very common, and in fact they save lives, but evidence has come out recently to question whether using blood in some cases, particularly in certain patient groups, actually doesn’t save lives, doesn’t add value. So we’re seeing a national trend toward using less blood.”
In the same way, participating emergency physicians have questioned the use of high-end imaging for headaches, pathologists have questioned vitamin D testing, and so on.
“Cardiologists have a list, orthopedic surgeons have a list … it goes on and on,” Salvador said. “It also engages patients about their care, and I think that’s always been important. I think we’re getting better at it, and things like this help us do that.”
Beyond the Bottom Line
Salvador said he came to Baystate six months ago to grapple with these very questions, because transforming healthcare is part of the organization’s culture.
“From my perspective, a lot of hospitals across the country are discovering that the answer lies, more than ever before, in our continuing effort to improve the quality of care by delivering the best care with the fewest complications,” he said, emphasizing again the philosophy behind accountable care and the new national push to keep costs down. After all, he said, it’s not quality care that raises costs, but unnecessary care.
“Most of us are working very hard to reduce readmissions to the hospital and deliver excellent care both inside and outside the hospital,” he went on. “When we don’t have patients returning to the hospital, the overall cost goes down.”
It’s easier said than done, but hospital leaders say they’re making real progress toward this more efficient model of care. And that’s got more than just patients feeling better.
Joseph Bednar can be reached at [email protected]

Ronald Bryant says his primary accomplishment has been to create an environment where people want to succeed and are put in a position to do so.
Over the past three years, the president and chief operating officer has instituted impressive change that has brought new life to the independent medical facility and reinstated its standing as a top-notch center for healthcare in the Greater Westfield area.
Improvements include new physicians; a renovated patient wing; a new, comprehensive primary-care office building; a new, $450,000 Noble Walk-In Express Care service next door; a urology practice; new orthopedic offices; comprehensive breast-cancer services with a full-time breast surgeon; and a lot more, which have been realized through dedicated teamwork and outreach efforts, led by Bryant’s tireless effort.
“I have not done this alone. It has been accomplished with physicians, nurses, trustees, and administrative staff, which extends to dieticians who make sure patients have the right nutrition,” said Bryant. “My job is to create an environment where people want to succeed and are put in a position to be able to do so. And healthcare is moving so fast that you cannot stop. You have to get up every day and continually try to improve your organization.”
The hospital has 97 beds in a 257,000-square-foot building, which includes a telemetry unit, an intensive-care unit, a 20-bed psychiatric unit, a 15-bed inpatient rehabilitation unit, physician office space, and a medical/surgical unit which has been completely renovated with upgraded floors, walls, bathrooms, and nursing station, made possible due to money raised at the annual Noble Ball.
Noble’s new diagnostic imaging and X-ray service offers cutting-edge technology that helps physicians make definitive diagnoses.
“We were very prudent in making sure the investments we made promoted healthcare within the community,” he said. “Noble has always been consistent and conscientious about providing quality care, but in the past, we didn’t have enough physician services to keep patients in the community.”
That was caused in part by the critical shortage of primary-care physicians in Massachusetts as well as a national shortage, which made it difficult to attract these specialists to Noble.
But the hospital has been successful in recent recruitment efforts, and a primary-care office opened in July in a new building on 67 Union St. with seven primary-care doctors.
Noble’s efforts to attract physicians has also resulted in a partnership with the Urology Group of Western New England, P.C., which now has state-of-the-art exam rooms and office space within the hospital.
“This came about as part of our effort to build new relationships with physicians,” Bryant said. “They have their own waiting room and testing lab here now.”
There is also a new obstetrician-gynecological program, created through an affiliation with Baystate Medical Center. “Patients see their doctors here and deliver their babies at Baystate,” Bryant said, adding it is too costly for a hospital of Noble’s size to be able to do everything alone.
To that end, the third floor is now home to new cardiopulmonary offices and services, which also involves a liaison. “We partnered with the Baystate Regional Heart Attack Program and can get people out our door to their cardiology department faster than anyone else in the Valley and all of our competitors,” the CEO told BusinessWest.
Other improvements include a new, state-of-the-art, $2.6 million MRI center, which opened at the same time as the urology offices, along with a new van to transport patients. The service is free to senior citizens or anyone who needs it in the hospital’s primary service area.
“We’ve invested more than $6 million in the hospital over the last few years in equipment, services, and facility renovations,” Bryant said, adding that these investments have made a difference, and the hospital’s patient satisfaction scores for 2012-13, as measured by the Centers for Medicare and Medicaid Services, are the highest in Pioneer Valley.
“This is especially significant because not only are we the smallest independent hospital in the state, we are also the lowest-cost hospital in Massachusetts,” he said.
Strong Commitment
Noble’s CEO worked as a public accountant for a government agency before he entered the healthcare field, where he has put his talents to work for the past 15 years.
He was born and raised in Worcester, graduated from Assumption College, and is currently working on a master’s degree in health administration. He serves on the board of the Mass. Hospital Assoc. and Noble’s Visiting Nurse Assoc., and chairs the Greater Westfield Chamber of Commerce.
The licensed, certified public accountant began his healthcare career at MetroWest Medical Center in Framingham and Natick, where he served as account manager for the developmental disabilities and home health department. That stint led him to join Health Management Associates, a nonprofit organization that represents 70 community hospitals in the South and Southwest.
Time spent with that group inspired Bryant’s passion for community hospitals. “I went through their management program and realized early on that community hospitals were a good fit for my personality,” he said.
After working in South Carolina and Oklahoma, his family wanted to move closer to home, so when he was offered the position of chief financial officer at Martha’s Vineyard Hospital, he accepted.
Five years later, he moved to Goodall Hospital in Maine, where he held the same position, and three years later, he landed at Noble.
Bryant served for nine months as Noble’s CFO before moving to the position of president and CEO in August 2011.
“Noble Hospital offered challenges which were a good fit for my skill set,” he noted. “I had the financial background needed to compete in today’s healthcare environment and knew there was a good chance that the hospital had a bright future.”
However, he conceded that, in spite of this belief, Noble was in difficult financial straits when he arrived.
“I knew that, without proper fiscal management, physician recruitment, and rebuilding service lines, the future was in jeopardy,” he said. “The organization was in a good geographic location and had strong demographics, but had poor fiscal management.”
However, his past experience soon came into play. “Both Martha’s Vineyard and Goodall were financially challenged, but I was very fortunate to have mentors at both hospitals who taught me a great deal,” he said.
His first step was to rebuild the hospital’s four-person revenue team.
“I brought in new talent and reorganized and revamped a new, talented team of 20 people,” Bryant said, noting that the top two factors that lead to the success or downfall of any community hospital are its physicians and management of its revenue.
“So, after we solidified our financial position, we turned our attention to growth,” he explained.
This was critical because a community survey of the hospital’s service lines revealed a shortage of physicians in the area. “It also showed that more than half of the population was not aware of the services Noble provided, so our task was clear.”
The hospital took steps to recruit doctors to work there full-time, and cultivated relationships with others willing to become affiliated with Noble.
The effort was very successful.
“Twenty-four months ago, we had one physician on staff, and now we have seven, and to complement this, we also rebuilt specialist services,” Bryant noted, adding that the hospital re-established relationships that had existed in the past and formed new ones with specialists on the other side of the river.
That included its partnership with the urology group as well as the creation of a comprehensive breast-cancer program.
“We also hired a gastroenterologist to partner with the existing one on staff, and revamped our radiology, anesthesiology, and pathology services, which helped build confidence among the physicians in our community. If a hospital doesn’t offer strong services, physicians won’t send their patients there,” Bryant explained.
The demand for general surgeons was also met, and Noble now has two surgeons who also work for another hospital. “It fills two needs — ours and their need for more volume,” the CEO said. “And a good percentage of our doctors are also affiliated with Baystate Medical Center.”
For example, Noble’s breast-cancer surgeon brings in plastic surgeons from Baystate Medical Center to do reconstructive surgery on their patients. “Our doctors and affiliated physicians work together, and these types of relationships help make us successful,” Bryant said.
Once the hospital had attracted enough physicians, the next step was to create a comprehensive marketing program that was specifically designed to reintroduce Noble to the community. It began two and a half years ago with a “Yes Noble” website, on which Noble employees wrote about how much they enjoyed working there. “We just won an award for it,” Bryant said.
From there, efforts were aimed at informing residents in the hospital’s geographic area of the services Noble offered, as well as introducing doctors in the Noble Health Network. It was accomplished via speaking engagements, radio and TV advertising, publications, and a healthcare symposium in Westfield that attracted 100 people who learned about what Noble was doing in the area of healthcare reform.
“We speak at all major community events and are very, very visible in the community,” Bryant said.
In addition, the hospital hosts a series of ongoing employee luncheons where physicians talk about what they do.
“There will always be competition, but from the time I came here, I believed that, if we did our job in a high-quality fashion, patients would not want to cross the river,” Bryant said. “I told myself from the beginning that I wanted each individual in our community to think of Noble first for their healthcare needs. I want our healthcare network to be the best place to give and receive safe, quality, compassionate care.”
Ongoing Mission
The vision that Bryant brought to the position continues to broaden. “Everything we’ve done has been geared toward keeping patients here, and the confidence we’ve built has allowed us to maintain our market,” he said. “But I’m always thinking about what’s next. It’s really important to adapt to change and be able to capitalize when opportunities arise.”
To facilitate that goal, he has surrounded himself with people who are talented and have great imagination.
“The financial pressures and challenges will not get easier, and it will continue to be a balancing act between costs we can support and our needs. But I want to go further and continue to grow our market,” he said. “Our work hasn’t stopped, and we will continue to develop our network so we will become the provider of choice in our area.”
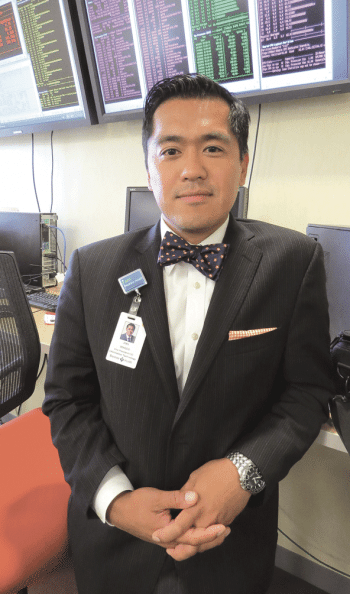
Joel Vengco says healthcare IT now involves much more than technology. Increasingly, the focus is on taking data and transforming it into information — and then knowledge.
And he started with some subtle humor.
“There’s a lot more meetings to go to,” he said with a laugh, choosing that starting point to explain how and especially why this administrative position is now much more about information and operational strategy than it is about hardware and software.
“CIOs today are more strategic in nature; today, there’s so much reliance on technology and on information inside those technologies that the CIO has to be part of the strategic discussion and the envisionment of business as a whole,” he told BusinessWest. “And that’s a different skill set altogether. You really have to understand strategic development, you have to understand the business that you’re in, and you have to understand finance.
“And you have to be more of a people person than I think CIOs were in the past,” he went on, adding quickly that he certainly wasn’t disparaging those who came before him, just referencing how times have changed. “Many of them would sort of hide out in the data center and focus on putting up a server. We’re now forced to be out there, talking to our partners and our users and really helping to lead the use of technology and information for competitive advantage or progression of the business.”
Elaborating, Vengco said the CIO must now wear a number of hats in addition to those that have been traditionally worn. Indeed, while the CIO is still tasked with keeping a health system running from a technology standpoint — what Vengco called “keeping the lights on,” a reference to everything from PCs to operating-room equipment — there is now much more to this job.
“In many ways, I wear an operating hat, a strategic hat, a finance hat, and sometimes I even wear a clinical hat, even though I’m not a clinician,” he said. “And then, you have to wear the innovation hat, because you can’t be stagnant and just look at the technology in front of you; you need to understand and begin to distill all the new technologies that are coming down the pike and correlate them with the current problems and the future state.”
With that mentality, Vengco was one of the key architects of the Baystate Innovation Center, what he described as a cross between an incubator and an accelerator that is taking shape at 1350 Main St. in downtown Springfield (more on that later).
But perhaps the most important line of the job description for today’s healthcare CIO, he said, may be enabling both a specific health system and the community it serves to make more and much better use of the vast amounts of data that modern technology allows people to collect.
Vengco, who came to Baystate in 2012 after work with GE Healthcare, has spent much of his career focusing on information and analytics, or what he called “liberating data,” and transforming it first into information and then knowledge.
“Data is the raw content of systems; it’s the diamond in the rough,” he explained. “You really have to transform it, or massage it, in layman’s terms, to really come up with information from that data. and then, from that information, you can develop knowledge through the delivery of an architecture that really takes that information and makes it actionable for people.
“If you put most of the raw data we have into a computer or an algorithm, it wouldn’t be able to compute anything out of it. In isolation, it may not necessarily make much sense; it’s just data, not information,” he went on. “But once you put it into context, like if you took a lab value and put it in the context of a disease state, or, better yet, you aggregated all of those labs and correlated it with a specific chronic disease state for a cohort of patients, then you have information about diabetes or information about congestive heart failure.”
For this issue, BusinessWest talked at length with Vengco about the evolving and expanding role of the CIO — and about all those hats he and others who take that title are now wearing.
Technically Speaking
Vengco told BusinessWest that, since childhood, he’s been drawn to the healthcare field, and that he attended medical school to essentially appease his parents and become a doctor. But his career path took an abrupt turn during his second year there.
“I was transitioning into my Ph.D. years, and one of my thesis advisors had suggested that I look at doing some work with a health information technology firm, which back then [2001] was pretty novel,” he explained, noting that the firm in question was Boston-based Eclipsys. “The idea was to develop a national data warehouse where I could develop algorithms for disease progression, outcome measurement, develop new clinical decision-support rules in analytics — a lot of the things we’re talking about now in terms of big data, but perhaps it could be done in this corporation.”
He took on that challenge, and in the course of doing so discovered that there was a considerable challenge behind utilizing the data collected by health systems because it was largely unusable, and not “liberated,” a term he would use early and often to describe this phenomenon.
In short order, finding ways to make such data more usable became his career passion.
He left medical school and entered the field of informatics and analytics. He interned at Partners Health Care and later taught at Harvard before landing at Boston Medical Center for his first IT operations job.
“It was at that time that I started to see the value of understanding technology in the context of a journey toward really understanding information,” he noted. “Because, ultimately, my real interest here was to try to figure out how to utilize this information so we could develop new knowledge and new insights. Technology changes so rapidly, but what is a mainstay and the most important element for me is information that we can gather from these systems. It’s like DNA for the human body; this information is the DNA for coordinating and developing quality care for the future.”
From Boston Medical Center, he went to GE Healthcare, where he became vice president of a global business called eHealth, a job he took to better understand what people in other countries were doing in the emerging field of population health.
He took part in projects in the U.K., France, Australia, Canada, and other countries — many of them involving health-information exchanges, care-management systems, collaboration systems, mobile health platforms, and population-health analytics — and took some valuable lessons back to the U.S.
Vengco said he wasn’t looking to leave GE, but always harbored a desire to return to the setting of the health system CIO, preferably in Boston, and in early 2012, Baystate was advertising for one.
“I hadn’t really thought about Springfield or Baystate — I knew of it, but didn’t really know the culture and the footprint of the community,” he said. “When I was recruited to take the interview, I came out here to see what it was about, not really looking to make an adjustment or a move. But I was really surprised with the vision Baystate had and the leadership it had.”
What’s more, he toured the region and came away with the impression that it would be an ideal setting for the innovation center that is now becoming reality.
“I enjoyed my discussions with Baystate, and was deeply moved by the mission they had for the community and healthcare in general,” he said. “It really matches my vision and my hopes — that healthcare needs to be more patient-centered.”
Making IT Happen
Vengco said the work of the IT Department at Baystate has four main pillars:
• Optimization, or making the most of the technology systems that exist today;
• Community engagement, or community collaboration, a realm that includes an initiative known as the Pioneer Valley Information Exchange (PVIX), which essentially creates a single patient record that optimizes the care delivery of all transitions of care across the continuum;
• Analytics, or the liberation of data; and
• An innovation platform, perhaps best represented by the innovation center.
Focusing on all four, plus that aforementioned work to keep the lights on, has become a considerable challenge, said Vengco, noting that he and his staff of roughly 230 are inspired by the breadth and depth of that challenge.
“You really are thinking well beyond the technology that you have to install,” he noted. “It’s an exciting time, but it’s also very daunting; I feel the enormity of the task, and so does my staff.”
And with that, he returned to his thoughts about how IT now extends into the realm of information — both gathering it and liberating it.
“The historic design of the EHRs (electronic health record systems) in the past and somewhat current state is that they take in data, but they don’t necessarily spit it out easily,” he explained. “And data loses its value if you don’t have the ability to liberate it and use it for the delivery of care. And that has been my mission since I started this journey back in 2001.
“There’s so much to be gleaned and to be achieved through the data we have locked in our systems,” he went on. “That’s why liberating that data is the first mission we should all have, because once we have that information in hand, it becomes knowledge and actionable delivery of care.”
Many of the Baystate IT Department’s initiatives have come together in the creation and operation of the PVIX, said Vengco, adding that the broad aim is to create a single patient record that can be used by a host of area care providers.
“Patients are very mobile; they’ll see a specialist, see a primary-care provider, visit the hospital … and those care organizations may not be affiliated with each other and so may not be on the same electronic medical record system,” he explained. “So when a patient goes in for his next visit and the provider wants to see all the meds they’re on and all the allergies they may have, they may not see all that comprehensive data because it may be in other systems dispersed across the community.
“So, today, we have to hope that a patient knows all the meds they take and all the allergies they have, or that the medical group down the street that they just visited will fax that information,” he went on. “But that doesn’t happen consistently, so you wind up treating patients with the information you have, and it might not be enough.”
The PVIX was created to solve that problem, he went on, by creating a comprehensive record that essentially follows the patient.
Founding members of the exchange include Baystate, Mercy Medical Center, Health New England, Riverbend Medical Group, Berkshire Health Systems, Holyoke Medical Center, and many others, said Vengco, adding that some of the challenges moving forward are convincing patients that their information is secure and also convincing providers that sharing such information is the right thing to do at this critical juncture for the healthcare industry.
“There’s still an uncertainty among organizations that care for patients about whether they should be sharing that data with other collaborating providers,” he explained. “And some of that stems from the notion that this data is competitively advantageous — that, if I share this data, you might know enough about me and my market to steal my patients.
“That’s just not where we need to be to care for our patients in the appropriate way,” he continued. “We have to be able to say, ‘for the betterment of patient care, quality of care, and efficient care delivery, we need to be able to exchange this information.’”
Center of Attention
Putting on that aforementioned innovation hat, Vengco stressed the importance of not simply understanding and maintaining the technology of today, but also anticipating the technology of tomorrow and being at the forefront of its development.
This was the impetus for the Baystate Innovation Center, which is still under construction but is in many ways already operating at One Financial Plaza in downtown Springfield.
“We need to make a mind road map, if you will, of what technology needs to look like in the future for your business,” he explained, noting that the innovation center was created, with the help of a $5.5 million state grant, to focus on solving the problems of healthcare today through technology and informatics.
The center’s creation — not to mention its location — brings another layer to a growing regional emphasis on entreprenurship, technology, and economic development, said Vengco, noting that, within a few blocks of each other, the innovation center, Valley Venture Mentors, and Tech Foundry, a facility dedicated to training individuals for careers in IT, are creating enormous momentum for new technology startups and getting established companies to the next stage.
“For those of us in healthcare, the rapid change that has come as a result of reform and the need to change healthcare delivery requires us to continue to innovate,” he said. “And for Baystate, this is an extension of our mission because it enables us to continue to look forward to doing the best that we possibly can to deliver the best possible care to the community through these innovations, while still maintaining our current operations.”
Elaborating, Vengco said innovation center administrators are looking for ventures that are in what he called the “last mile of development.”
“They come in with a solution already in hand, but it really needs a few more tweaks here and there, and that’s where we really come into play,” he noted. “We provide that innovator with the necessary adjustments and development advisement to get them to a usable product or solution.”
And these products and solutions are carefully chosen to meet the objectives of the health system, he noted, adding that organizers are not necessarily looking for the next Google.
“The intention here is to make sure we’re bringing in solutions that will address system objectives,” he told BusinessWest, adding that these include improving quality of care, patient progress, high-value care, and bending the cost curve. “We’re looking for technology that’s relevant to the problems we’re trying to solve. It’s not about making money; it’s about delivering an innovation that’s going to help us achieve our mission in an optimal way.”
He went on to say that he considers Baystate to be a model health system in a model state — Massachusetts is generally considered to be on or well ahead of the curve when it comes to innovations in healthcare — and that the Baystate system, by implementing products and concepts developed at the innovation center, could become an important proving ground moving forward.
“As you look at all of these other organizations, these integrated delivery systems that are being built or are already in place, they’re aspiring to be what I believe Baystate is already beginning to become,” he explained. “And we’re in a state that in many ways is one and a half to two years advanced in terms of policy and reform, and that becomes very attractive for developing solutions when you’re looking at ways to impact care delivery across the country. If you can do it here, it’s likely that it’s going to be impactful elsewhere; it’s a really great environment to do that kind of innovation.”
For the Record
Summing up his thoughts on health IT and where it’s headed, Vengco said it is going to play an increasingly vital role in the delivery of patient care and overall population health.
And carrying out the many and diverse aspects of his department’s mission will become ever more challenging as it extends well beyond technology and optimizing all that it brings to the table.
“My responsibility is to try to engage our leadership and our strategy so we can focus the use of technology and information,” he explained. “That’s the challenge; everyone wants the next technology, but we have to make sure we’re selecting it strategically and that it continues to support our mission.”
George O’Brien can be reached at [email protected]

Dr. Robert Roose says Massachusetts residents struggling with opiate addiction are also, in many cases, struggling with long waiting times for treatment.
Responding to a troubling rise in drug addiction in the Commonwealth over the past decade, Gov. Deval Patrick’s administration convened a task force earlier this year to come up with solutions. The recommendations are plentiful, and time will tell how effective implementation will be.
“I think it’s very appropriate to characterize this as an opiate addiction crisis,” said Dr. Robert Roose, chief medical officer, Addiction Services, for the Sisters of Providence Health System. “Government and media and other parties who have described opiate addiction as an epidemic are making an honest assessment of what this region and others have been dealing with for a number of years. And we have not seen potentially the worst of the consequences of this crisis.”
One problem the task force sought to address was a shortage of treatment options in the Bay State, where an estimated 120,000 people are addicted to opiates, and roughly two deaths every day are attributed to overdoses — while perhaps 100,000 of those people either cannot access limited treatment resources, or are not trying.
“Everyone is trying to keep up with the current demand for treatment,” Roose noted. “I would say, at this point, patients struggling with opiate misuse are also struggling with longer waiting times to get into treatment programs, and that puts people’s lives at risk.”
The task force’s recommendations (more on those later) encompass strategies for expanding treatment access and boosting educational efforts, but also altering how the insurance industry and correctional system handle addiction, among other goals.
The coalition of more than 35 stakeholders — representing municipalities, hospitals, insurers, social services, and other entities — worked with families, the Department of Mental Health, and a host of organizations to develop a set of recommendations designed to improve the Commonwealth’s opiate-abuse prevention and treatment systems, prevent further misuse and addiction, increase the number of people seeking treatment, and support individuals recovering from addiction.
“These actions will help enhance our network of treatment and recovery services to help communities and families struggling with addiction,” Patrick said. “I hope this work results in more families talking openly about issues of addiction in order to spark the process of healing and recovery.”
Roots of a Strategy
What would become known as the state’s Opioid Task Force stemmed from Patrick’s declaration in March of a public-health emergency in regard to opiate addition. The task force, chaired by Cheryl Bartlett, commissioner of the state Department of Public Health (DPH), was charged with developing policy recommendations to strengthen the Commonwealth’s response to this crisis. The task force eventually made recommendations in several categories, including:
• Expanding and streamlining access to services. In order to meet the escalating demand for treatment, ensure a comprehensive continuum of care, and facilitate access to coordinated care, the DPH intends to expand community-based and residential treatment programs for underserved populations, including adolescents, young adults, and families with children.
• Enhancing opiate education. The DPH will launch a statewide awareness campaign for youth and parents to promote more openness and public dialogue about issues of addiction and recovery. The Commonwealth will also work on strategies to enhance education for medical professionals on best practices in identifying and treating individuals struggling with opiate addiction.
• Addressing insurance practices. The DPH and the Division of Insurance, in consultation with the Health Policy Commission, will conduct a comprehensive review of insurance coverage for opiate addiction treatment. The agencies will consult with clinical experts to develop minimum criteria for opiate abuse and addiction treatment services that will be considered medically necessary for all patients. The task force found that gaps in coverage were impacting services for individuals in need.
• Expanding correctional-system treatment. The Commonwealth will work to provide individuals with enhanced support and treatment for drug addiction when they leave correctional facilities and integrate back into society.
• Expanding peer-support networks. The Patrick administration will work with communities to expand peer support networks comprised of individuals in recovery who provide guidance to those navigating pathways out of addiction.
Patrick also met in June with other New England governors at Brandeis University to discuss a regional response to the opiate epidemic.
Roose noted that he worked in addiction treatment in New York City for a couple of years, and he sees parallels with Western Mass. in how addiction isn’t just entrenched in urban areas, like Springfield and Holyoke, but has spread into other communities, which don’t always have the infrastructure to deal with it.
“It was a bold move by the Legislature to create a task force, and they put forth some strong, bold recommendations, which will hopefully make an immediate — but lasting — impact,” he told BusinessWest. “Recovery is a lifelong process, and treating addiction is something done over time. I expect we’ll be dealing with this for many years to come.”
John McGahan, a task-force member and president of the Gavin Foundation in Boston, said the task force’s approach “addresses a public-health crisis without compromising public safety and … supports communities, families, and the people seeking recovery.”
From Drugstore to Street
The education component of the task force’s recommendations is especially important, considering how subtlely many individuals become addicted, as Roose noted.
“There have been different studies that looked into this, and they reinforce what had become a common understanding, which was that a general overprescribing of prescription painkillers, starting in the ’90s, led to a dramatic increase in access to painkillers and opiates. And many people developed physical dependence because of this increased availability. These include young people and teenagers who began experimenting with prescription painkillers.”
John Morello says the roots of the problem run deeper than young people discovering their parents’ painkillers in the medicine cabinet. A Worcester-based actor and writer who performs Dirt, a one-man show about substance abuse and choices, in schools and colleges across the U.S., Morello said a culture that has become more welcoming to the idea of pills as a solution to problems has helped grease the skids toward higher rates of addiction among young people.
“I think one of the biggest things I’ve noticed is how medicated most students are these days, and how it is a direct reflection of the medicating of their parents,” he said. “We have a generation that has been overmedicated by painkillers and anti-depressants, having children and then being told that their kids have ADHD and need to be medicated.
“No matter what school I go to — maybe more, though, in wealthy areas or private schools — I see kids being medicated for academic performance,” he went on. “I don’t know if it’s because parents and communities are buying into this whole idea that ‘our children are falling behind, and we as a nation need to keep up with China and India,’ or maybe it’s just plain fear, or maybe they truly do want what’s best for their kid and are not getting any other answers besides some anecdotal reports on afternoon talk shows and a prescription from the pediatrician.”
The numbers at some schools are startling, said Morello, recalling a relaxed chat he had with about 25 or 30 students after one of his shows. When the subject of prescription drugs came up, more than half the students said they were on some sort of behavioral prescription, and the ones on Ritalin or ADHD medications had bought into the idea that the pills were helping them be successful students.
“So, there is this overarching message that to fix things, we take a pill,” he continued. “Of course, I question the whole premise most of the time because I don’t even think that what they’re ‘fixing’ is even broken half the time.”
Whatever the reasons for increasing numbers of addicts, it’s not hard to understand how a significant number of those people have moved from the medicine cabinet to the street, where a hit of heroin is typically $10, compared to $30 for one dose of Oxycontin, Morello noted.
“We are seeing the effects of young people who tried painkillers, became addicted to them, and transitioned to heroin,” Roose said. “There’s very clear evidence that, as the number of opiate prescriptions increased over the last two decades, so did the number of treatment admissions and the number of opiate-overdose deaths. As the medical community and others recognized this was a problem, the subsequent decrease in prescribing them led many already addicted to switch to heroin, which has always been readily available.”
Added Morello, “what happens when the patient cannot afford the FDA-approved and legalized habit that was created and nurtured in him by prescriptions since childhood? He or she will either break the habit or find a way to feed it that they can afford.”
Bottom Line
The task force’s recommendations are aimed, at least in part, at breaking those habits, but no one is saying it will be easy.
In fact, Roose said some addicts simply aren’t willing to seek help, and perhaps the best way to reach them is through programs that educate people about safer injection practices and overdose prevention.
“Heroin dependence brings additional risks, including complications that arise from injection use, which sometimes lead to more dramatic social and economic consequences for individuals, families, and the community,” he said. “The good news is that we have treatment — treatment that works — for addiction, but we’re behind the 8-ball, coping with the increased demand.”
Bartlett said the task force wants to expand on a strong, if overextended, treatment system in Massachusetts, and to create a national model for recovery. Roose, who works for a health system with a broad range of inpatient and outpatient addiction-treatment services, knows the battle is only beginning.
“Despite increasing capacity over the past year,” he said, “we’re still coping with the same demand the state is experiencing. It’s a problem.”
Joseph Bednar can be reached at [email protected]
In fact, as senior vice president of strategy and marketing for the Sisters of Providence Health System, it’s part of his job to understand the demographic and medical trends in the region — and how SPHS should respond to them.
“Every year, we do a community health-needs assessment and some ongoing tracking of what’s happening with demographics and what’s happening with diseases in the region,” he said. “And cancer rates in our region are higher than the national trend. Meanwhile, our demographics are older than a lot of regions, and we’re aging in place; there’s not as much outmigration as in some other regions. And as folks age, we’ll continue to see both actual and predicted growth in cancer prevalence.”
In short, “we said, ‘wow, we’ve got some things we need to prepare for.’”
SPHS is doing so with a major expansion of its Sr. Caritas Cancer Center in Springfield, increasing its floor space from 16,000 square feet to almost 40,000 and bringing more cancer services together in one location.
“We’re bringing radiation oncology and medical oncology under one roof, which is ideal for the patient, both from a convenience standpoint and from a comprehensive care standpoint, because they can get all their care in one place,” Fulco said. “And having everyone together in one place is very effective for clinicians because there is quite a bit of interaction between various medical specialists who provide care in the cancer center. So having everything together in one place is very efficient for both caregivers and providers.”
That under-one-roof philosophy is one that has guided the recent surge in dedicated cancer centers around the country and particularly in Western Mass., where Baystate Health’s 65,000-square-foot D’Amour Center for Cancer Care and SPHS’s Sr. Caritas Cancer Center, both built in 2003, pioneered the concept.
In addition to the Caritas expansion, Berkshire Health Systems, which runs Berkshire Medical Center in Pittsfield, opened the BMC Cancer Center last fall and is gradually moving all cancer services under one roof. Meanwhile, Cooley Dickinson Hospital in Northampton, which has collaborated with Massachusetts General Hospital on cancer services since 2009, is now affiliated with that institution and will open the Mass General Cancer Center at Cooley Dickinson Hospital next year.
“Cancer care is a multi-disciplinary disease,” said Dr. Sean Mullally, medical director of the CDH Cancer Care Program. “It requires the input of a medical oncologist, radiation oncologist, and surgical oncologist, and it’s very important, in many situations, to have a collaborative approach from all three specialties.”
Michael Leary, director of media relations at Berkshire Medical Center, said the way cancer patients were shuttled around just a few years ago is not considered acceptable today.

The Sr. Caritas Cancer Center expansion, which will more than double the facility’s floor space, is expected to be completed in 18 months.
That’s why the health system repurposed the original Hillcrest Hospital in Pittsfield to bring those services under one roof, said Ann McDonald, director of Oncology Services for BMC.
“We opened initially with medical oncology, infusion, and laboratory services,” she told BusinessWest. “Over the course of the next year, we will continue to add services, start opening some integrative health services, combining nutrition services, care navigation, social work, and movement therapy.
“The next phase, which won’t open until late this year, is a multi-disciplinary clinic, where patients can see a variety of physicians during treatment,” she continued. “We’ll have palliative-care services in the future. The last phase will be a year from now, when radiation oncology moves from its current site [at BMC] to the new cancer center. Then all our oncology physicians will see patients in one place.”
In this issue, BusinessWest examines the recent evolution of cancer care at area hospitals and why both patients and providers are cheering the effort to bring comprehensive oncology services under one roof.
Come Together
The plans for the Caritas Center expansion, which broke ground in the spring, include medical-oncology offices, including physician offices and examination rooms, on the first floor, and medical-oncology treatment space, including 32 infusion bays, an oncology pharmacy, and laboratory space, on the second floor. The project is expected to take 18 months.
The center is also adding two medical oncologists by the fall bringing that number to five, and has been using space in Weldon Rehabilitation Hospital — which, like the cancer center, is located on the Mercy Medical Center campus — pending the expansion of the Caritas Center.
Bringing more services into one building will offer patients much more efficient, comprehensive treatment, Fulco said. “By having the team together, we’re able to more efficiently deliver those services.”
Another driving factor in oncology, reflected in the design of the expanded cancer center, is the shift from inpatient to outpatient care. “We’re preparing for that; we think more and more care will be delivered on an outpatient basis. Even today, most of it is, except for surgical treatment,” he noted. “Over the years, we’ve seen care and treatment dramatically change, both the way care is delivered and the setting.”
Meanwhile, the first phase of the new BMC Cancer Center opened in November, including the new offices of Berkshire Hematology Oncology, BMC Infusion Services, and the Cancer Center Laboratory and Pharmacy.
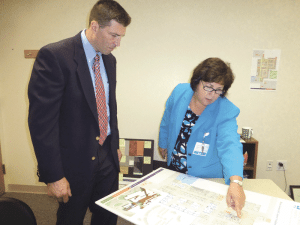
Dr. Sean Mullally and Janet O’Connor say CDH’s affiliation with the Mass General Cancer Center has only strengthened what has been a five-year collaboration.
“The goal was to take all the disciplines and put them together in one location, which happens to be a very beautiful location, the Hillcrest campus of Berkshire Medical Center, formerly Hillcrest Hospital,” he explained. “It’s a really pretty section of Pittsfield, overlooking a gorgeous lake, surrounded by pine trees and walking trails. We wanted a location for patients that was calming and soothing, but also one place they could go to receive as much care as possible. They’re facing enough challenges as it is; we’re making it as easy as possible on them.”
That’s especially true in the Berkshires, he said, which is even farther from cutting-edge oncology services in Boston — or even major highways — than the other regional hospitals building or expanding cancer centers.
“It’s really important to provide this care close to home,” Leary noted. “In any small community, the tendency is to think you can’t get state-of-the-art, advanced care unless you go to Boston or New York — Sloan Kettering or somewhere like that.
“But with the investments Berkshire Health Systems has made in its cancer program over the past several years, we have technology that, frankly, many cancer centers don’t, including one of the highest-end versions of tomotherapy,” he said, referring to a form of radiation therapy. “We do that because we don’t want people to have to go to Boston or New York. Obviously, we’d rather they stay in their community for their quality of life — and it makes it easier on their families, too.”
McDonald noted that BHS can also videoconference with, say, a geneticist in Boston, when necessary, so that a patient doesn’t have to spend five hours on the Pike. “We can send the information and do an entire consultation in a room at the cancer center.”
Getting Better
Cooley Dickinson can videoconference with Boston as well — specifically, Mass General, the institution it merged with last year.
Mullally said the affiliation expands what was already a healthy collaborative partnership when it comes to cancer care, and what is being called the Mass General Cancer Center at Cooley Dickinson will relocate into a new building on the CDH campus in 2015. The cancer center will be operated by Mass General Hospital Cancer Center, he added, and all its physicians will become Mass General doctors.
Expanded services will include access to clinical trials at Mass General Cancer Center, an increased number of chemotherapy and radiation-therapy treatment protocols, increased access to genetic screening and counseling, and, of course, implementation of Mass General’s multi-disciplinary care model, where patients and their medical, radiation, and surgical oncologists can meet in a single appointment to plan all aspects of care.
Janet O’Connor, the center’s clinical nurse director, said the facility emphasizes both state-of-the-art treatment and services that impact body, mind, and spirit, with integrative therapies including acupuncture, massage, and Reiki.
She said the high-tech and high-touch elements of modern cancer care are equally important, reflecting the fact that reducing stress enhances healing. So, while CDH now has access to the type of cutting-edge care available at Mass General, patients will receive treatment in a building designed with a healing atmosphere in mind.
“We’re building a beautiful space,” O’Connor said. “The waiting room space will be very open with lots of light, and we’re creating a green roof with windows looking onto the roof and greenery.” The center will include 18 infusion areas, up to 12 exam rooms, and swing space for the support services, from nutrition to massage. “The idea is to keep the patient with us and bring our people to them, so they can have a consultation with a dietician, or with someone in occupational or physical therapy … we’re providing space where they can go to the patient.”
Patients and families were involved in the design phase, she added, and they will be further consulted on what kinds of committees or programs may be developed down the line.Mullally also stressed the clinical-trial benefits of the Mass General affiliation, as MGH is one of the nation’s leaders in targeted therapy trials in melanoma, brain tumors, and other solid tumors.
“For the most part, if people want access to clinical trials, they need to drive to Boston. In the future, we’ll be able to provide many trials here, so it doesn’t require a ride back and forth,” he noted, adding that subspecialists at Mass General are easy to access when their consultation is needed. “They have an open-door policy; they pick up the phone.”
I Feel Fine
The cancer centers at Berkshire and SPHS are also embracing some new modalities, including the STAR (Survivorship Training and Rehabilitation) Program, an evidence-based education and training program that many hospitals and cancer centers offer to their administrative and clinical staff to develop more effective oncology-rehab services.
“It allows cancer patients, like those who have joint surgery, to go to rehabilitation faster and get better more quickly because of this enhanced focus on their rehab,” Fulco said.
The addition of rehabilitation oncology — combined with physicians’ new ability to coordinate care in one building — adds up to better quality of life for patients in Pittsfield, McDonald said.
“For so long, helping people survive was the primary outcome. As survival improves, quality-of-life treatment takes on additional meaning,” she said, which is why it’s important to add elements like exercise and rehabilitation; integrative services like yoga, Reiki, and acupuncture; and nutrition education. In fact, the center will invite guest chefs in for demonstrations on cooking healthy food.
Meanwhile, Leary said, “the Berkshires are a very good place for artists, and we’ve lined the walls of the cancer center with pieces of art by local artists. We’ve been able to display the talents of our community there.”
All the new cancer centers take the healing environment into account, Mullally said, and CDH is no exception. In the end, though, what drives the evolution of cancer care is that emphasis on bringing services to patients under one roof, and lessening their anxiety at what may just be the worst moment of their life.
“It makes it more convenient, and patients have better outcomes, if all the specialties are working together at the same time,” he said. “It makes for more patient-centered care.”
Joseph Bednar can be reached at [email protected]
James Caldarola, left, and Jeffrey Halls say qualified professionals customize hearing aids to fit a person’s preferences as well as their home and work environments.
“He told me he sat on a perch in a tree for days without any luck,” Halls, co-owner of Baystate Hearing Aids in West Springfield, recalled. “Then, he looked down and saw two deer right beneath him. He hadn’t heard them moving through the woods, and that prompted him to seek help for his hearing loss.”
This story is typical of what he hears from customers, he went on, adding that the man knew his hearing had declined, but like many people, failed to address the problem until it affected an activity he loved.
Statistics from the Hearing Loss Assoc. of America show that 48 million adults in the U.S. suffer from hearing loss. It is the third-most-common physical condition after arthritis and heart disease, and although most people associate the condition with aging, 65% of Americans with hearing loss are under age 65, and the majority are in the workforce.
But most people wait five to seven years to seek help. Experts say some think their hearing loss is not advanced enough to do anything about it, while others, working with outdated information, don’t want to be seen wearing a hearing aid.
Indeed, today’s hearing aids have kept up with advances in technology, and some are so small they are almost invisible to the eye. There are a wide variety of styles to choose from and a vast array of programs that are coupled with the computer chips inside them. In fact, many automatically adapt to different physical settings and have Bluetooth connectivity.
“People often avoid seeing a specialist about their hearing loss because they think a hearing aid will make them look old. But a hearing loss is more obvious than today’s hearing aids,” said audiologist Susan Bankoski Chunyk, who owns Hampden Hearing Center in East Longmeadow.
James Caldarola agrees. “People are surprised at the size and clarity of the hearing aids available today, and with Bluetooth, they work better with phones and TVs than they did in the past,” said the co-owner of Baystate Hearing Aids. “Hearing aids can’t restore a person’s hearing, but they can make it a lot better. And since most hearing loss is gradual, many people aren’t aware of what they could be missing.”
Chunyk explained that a person who is gradually losing their hearing may not notice they have stopped hearing environmental sounds, such as crickets chirping or the click of a directional signal in a car. “But family members, friends, and co-workers may notice the person is having trouble understanding them.”
People often compensate for the problem by talking more loudly to the person with the hearing loss or repeating themselves.
But it’s not a good solution, and ignoring the problem can lead to other health issues, including dementia.
“Mild untreated hearing loss doubles your risk for dementia, moderate untreated hearing loss triples it, and severe untreated loss makes dementia five times more likely,” said Chunyk. “In addition, research shows links between untreated hearing loss and depression, anxiety, poor self-esteem, fatigue, isolation, and loneliness.
“It is important to act sooner rather than later because better hearing improves every aspect of a person’s life,” she went on. “But, unfortunately, only 15% to 20% of people with hearing loss ever seek help.”
However, the problem is growing and is now linked to a variety of health conditions. “New research shows hearing loss is twice as common in adults with diabetes, smokers, and people with heart disease,” she told BusinessWest. “It is also common in people with kidney disease.”
Hearing loss can be hereditary or related to aging, occupational noise, or frequent use of earbuds with the volume turned on high. “In many of these cases, it is preventable,” Chunyk said, adding that using earbuds for extended periods of time with the volume turned up can be dangerous.
Caldarola said there is a need for increased awareness about hearing loss along with the technological advances that make today’s hearing aids comfortable to wear and smarter than they were in the past. “Some people don’t think they have a loss because they can hear things far away or can hear some sounds very well. But we recommend that people over the age of 40 get tested every two or three years,” he said.
Technological Advances
Most hearing aids sold in the U.S. are digital, and are a vast improvement over older analog models, which were difficult to adjust and amplified background noise as well as speech. Today’s models respond to noise in the environment, so people don’t have to experience problems associated with feedback and echoes.
“Today’s hearing aids are all digital, which allows us to customize them to make sounds clear and natural,” Caldarola said, explaining that people hear over a range of sound, which involves tone and pitch.
Chunyk concurred. “Thirty years ago, we used to adjust hearing-aid settings with a tiny screwdriver; this limited the range of possible adjustments,” she said. “But today’s digital instruments are programmed via the computer, which makes the adjustments more precise and personalized to an individual’s needs. The newest hearing aids are sleek and discreet, so they are less visible and more comfortable to wear. In fact, some people who get them are so excited about how small they are that they take them out and show them to their friends.”
The new devices are also adaptable. “In the past, if someone got a hearing aid and their hearing changed, they were forced to get a new one. But today, we can reprogram a hearing aid in minutes,” Halls said.
A hearing test will determine whether a person will benefit from a hearing aid, and if it can make a difference, they will be shown models that meet their cosmetic preferences and lifestyle needs.
“Not all hearing aids are the same,” Chunyk said. “We pick a category that is appropriate for mild to moderate hearing loss or a severe degree of loss. There are also super-power or ultra-power aids for people with profound hearing loss.”
Halls said people hear over a spectrum, which includes high to low pitch. “The ability to hear high pitches makes speech clear,” he explained, adding that the newest hearing aids will allow people to hear sounds such as a bird chirping outside their window, although the pitch may sound a bit different than it does to people without a hearing loss.
Hearing aids are classified by the U.S. Food and Drug Administration as medical devices, but many people confuse them with over-the-counter models that can be purchased at retail stores or via the Internet.
“The over-the counter models are simply sound-amplifying devices,” Chunyk noted, adding that she has patients who have told her they purchased them, then threw them away because they didn’t help.
“Hearing loss is not just about volume; more often, it is about clarity, which can only be addressed with professional help,” she continued, adding that, although most hearing loss cannot be treated medically, hearing aids can do a lot to restore hearing.

Susan Bankoski Chunyk shows off a device that can stream sound from a cell phone to a hearing aid with the touch of a button.
For example, some have a feature that allows them to automatically adjust to a quiet place or noisy setting.
“If the person is in a quiet room, the hearing aid will go into surround-sound mode,” said Chunyk. “But if they walk into a noisy restaurant with competing noise, the instrument will activate directional microphones which automatically focus forward and reduce sound from the side and back so the wearer can hear the person in front of them.
“At the same time, there is noise-reduction circuitry inside that will recognize a voice and focus on it, while reducing everything else,” she continued. “Older hearing aids often required people to push a button to make changes, but today’s models do it automatically with more precision.”
Another major improvement is the reduction of feedback. “Older styles used to give off a high-pitched squeal if a person hugged someone or did anything that blocked the aid,” Chunyk told BusinessWest. “But today’s technology controls feedback much more effectively.”
These high-tech hearing aids come in many styles, but many factors go into choosing the one that is right for each individual. “Part of the selection process is knowing what the person’s preferences are for sound and what type of environment they are in every day,” she explained. “The needs of a very active person are different than someone who is home all the time just watching TV.”
New Features
Today’s hearing aids work well with other electronic devices. “There is connectivity between hearing instruments and mobile phones, land lines, and televisions,” Chunyk said. “For example, one manufacturer makes a model that allows a person to wear a small device around their neck that is paired with their cell phone. When the phone rings, they push a button on the device, and it streams the sound to their hearing aid through a microphone. If there is too much background noise, they can hold the streamer close to their face to eliminate it.”
Caldarola noted that Bluetooth technology has resulted in hearing aids which automatically cue into a phone. “In the past, people had to push a button to hear on the phone, but now many models are automatic and have features that reduce background noise without manual intervention, so speech is more intelligible,” he explained.
Other accessories include lapel microphone clips that can be put on another person’s collar in a place like a noisy restaurant. “It sends the person’s voice to the hearing aid,” said Chunyk, adding that several manufacturers have hearing aids that are made to be compatible with iPhones and work through free apps.
However, there is a lot to know about purchasing a hearing aid, and Caldarola and Halls offer the following advice:
• Ask people who wear hearing aids where they got them and if they were happy with the service;
• Ask about the seller’s return policy and if they can repair hearing aids on the premises;
• If you have been fitted with a hearing aid and experience a problem, ask for help in resolving it. Most people need several visits before the settings reflect their preferences;
• Ask if additional features can be added later on, like Bluetooth or a remote control; and
• Ask about any additional costs that will be charged after you purchase the hearing aid.
Halls said fitting a hearing aid is a process. He and Caldarola advise clients to wear a new device for a week, then return so adjustments can be made. “Sometimes it takes several visits to achieve a goal.”
In some instances, they have had to go to the person’s home to solve the problem. For example, one woman who complained her refrigerator sounded too loud discovered it was too loud and she needed a new one.
But in many cases, hearing aids can be fine-tuned. “We can add a program for golfers that will eliminate wind noise,” Halls said, citing one example.
Ringing in the ears can also be masked. But people need to be realistic, because hearing aids have limitations, and some situations may continue to be problematic, such as hearing a person who talks rapidly, mumbles, or speaks very softly. “In these instances, even with a hearing aid, it can be difficult for the person to understand 100% of what is being said,” Caldarola said. “It’s unrealistic to expect to restore hearing to the way it was when a person was 16 years old.”
But hearing aids have internal memories, and experts can tell how often it switches from one mode to another, which helps the fitter to make adjustments.
Moving Forward
Caldarola has two patents for hearing aids, and his latest model is called the Micro-Air. It is suspended in the ear canal, and what sets it apart from other instruments is that it allows natural sounds to pass through the ear canal while amplifying the frequencies that the person who wears it is missing. The result is the elimination of background noise and echoing which plagued many people in the past.
Such advances will continue, and technology has come so far, there is no reason why people should shy away from the thought of visiting a hearing specialist.
“More than 75% of people with hearing loss could benefit from a hearing aid,” Caldarola said. “If the loss starts affecting your life, it’s time to get checked.”
Chunyk concurred. “People shouldn’t wait,” she told BusinessWest. “It’s a whole new world.”
 When Boston’s Beth Israel Hospital merged with Deaconness Medical Center 18 years ago, Joanne Marqusee was there to witness the aftermath.
When Boston’s Beth Israel Hospital merged with Deaconness Medical Center 18 years ago, Joanne Marqusee was there to witness the aftermath.
And it wasn’t pretty.
“I learned about what organizations should not do when they merge,” said Marqusee, the new president and CEO of Cooley Dickinson Hospital in Northampton, taking over for Craig Melin, who had steered the CDH ship for a quarter-century and through both quiet and turbulent seas.
With Cooley Dickinson having recently finalized a merger of its own, with Massachusetts General Hospital, she reflected on the smoothness of that transition compared to the tumult that followed the Beth Israel Deaconess deal in 1996.
“Being across the street from each other, in some ways it seemed like the perfect merger,” said Marqusee (pronounced ‘mark-a-see’), who joined the BI team in 1992. She noted that the two institutions had complimentary specialties; for example, Deaconess was known for surgery, while BI had a stronger medicine program. “On paper, it seemed like a match made in heaven. But in some ways, there really wasn’t enough attention paid to how to bring two cultures together, how to manage people through that situation. And it really matters.”
Staff from the two Boston institutions became notoriously suspicious of each other. “People didn’t want to work in teams. Fortunately, I had been there only three years, so I didn’t define myself as a ‘BI person.’ I didn’t have this bias based on what side of the street I worked on. That didn’t define my contribution to the corporation.”
On the bright side, however, “when the organization was in such flux, with people coming and going, there were a lot of opportunities,” she said. “So I was given more and broader responsibilities — often in areas I didn’t necessarily have any background in.
“I kind of learned over time that management is management,” she continued. “Particularly as a non-clinical person moving up in healthcare, I applied the same approach to problems involving people, whether in a clinical or non-clinical area.”
Having most recently served as executive vice president and chief operating officer at Hallmark Health System, located just north of Boston, a job she accepted in 2009, Marqusee is embracing her first stint in the CEO’s chair, and has been pleased with the way Cooley Dickinson and Mass General are coexisting.
“The distance makes it almost easier; people don’t feel threatened,” she told BusinessWest. “And they have been terrific. We can call there for help; they have such intellectual capital. I spend at least one day a month at MGH and feel like a part of their team, which is nice.”
Matthew Pitoniak, who chairs the CDH board and led the search committee tasked with replacing Melin, is impressed with Marqusee’s acumen for bringing different teams together within an expansive health system, one that includes the hospital, the Cooley Dickinson VNA, and a number of other practices.
“We set out to identify a person capable of leading our care system into the future,” he said. “We also wanted a strong collaborator who can bring together the components of our care system for optimal patient care, and a leader who could build upon our affiliation with Massachusetts General Hospital while strengthening our local system.”
On a Mission
Marqusee was raised outside New York City in a family that was politically involved and socially conscious. “All my siblings and I ended up doing mission-based work in one way or another.”
Attending Cornell University, she didn’t know what career path she wanted to take, but she had a love for international affairs and languages, so she majored in linguistics. But she eventually felt a call to nonprofit management.
“I thought, ‘should I be a social worker?’” she said. “But I had a sense that a better fit would be to look at how whole organizations work and to make an impact there.”
While earning a master’s in public policy from Harvard University’s Kennedy School of Government, she decided she was more analytic than she’d suspected, and wound up working in New York Mayor Ed Koch’s first administration. There, in 1984, she was exposed to the Health and Hospitals Corp., which ran 11 public hospitals, five nursing homes, and dozens of ambulatory-care sites. It was a $2 billion corporation with 50,000 employees.
“After about a month, I realized I wanted to be in the healthcare world,” she said. “It was so complicated; I had the sense I could spend decades in healthcare and have different roles and always be learning.”
From there, Marqusee joined Beth Israel in 1992 and eventually ascended to senior vice president of operations for the merged system. She eventually ran most support and ancillary areas of BI Deaconess, including the Laboratory, Pharmacy, Radiology, and other clinical areas, as well as non-clinical areas such as housekeeping and patient transport.
“I got an appreciation for the fact that hospitals aren’t just doctors and nurses, even though TV and movies tell us they are,” she said. “I really got to see how, if you could tap the creativity of what’s considered support staff, it can make a great deal of difference.”
Take transport personnel, for example. “Follow one of them around for a day and see what a difference they make in healthcare,” she said, noting that patients are often already anxious and confused as they’re being moved from a room they know to somewhere unfamiliar, and a transporter who engages that patient with information and compassion makes a huge difference. “If nobody talks to them, it can be quite frightening.”
Eventually, though, Marqusee sought a new challenge. “I loved BI Deaconess; I loved the fact that it was an academic center. But personally, my interest and skill set is on the clinical side of medicine, and while teaching and research are good — we want to find a cure for cancer and teach the physicians of the future — my skills at managing people, bringing people together, can make more of a difference on the clinical side. I wanted to work in a community hospital.”

Joanne Marqusee takes over at CDH in an era of growth and new construction for the community hospital.
“Hospitals are complicated cities with 24/7 operations, involving doctors, nurses, phlebotomists, transporters, people who make sure supplies get where they need to go — it’s this complicated dance to make sure everything gets done right,” she said.
“There are a lot of policy issues, but also the question of, how do you make such a complex organization work better? How do you make teams work better?,” she went on. “The emergency room, for instance, is an amazing thing — think of all the different parts that have to come together to move everyone from A to B.”
In her five years at Hallmark, she said, she helped standardize practices and managed to improve both patient and employee satisfaction, while better engaging physicians — even while battling the onset of a recession that made life difficult for all community hospitals.
“In 2009, it was awful. People were losing their jobs, and if not them, their spouse was losing their job. It had a huge effect in all hospitals,” she said. “We were able to get through that and find ways to reduce costs while improving care. As a non-healthcare person, I like to apply the quality-improvement approaches of other industries, like the LEAN approach that Toyota uses. That’s very helpful in bringing frontline staff together, standardizing workflow, and finding ways to keep the patient at the center.”
Marqusee added that she wants employees at all levels to enjoy their jobs. “That’s important. People like it when they have fun and work as a team. For staff, it’s important to balance the seriousness of what they do with enjoying the community they work in. People come to healthcare, usually, because they care about what they’re doing.”
Western Swing
While Marqusee loved being in a community hospital, she occasionally missed the learning experiences of an academic medical center, and the opportunity to lead a Mass General-affiliated CDH appealed to her. “I wasn’t sure what I wanted to do, but when this came up, I was really excited; it seemed like the perfect job for me. It’s a community hospital that’s very well-regarded with high quality scores — very, very impressive.
“I hadn’t thought I would leave the Boston area, but my twins grew up and were in college, and my husband recently retired,” she went on. “Northampton seems like such an ideal area, really, with the culture and level of activity here. We can be connected with Boston, and not far from New York.”
She cited the hospital’s well-known infection-control efforts as one example of how CDH has been a leader.
“The focus on quality is clearly embraced here; physicians and staff are proud of being innovators,” she said. “Some people think hospitals and healthcare systems are solely based upon healing people, but harm can happen in hospitals. We want to make sure people don’t leave with an infection, and we make a priority of that. The housekeepers are passionate about this issue. They think, ‘what I do makes a difference in whether patients get sick here or not.’”
At the same time, Marqusee takes the reins amid controversy over a state investigation into several serious incidents in the Childbirth Center, including two infant deaths and a failure to properly treat high blood pressure in a mother, leading to a stroke that caused her death. The hospital has since reorganized the center and its affiliated nurse-midwife practices and launched a corrective action plan.
“We’re trying to be out there and communicating,” she said, noting that the recent tragedy comes on top of stress that already existed related to the Mass General merger and Melin’s announced retirement. “It’s been a year and a half of people not knowing what’s going to happen. So we communicate with them the good and the bad, the issues we need to work on, trying to be honest so we can get better. We’ve been as open as we can about the Childbirth Center to staff and the community.”
She credited Melin with steering the hospital with a steady hand amid an ongoing shift in the healthcare industry toward accountable care, which emphasizes efficiencies of treatment. “In America, we use more healthcare, but we don’t necessarily have better health outcomes.”
She said Northampton is a progressive community when it comes to understanding, for example, that more MRIs are not necessarily better, but added that the industry has a long way to go toward a less-wasteful system of care.
“Physicians get paid to see patients; they don’t get paid to talk on the phone,” she noted as another example. “But even five minutes on the phone can be more valuable than having them come into the hospital, be exposed to more germs, and maybe be encouraged to take an unnecessary test.”
What Cooley Dickinson can do, Marqusee said, is improve its own processes, and that begins with better communication between departments.
“We’re trying to understand where our systems do not work as well as they could, to connect the departments with one another, communicate better between the day shift and evening shift,” she said.
“The departments themselves run quite well; this place is strong operationally. They don’t need a leader to come in and tell food services or the ICU how to run their department, but they could use help linking to one another in interdisciplinary teams,” she continued. “Most errors in healthcare tend to be around communication or handoffs, radiology to ICU, day shift to evening shift, communication between nurses and physicians, nurses and technicians. I’ve been interested in finding where the gaps are and setting priorities for improvement projects.”
Take the Emergency Department, for example. “That’s such a complicated place — the doorway to the organization in many ways; a hospital’s reputation in the community tends to rise and fall with the Emergency Department,” she told BusinessWest. “But the ED staff themselves say we could do much better with the way we communicate with people upstairs, so in the fall, we’re launching a major project to reorganize how we work in the ED, make it even better.
“Right now, patients are happy with it,” she stressed, “but if they spend less time here, it would make them even happier.”
Talk It Out
In her first two months on the job, Marqusee has been busy spending time in many different areas of the hospital and, in fact, the entire CDH network. “I’m trying to make people understand that it’s not just a hospital; Cooley Dickinson is also the VNA, off-site physician practices, radiology, and rehab,” just to name a few, she said.
“I’m also trying to meet people from different shifts — nights, weekends, evenings. It’s a whole new world at night, so I’m trying to understand their challenges, too. I’m just trying to create some visibility; I don’t want anyone to think the CEO is a suit in the corner office they can’t talk to. I want to have a culture that’s not hierarchical, where the frontline staff understand that I care about them, and they can talk to me.”
The bottom line, Marqusee said, is that, despite recent challenges, a well-regarded hospital system has the ability to improve, and that’s not a task she takes lightly.
“I feel like this community values Cooley Dickinson, and that doesn’t just happen,” she said. “It’s years of reaching out and providing valuable services.”
Joseph Bednar can be reached at [email protected]

Victoria Healy stands in the front lobby of the new HealthSouth facility, complete with a mural depicting the signature clock tower in the Ludlow Mills complex.
“It was difficult giving tours there — that facility was not an easy sell,” said Healy, who gave more than a few over the years in her role as controller.
There were five floors to negotiate, she told BusinessWest as she talked about the former Ludlow Hospital, an acute-care facility built in 1907, adding that the elevators were old and slow, the rooms had multiple patients and shared bathrooms, and the rehab areas were quite small.
All this made for competitive disadvantages at a time when patients and their families were becoming far more discerning about where and how they receive care, and doing their homework before choosing a provider.
“What we’re finding now is that people are really educated, and if they’re going to have surgery they believe will require rehab after the fact, like having both knees replaced, they’re doing the legwork up front,” she explained. “They’re figuring out where they’re going to go before they need it.”
These days, giving such tours is a very welcome assignment for Healy, now the facility’s CEO, and anyone else who gets to do the honors.
That’s because the new, $28 million HealthSouth, built at the Ludlow Mills complex and opened last December, is state-of-the-art in every sense of that phrase — from its pending LEED (Leadership in Energy and Environmental Design) certification to the private rooms and accompanying spacious bathrooms; from the large inpatient gym, where occupational, physical, and speech therapists work with patients, to the courtyard, which doubles as what Healy called a “functional therapy gym” (more on that later).
“Tours are a lot more fun here — this building sells itself,” she told BusinessWest, adding that there have been dozens of visits in recent weeks from prospective patients and their families, town officials, the press, and other constituencies.
But while the new, 53-bed, 74,000-square-foot HealthSouth is a model of the present and, in many respects, future of rehabilitation services, there is also a nod — actually, several of them — to the past. In this case, it’s the hospital’s new home, the massive former jute-manufacturing complex that is now the site of an ambitious redevelopment project being undertaken by Westmass Area Development Corp.
Indeed, the HealthSouth facility is one of the first undertakings within this initiative, which includes both new construction and repurposing old mills, and those constructing and then decorating the hospital acknowledged the rich history of the site.
For starters, 100,000 bricks salvaged from some of the dozens of historic stock houses that populate the property were used in the construction of the new hospital. They can be seen in the front lobby, which also features several planed wooden beams from those stockhouses, several photos of the mills, and a large mural featuring the signature clock tower that dominates the property and has become the town’s most recognized landmark.
Meanwhile, a mix of artwork adorns corridors throughout the facility — a colorful collection of photographs of area landmarks (everything from Mount Greylock to Westfield’s Tekoa Country Club), as well as a number of vintage photos, many a century or more old, including many of the old mill complex and the nearby Putts Bridge that links Ludlow with Indian Orchard, as well as other town landmarks.
Healy said an early favorite among patients and staff alike is an image from the maternity unit at the former Springfield Hospital, circa 1905, showing nine infants on one large cart.
“We originally thought those were loaves of bread, but they’re babies,” she said. ‘Times have definitely changed.”
For this issue, BusinessWest took one of the many tours being offered these days by Healy and her staff to gain some perspective on what this new facility means for the organization in terms of serving patients and achieving desired growth.
It’s Not Run of the Mill
Healy, who joined HealthSouth’s Ludlow operation in 1999 — a few years after the corporation acquired it from Advantage Rehabilitation, which set up shop soon after Ludlow Hospital closed its doors in the early ’90s — said administrators have known for some time that larger, more efficient, and far more modern facilities were needed.
Indeed, while the company has a reputation for good outcomes for its patients and has long enjoyed a high occupancy rate (roughly 90%), the multi-level, 60,000-square-foot facility presented some real challenges.
The 53 beds were placed in far fewer rooms than the current facility, she explained, noting that there were often three or four patients to a room. This created issues with privacy and infection control, but also presented some logistical problems.
For example, as the patient population shifted, gender-wise, patients would have to be moved, often several times during a typical two-week stay, said Healy, adding that this was an inconvenience for both patients and their families.
“We had such a high occupancy rate, in order to accommodate more patients, we had to do a lot of room moves,” she noted. “In an average length of stay of 13 days, a patient might move three or four times.”
And then, there were the multiple beds and common bathrooms, which, suffice it to say, were not the highlights of those aforementioned tours.
“When the younger generations toured and saw the three- and four-bed rooms and the shared bathroom, they were not interested in coming to our hospital,” Healy noted, “especially when they came from either Baystate or Wing and the new units at those facilities, which featured all private rooms.
“And the bathrooms we had at the old hospital were more like toilets,” she went on. “The sinks were outside the bathroom, and the showers were toward the nursing unit. It was more like a gym shower.”
These and other problems and challenges are now talked about nostalgically, if that’s the right term, by HealthSouth’s staff of 225.

The inpatient gymnasium can host dozens of patients and therapists, and represents a marked improvement over facilities in the former HealthSouth Rehabilitation Hospital.
“It’s a huge change — like night and day,” said Healy with a laugh, adding that the new facility allows for the same patient outcomes, a better patient experience, and a far more appealing environment in which the staff can work.
All of the above became evident as Healy offered BusinessWest a tour, starting outside her office in the administrative area. Nearly 20 people now work in one designated area — where before they were spread throughout the old hospital — allowing for better communication and improved productivity.
But the hospital really exists for its patients, she said, before moving quickly through the lobby to an outpatient-treatment area that represents a vast improvement over the same facility at the old Ludlow Hospital, enabling HealthSouth to better compete in a crowded field of outpatient-service providers, which is a small but still-important component of the business.
The main thrust is inpatient care, she said while moving on to the two wings with patient rooms for those recovering from everything from stroke and other neurological disorders to spinal-cord injury; from amputations to cardiac and pulmonary conditions.
While these rooms have become a strong selling point for those doing that aforementioned legwork that Healy described, there are many other amenities.
These include a spacious day room where patients and their families can relax and spend time together. Activities range from bingo to church services, said Healy, adding that there is another gathering space unofficially named the ‘night room,’ she noted, because it doesn’t have the huge windows that define the ‘day room.’
Around the corner is the large inpatient gym, which can accommodate several dozen patients and therapists at one time. And then, there’s the large courtyard, which, as she said, doubles as a functional therapy gym. There are stairs, handrails, and several slight changes in elevation, Healy noted, adding that navigating all this can certainly assist many patients in their recovery efforts.
“One of the challenges that many patients have as they’re learning, especially after a stroke or a car accident, is that it’s very difficult for them to learn to walk on different surfaces,” she explained. “So here, there are stairs, ramps, brick, concrete, stone, and sand. After a life-changing event, it’s very difficult to learn how to reambulate on surfaces like this, so we’re excited about what we can do here.
“Also, I think it’s good therapy for the soul to have the fresh air and the sunshine,” she went on. “Our goal is to get people back to their lives, and this [courtyard] is closer to life than anything a hospital can simulate.”
The facility has been closed through the long, harsh winter, said Healy, but now that spring has finally sprung, patients and their therapists are taking full advantage of the opportunities afforded them.
The new hospital comes complete with a large amount of shell space, said Healy, adding that the ultimate goal is to expand into that space with more patient rooms.
To do so, HealthSouth will have to convince state health officials there is sufficient need, she said. At the moment, this would be difficult to do because most competing facilities have lower occupancy rates.
“There is space for an additional 17 beds, and it’s our goal to eventually expand into it,” she said, noting that, as the population ages and need for rehab services rises, this space will eventually be put to use.
Making More History
That shell space is currently not on the agenda for most of the tours being given at the new HealthSouth, but there are plenty of other things to see and experience, said Healy, reiterating, again, how much more enjoyable it is to introduce people to this facility than the old hospital just a few blocks away.
“It’s the best part of my day,” she told BusinessWest, adding that the new facility provides the room to grow and an environment in which patients and staff can thrive.
Which means it’s a place where more history can be made.
George O’Brien can be reached at [email protected]
By the time an effective vaccine was developed and distributed in the fall, however, the H1N1 threat had begun to ease up. “It was a flu that went through the entire summer and into the fall, when the traditional flu season was supposed to be starting, and then it started to tail off and disappear,” said Carol Wojnarowski, an RN and infection-control manager at Holyoke Medical Center. “It was a very unique situation. That’s how pandemics get labeled — it’s out of season, it’s worldwide, it usually moves rapidly, and it can be a significant disease for those who can’t fend it off.”
Wojnarowski and her staff — and infection-control personnel at all area hospitals — are among the community’s front-line defenses against such threats, along with local and state public-health officials. When threats emerge, their concerns range from making sure enough masks are available to protect people against airborne transmission to working with pharmacies to rotate antibiotics, to preserve their efficacy.
“We’re always working with other departments, from microbiology to central supply sterilization,” Wojnarowski added. “All these have to be moving together. One won’t work on its own.”
Not every infectious disease is communicable among people, she was quick to note. “You can get tetanus from a dirty nail or a rusty fence, but I can’t give you tetanus. But smallpox, chicken pox, measles, flu, I can give those to you and the person next to you. We have strategies in case we have a pandemic in the community and our vaccines aren’t suppressing it, so we can keep it under control.”
Mary Ellen Scales, an RN and chief infection-control officer for Baystate Health, said outbreaks of flu or a norovirus in the community will often be reported by the Department of Public Health, while, in other cases, a surprising number of patients with similar symptoms will show up in the emergency room, triggering an alert.
But she was quick to add that a significant part of her department’s job has nothing to do with infections and viruses that show up in the community. “Part of infection control is actually prevention. Chasing the horse after it’s left the barn is infection control; not opening the door in the first place is infection prevention.”
Indeed, infection prevention is serious business for hospitals. According to the Centers for Disease Control and Prevention (CDC), hospital-acquired infections are the fourth-leading cause of death in the U.S., and are responsible for tens of billions of dollars annually in healthcare costs.
“We have a responsibility to make sure patients, staff, visitors, and community members who come to Cooley Dickinson Hospital or its satellites are protected from transmittable infectious diseases,” said Linda Riley, an RN and manager of infection prevention at CDH. “We look for certain diseases in the hospital, and infections related to devices people use — IVs, catheters, tubes in the lungs that help them breathe. We look for infections in people having certain procedures and surgeries.
“We work as a team to keep our whole community safe where there’s a community exposure,” she noted. “I would alert our medical staff members, all our offices, let them know what they should expect, what the symptoms are, what they should do if people end up at their offices with measles or flu or something else.”
But where CDH has made major strides, she explained, is reducing the threat of infection inside the hospital.
“We’ve developed improvement plans to reduce the threat of infections,” Riley said. “We do orientation and education for staff, patients, and community members. We implement best practices, and I’m always on the Internet, reading infection-control journals and blogs, looking for new ideas, things we can do to create a safer environment for patients and staff.”
Just Breathe
Take, for example, ventilator-associated pneumonia (VAP), which is usually serious and caused by bacteria, which can be resistant to antibiotics. According to the Centers for Disease Control’s National Healthcare Safety Network Report, Cooley Dickinson’s efforts in preventing ventilator-acquired pneumonia place the hospital in the top 10% of the nation’s medical/surgical ICUs.
And that’s a big deal; patients on ventilators have a 32% mortality rate in the short term, but it rises to 46% when pneumonia is introduced.
The culture shift began in 2005 when a team of respiratory therapists, physicians, nurses, quality-improvement staff, and infection-prevention specialists adopted a set of instructions from the Institute for Healthcare Improvement known as the ‘IHI ventilator bundle.’ The bundle offers a series of interventions determined to be the best evidence-based practices related to reducing the risk of VAP to patients.

Carol Wojnarowski says infection-control work in hospitals involves a number of departments effectively working together to identify — and minimize — risks.
The hospital’s prevention strategy — which works, since it hasn’t had a VAP case in three years — includes making sure patients’ heads are elevated and heating the ventilator tubing to body temperature before use; if they aren’t heated, the gas that passes through them can turn into water vapor, which is a potential breeding ground for contaminants. Doctors at CDH also use closed-suction catheters, which allow them to clean secretions from a patient’s airway while maintaining ventilation, which also cuts down on the risk of infection.
A similar team was assembled at Baystate, which also adopted the IHI ventilator bundle in 2005 and, like CDH, witnessed an almost total elimination of VAP incidents. That followed on the heels of other infection-control measures, like installing alcohol hand rubs throughout its hospitals. “It’s important for healthcare workers to clean their hands,” Scales said.
Cooley Dickinson has taken a high-tech approach to hand hygiene, installing an electronic system, called the DebMed GMS, that monitors whether doctors, nurses, and other care providers are cleaning their hands before seeing patients.
An electronic box at each station keeps a tally of how many provider-patient contacts are preceded — or not — by hand disinfecting. Each department then discusses the findings at staff meetings to develop goals and strategies for improving compliance rates.
Again, this is a serious matter. A study conducted at Duke University Medical Center showed that a 1% increase in hand-hygiene compliance results in annual cost savings of $39,650 for a 200-bed hospital, due to fewer incidents of germ transmission requiring further care and longer stays.
Cooley Dickinson has also taken a cutting-edge approach to cleaner patient rooms using an ultraviolet disinfecting technology known as Xenex Px-UV. The system uses UV light to kill drug-resistant organisms like MRSA, VRE, and Clostridium difficile, or C. diff — which, by itself, infects 165,000 hospitalized patients annually, and about 9,000 of those die, according to the CDC. But at CDH, the presence of C. diff dropped by 82% in just the first four months after the introduction of Xenex.
Home Invasion
Wojnarowski said the report of a widespread pathogen in the community is followed by communication with public-health officials and procedures on everything from quarantines to immunizations. Hospital policy also requires care providers to be fully immunized against transmittable diseases.
But she also emphasized the importance of monitoring and preventing infections that develop inside the hospital.
“We invade the patient a lot; we put catheters in their veins, their bladder, their lungs. And those therapies, though they help the patient and provide relief in some ways, are also a pathway for bacteria to get in.”
That’s why Holyoke Medical Center has established guidelines for how long a catheter or IV can stay in, and how to put a medicated dressing around the catheter and insertion site.
“We’re always updating our guidelines, our patient-care practices, always consulting with operating-room people, sterilizing equipment — what can we do better to clean equipment, keep it sterilized? What are the latest strategies out there?” Wojnarowski explained. “It extends to purchasing equipment, too. For example, sometimes it’s cheaper to buy something disposable versus something we have to sterilize.”
Riley agreed. “We’re part of the equipment-management process, and we look for things that make hospital procedures safer.” For example, IVs must be disinfected with alcohol swabs, but CDH has started using alcohol-impregnated caps that keep the port disinfected. “We found this made our IV-related infections go away. We’re always looking for new things that come on the market and new practices to help us prevent infections.”
She said her job is enjoyable, if only because no two days are the same. For example, “environmental sources of infection are a concern when we do construction, so we do risk assessment, decide what protective barriers need to be in place, and do regular inspections. We do water and air testing to make sure they’re clean for the staff.”
Scales said her team gets support from the Mass. Department of Public Health, the Centers for Disease Control and Prevention, and other bodies dedicated to preventing infection both inside and outside a hospital’s walls.
“We also get calls all the time from people in the community, clinics, doctors’ offices, about how to manage certain things. I got a call from a barber who wanted to teach infection control in hairdressing. That’s fascinating. People are more aware of the fact that infections can be passed — and that they can be prevented.”
Those relationships with state and national agencies can be onerous, too, Wojnarowski added, because organizations like the Joint Commission demand rigorous record-keeping. “We’ll have to provide a log book for temperatures in refrigerators, to prove that vaccines are stored at the right temperature,” she said. “A lot of stuff is very tedious, but it’s all about keeping people healthy, because healthcare does have risks. The therapies and treatments people undergo are not risk-free.”
Riley added that her department works closely with infection-control officials in other hospitals to support each other and share strategies that work. “We help each other problem-solve, do educational programs, and e-mail each other when we have questions. I think it’s the most successful example of hospital collaborations and communications. Our relationships are everything — knowing whom to call, when to call, and knowing you trust these people.”
Impossible Task?
Wojnarowski said they need that network because of how demanding their role is.
“The government says to the hospital, ‘improve this number, get this number to zero,’ which is completely impossible,” she told BusinessWest. “People ask, ‘why is it impossible?’ Well, you have a very elderly population; you have a population that’s on a lot of serious medications that weaken your system.
“Not every patient is a 20- or 30-year-old marathon runner,” she added. “Some are overweight, some of them smoke, and they’re not as healthy as the marathon runner. A risk for me might not be a risk for you. Although there is standardization of procedures, we’re not all the same.”
Riley agrees that zero infections is an impossible goal to meet, but it’s still the goal.
“It shows the commitment of the hospital to do everything we can to make a safe environment for patients. The community really appreciates it,” she said. “The goal is zero infections. But no one is able to do that; it’s not just what we do, but the patient’s own immune system. No hospital has achieved zero, but we’re working as hard as we can, doing everything we possibly can, to create the safest environment for our patients, staff, and visitors.
“If we don’t aim high,” she added, “we’ll never get there. So we’re aiming for zero.”
Joseph Bednar can be reached at [email protected]

Karoun Charkoudian says people try yoga for a number of reasons, such as improving mental focus, easing back pain, improving athletic performance, or just feeling better.
“My personality is such that I need to be passionate about what I do, in every moment of every day. So I left, in search of the style of life where I could find that kind of passion,” she said.
Yoga was one of those things she felt passionate about, so she enrolled in advanced trainings and moved to Springfield, setting up a small studio in a building her father owned. “It was supposed to be a stopping-over point, not to stay. But I really fell in love with the city, and found out that there was very little yoga here. It was a good place to begin teaching.”
Three years later, she opened up a larger space in West Springfield, celebrating her one-year anniversary in the new location in January. “We have experienced tremendous growth since moving there,” Charkoudian said. “I really feel like it’s a beautiful yoga community; we are growing, and we have a beautiful staff. I feel so lucky to be a part of this.”
It turns out she’s not the only one searching for fulfillment through yoga. In fact, her years in business have coincided with a remarkable growth curve for what is now a $10.3 billion industry in the U.S.
Yoga Journal, which publishes a periodic “Yoga in America” study, reports that 20.4 million Americans practiced yoga in 2012 — a 29% increase from the 15.8 million participating in 2008. And it’s big business; that $10.3 billion spent on yoga classes and products in 2012 — including equipment, clothing, vacations, and media — is an 87% increase from $5.7 billion in 2008.
There seems to be more room for growth, too, as 44.4% of non-practitioners polled in the study said they are interested in trying it.
“The number of practitioners and the amount they spend has increased dramatically in the last four years,” said Bill Harper, publisher of Yoga Journal. “Companies that want to advertise to the health-and-fitness market for women will want to make sure that yoga is a strong segment in their target.”
That’s true; women are an overwhelming majority in the yoga world, representing 82.2% of the total market.
“Certainly, throughout the yoga industry, I think everyone would like to see more men in those classes, and there’s no reason not to,” Harper told the Coast News in California recently. “I think we know the reasons. They’re intimidated; they’re not as flexible is probably the number-one comment that I hear.”
What’s Stopping Them?
Helen Arnold has heard the excuses, too — but has also seen skeptics change their tune after trying yoga.
As director of Community Benefits and the Oncology Unit at Holyoke Medical Center, she said yoga is featured in support groups for cancer patients at HMC.
“When you do yoga, there’s the physical part, but mentally, it quiets your mind, and that’s really good for somebody who has any stress, anxiety, or depression,” she said, noting its benefit to individuals on a cancer journey.
“A lot of people feel with yoga that you have to be really in shape. But that doesn’t matter because there are different levels,” she said, adding that patients weakened by some condition or other find benefits from yoga. “It really does a lot for anyone with back pain, hypertension, cancer, epilepsy, menopause — those are probably the biggest things.”
Charkoudian said people try yoga for a number of reasons: to improve mental focus, to get calm and relaxed, to ease back pain, to improve athletic or work performance, to lower blood pressure, or just to feel better. But all have to overcome their preconceptions about the discipline.
“People tend to have really strong opinions about yoga, based on what they see in the media or on one class that they took in a style or with an instructor that may not have suited them,” she told BusinessWest. “People think that, because they’re stiff, they can’t do yoga, when that’s exactly why they should be doing yoga. Or because they can’t balance, they think they can’t do yoga. The point is to do yoga to have more flexible and supple muscles, better balance, and better focus — not to start that way, but to work toward that end. That’s why we call it a practice.”
 That practice encompasses a broad variety of styles. For example, Charkoudian offers different skill levels of Hatha yoga, which emphasizes basic strengthening, stretching, and breathing exercises, with a little bit of meditation, but also yoga based on the Vinsaya tradition, with a faster pace and an almost dance-like flow.
That practice encompasses a broad variety of styles. For example, Charkoudian offers different skill levels of Hatha yoga, which emphasizes basic strengthening, stretching, and breathing exercises, with a little bit of meditation, but also yoga based on the Vinsaya tradition, with a faster pace and an almost dance-like flow.
Other styles taught throughout the area include Anusara, a rigorous workout for the body and mind; Ashtanga, which is physically demanding and, like Vinsaya, links every movement to a breath; Bikram, a sequenced, sweat-inducing series of 26 poses, and a very popular option; hot yoga, which is similar to Bikram and performed in a heated room; Iyengar, a meticulous style that emphasizes the proper alignment in a pose and is good for people with an injury or chronic condition; and restorative yoga, which uses objects to prop students in passive poses so the body can experience the benefits of a pose without exerting too much effort.
Then there’s ‘laughing yoga,’ which was introduced to HMC support groups by cosmetic surgeon Dr. Vinodray Shaw.
“He came to our support group for an hour and a half and led the laughing yoga,” Arnold said. “Laughing yoga not only strengthens the mind, but aligns the body. How it aligns the body is, when you take a deep breath and laugh, it opens your lungs and affects every organ in the body.”
Practitioners of laughing yoga initiate laughter as a group exercise, and it typically turns into genuine, contagious laughter. The combination of deep breathing exercises from yoga and laughter exercises, which oxygenate the body and brain, makes participants feel more healthy and energetic.
“It affects the body, mind, and organs, and increases blood flow, which then increases mental alertness,” she said. “Just saying the word, ‘laughing yoga,’ we really had to pull people in. But after two hours, when we had to go, people were saying, ‘when is the next one?’ Really, the whole mood of the room changed.”
Learning Curve
People are now aware of what laughing yoga is and are looking forward to their next opportunity, Arnold said, but that seems to be true of yoga in general on a national scale.
“I found in our support groups that people thought they had to be fit, couldn’t be overweight, really had to be able to move, touch their toes,” she said, emphasizing again that, on the contrary, yoga is an ideal way for people to get fit or recover from injury, all while stretching their mind.
“It’s really good for patients with dementia, people who are losing some of their cognitive abilities, because it increases the blood flow to the brain,” she added. “Yoga really is body and mind together. I think it’s phenomenal.”
According to the Yoga Journal survey, the top five reasons people gave for starting yoga were improved flexibility (78.3%), general conditioning (62.2%), stress relief (59.6%), a boost in overall health (58.5%), and physical fitness (55.1%).
And many of them are just discovering those benefits. Of the survey respondents, 38.4% have practiced yoga for one year or less, while 28.9% have been at it between one and three years. A full 44.8% still consider themselves beginners, while only 15.6% say they’re expert or advanced.
That recent surge in new participants suits Charkoudian just fine. “Our new slogan is ‘step out of your box and onto your mat.’ It’s a challenge for people to step out of their daily lives for an hour two or three times a week, and experience the sense of connection and awakening that yoga does for the mind-body-breath system, and how that translates into their lives.”
Despite a recent proliferation of studios, she feels like yoga is still relatively new to the area, and people are still discovering how it may help them.
“It takes a lot of energy to educate people that yoga is good for them even if they’re really stiff or out of shape,” she said. “A lot of energy goes into that here, whereas, in other areas where yoga is more popular, people already know that yoga is great for them no matter what shape they are in.”
Arnold agrees that locals, even those who have been hospitalized, sidelined with injury, or stricken with cancer, are increasingly recognizing the benefits of yoga, from weight loss and strength building to a more positive mental focus. “It’s general health and wellness, yes, but the part many people don’t realize is that it’s not only for health promotion, but for peace of mind. That’s a really important piece.”
Charkoudian, for one, found peace of mind through yoga, but the road hasn’t always been a straight one.
“I went through a period of burnout about a year ago and did a lot of soul searching in terms of what it was that I wanted through teaching yoga, and who it was that I wanted to help,” she told BusinessWest. “And what I realized was this: when I was at ExxonMobil, I felt like so many people were asleep in their lives. These were regular, educated people making decent money. But it was like they handed their life over to some other entity and just went through the motions.
“What I hope to do with this studio is to help to awaken the people in the Greater Springfield area,” she continued. “We’re not looking to heal sick people. I feel like the worst epidemic isn’t sickness; it’s numbness — after all, people who are sick look to be healed, but people who are numb don’t even know there’s a problem. I want to help to awaken those people who have good lives, but maybe need a little boost, just something to bring more passion and vitality into their lives.”
Certainly, it’s not a stretch to see how the increasingly popular discipline of yoga can play a role in that quest.
Joseph Bednar can be reached at [email protected]
Dr. Andrew Lam’s twin passions for eye care and history have helped him carve out a unique niche in both fields.
That’s a passage off the book jacket of Two Sons of China, a novel penned by noted retinal surgeon Dr. Andrew Lam. The language is typical of that used by publishers to compel readers to turn some pages and buy the book, and it explains what this historical novel is all about.
But that excerpt doesn’t begin to convey the passion that Lam has for history, military history, World War II, and especially the usually forgotten theater of that global conflict — the war in China.
“I wrote this because I wanted more people to know what happened in China during World War II,” said Lam, who studied history as an undergraduate at Yale but was ultimately swayed to enter the medical field by the seemingly countless stories of the life-saving exploits of his father, a cardiologist (more on those later). “A lot of people don’t know that thousands of Americans served in China during the war and that millions of Chinese died; China actually served a very important role in the Allied victory, yet few seem to know the story.”
Telling it, or at least part of it, through this saga based on true events has become the latest chapter in an intriguing and newsmaking career, one that has put Lam’s name together in the same sentence with the phrases ‘distinguished ophthalmologist’ and ‘bestselling and award-winning author.’
Dr. Andrew Lam’s first published book blends the history of eye-care innovations with his own personal experiences, while his latest work explores the often-forgotten Chinese theater of World War II.
And they’re told with heavy use of the first person, which gives such weighty subjects and 15-letter words a needed personal touch.
“I told my agent I wanted to write a book about the heroes of ophthalmology,” he recalled. “And she said, ‘that’s fine, but nobody’s ever going to buy that book, because only nerdy ophthalmologists would buy a book about medical non-fiction like this.’ So I decided I had to do something to make it more marketable, to make it more interesting, to make people want to pick up a book about medical history.”
That something turned out to be his decision to blend his own experiences training in surgery, a tactic that helped the book, which came out nearly a year ago, greatly exceed his publisher’s expectations, become a bestseller on Amazon, and earn awards from the London Book Festival and the New England Book Festival, with more competitions to come.
Two Sons of China was actually finished before Saving Sight, but it took Lam’s agent more time to find a publisher for that work. The novel was released in December, and early sales have been promising.
Meanwhile, Lam is hard at work on his next project, a detailed look at the famous 442nd Regimental Combat Team — the unit of Japanese-American soldiers that fought in Europe during World War II while many of their families were held in internment camps in the U.S.
For this issue, BusinessWest talked at length with Lam about his twin passions, and how they both might be considered volume businesses.
Novel Ideas
The lobby at New England Retina Consultants looks like most other medical waiting rooms, with rows of seats, assorted magazines on a table near the front, and staff members taking information and calling out patients’ names.
What sets it apart are all the framed newspaper clippings about Lam and his books and signs alerting visitors that signed copies of these works are available for purchase.
The juxtaposition of these items speaks to how effectively Lam has been able to blend his passions for medicine and history rather than choose one over the other.
How he’s managed to do that is an intriguing story, one that begins in Springfield, Ill., where Lam grew up and received almost daily reminders about how respected, and revered, his father was in that community, famous as the birthplace of Abraham Lincoln.
“I’d go to the mall or just walk around the city, and people would stop me and say, ‘your dad’s a great doctor; he saved my life or the life of a loved one — are you going to be a great doctor like your dad?’” he recalled. “These kinds of experiences left an indelible mark on me; they showed me that being a physician could be a very gratifying thing. He had a very gratifying career, and you can’t help but be influenced by that when you’re growing up.”
So strong was that influence that Lam put aside any thought of doing graduate work in history and instead went to the University of Pennsylvania Medical School, where he quickly focused on surgery, which fit his personality — “I like to fix things; I like to do things and see if I can make things better” — and the eye.
“I felt that sight is so important to everybody, so ophthalmology was the perfect fit,” he said, adding that, 10 years after graduating from Yale, he completed a fellowship at the prestigious Wills Eye Hospital in Philadelphia and then joined New England Retina Consultants in Springfield, where he saves patients’ sight on a daily basis.
He treats a number of conditions, including retinal detachment, macular degeneration, and diabetic retinopathy, and told BusinessWest that the work is extremely rewarding because of the seriousness of those problems and the ability to greatly improve quality of life by providing solutions.
“The people I treat have serious eye problems — if other eye doctors have a complication, they will often call on us to help them,” he said. “But the flip side to this is that it’s very gratifying to try to help people, because we’re talking about their vision.”
But while Lam was certainly excelling in his chosen field, his passion for military history — and, more specifically, U.S. involvement in Asia during various 20th-century conflicts — never left him, and he began looking for ways to express it. He found one in his desire to relate a little-known chapter from the forgotten Chinese theater of World War II — an operation known as the Dixie Mission.
This was the first effort on the part of the U.S. to establish official relations with the Communist party of China and the People’s Liberation Army, led by Mao Zedong, which was then headquartered in the mountainous city of Yenan.
“During the war, Americans supported Chiang Kai-Shek’s nationalist government in Chungking,” he explained while turning to a map in his book. “But he wasn’t the best ally because his government was very corrupt and inept, and they weren’t really interested in fighting the Japanese — they wanted to hoard American weapons so they could use them in the future civil war with the Communists.
“So the Americans were very frustrated because they wanted to fight the Japanese,” he went on. “They later learned about another group of Chinese in the north in Yenan. It turned out that these were Mao’s Communists, and at this point we had no idea they would be the future leaders of China; these were just agrarian reformers who were also fighting the Japanese even though they hated the Nationalists, and there was basically a separation.”
The name Dixie Mission stemmed from how Americans viewed the Communists as rebels, not unlike Southerners during America’s Civil War, said Lam, adding that U.S. forces joined the Communist guerrillas on a mission behind Japanese lines. Accounts of this mission provided inspiration for the book, but Lam chose fiction to make the subject more entertaining for the reader.
“My goal is help people learn about the war in China,” he explained, “but I thought personally that it would be fun to write an exciting, action-packed, emotional war novel that would entertain people.”
The Latest Word
While his agent was shopping Two Sons of China, Lam shifted his focus — both literally and figuratively — to a different kind of hero: pioneers in eye care.
He said Saving Sight was inspired by the groundbreaking developments in ophthalmology and a desire to retrace some of the steps that laid the groundwork for these advances.
“We can take out cataracts in minutes, we can do Lasik surgery, which yields instant, glasses-free 20/20 vision, and we’re even starting to implant retinal microchips that can return some sight to the blind — it’s FDA-approved, but we haven’t started doing it yet,” he explained. “These are amazing things that we do, and I started thinking, ‘how did all this come about — who invented them?’
“What I learned were these stories of the heroes of my field,” he continued. “And these are incredible stories — they have the components of a Hollywood movie; there’s perseverance, serendipity … a lot of these people were ridiculed for their ideas for decades before they came into acceptance. I knew I wanted to write a book that shared all that.”
And Saving Sight is something quite unique in literature, he went on, adding that no one in the profession had written a memoir on what it’s like to be an eye surgeon, and it’s clear from the first year’s sales volume that the market was ready for one.
But as he tapped on the cover of Two Sons of China, Lam noted that fiction in general, and even historical fiction, is something much different.
“There’s a lot of competition in fiction,” he said, adding that, to stand out, a work of historical fiction must both inform and entertain. He believes Two Sons of China achieves that mission, and that his latest project involving the 442nd, called Repentance, will follow suit.
“Asian Americans know about the 442nd; it’s famous for us,” he told BusinessWest. “But not enough Americans know about it. This is the most decorated unit in U.S. military history — they won more than 20 Medals of Honor.”
As he continued to talk about the 442nd, the war, and the contributions of countries such as China and Russia, Lam’s passion for the subject came through loud and clear. And it is that passion that drives him to write — and find the time to do it.
“My goal is basically to inspire people,” he said. “I hope Saving Sight inspires young people, and I hope Two Sons of China helps people understand the history of World War II more, and you only do it because you’re passionate about it — it’s too much work otherwise.”
He said people are always asking where he finds the time for his writing, and admits that he has no profound answer for them other than to say that, if one is passionate about something — and he is when it comes to both science and history — then he or she finds the time.
“I have a great wife who supports me,” he noted. “I write whenever I can, like if I’m driving my kids and waiting for them after gymnastics, or if I’m waiting poolside at my son’s swim meets. There was a time when I’d watch a movie every night, but that was a major time suck, and I stopped doing that; now I use that time to write.”
Epilogue
Speaking of films, Lam said his agent is already having discussions with at least two parties interested in the movie rights to Two Sons of China.
Those talks are still in the preliminary stages, and he considers it unlikely that the story will be coming to the big screen anytime soon, although he’s staying optimistic.
“It’s a long shot, always, but there is interest,” he told BusinessWest, adding that he’s not sure how that story will end.
He is sure that he will have more stories to share. That’s because his passion for history is deep, and while it’s not his career, it’s a big part of his life, and it always will be.
George O’Brien can be reached at [email protected]

Dr. Richard Wood says American consumers are essentially guinea pigs for GMO foods, since no one really knows what their long-term health impact will be.
“I will say, ‘how many of you know somebody with a food allergy?’ I’ve done this for years, and every time, every single hand goes up,” said Wood, assistant professor of Exercise Science at Springfield College. “Then I say, ‘when you go home tonight, call or text your parents and ask them the same question about when they were in school. What do you think the answer will be?”
It’s a question worth pondering; doctors have indeed grappled with a surge of food allergies in the past 20 to 30 years. Some cite the ‘hygiene hypothesis,’ the idea that kids today stay too clean, too sanitized, and aren’t exposed to enough germs to keep their immune system busy, causing that system to turn on itself in the form of allergies.
But others are taking a critical look at what we eat today, from heavily processed, chemical-laden junk food to the proliferation of foods containing genetically modified organisms, or GMOs. Introduced to the commercial market about two decades ago, GMO foods are estimated to be present in some 80% of the items in the average grocery store.
“These have been around for 20 years, and no overt medical problems have been caused by them. But some people are concerned there are more subtle issues going on,” Wood said — like that startling rise in food allergies. But no one, it seems, knows for sure.
“It’s incredibly difficult to trace [an allergy] back to the GMO because we haven’t tracked it,” he went on. “People don’t necessarily know how much GMO product they’ve eaten and when they’ve eaten it, so if someone develops a food allergy, it’s really tough to say it’s caused by that.”
Genetically modified foods are produced from organisms that have had changes introduced into their DNA through genetic engineering — techniques that have allowed for the introduction of new crop traits as well as greater control over a food’s genetic structure.
The commercial sale of GMO food began in 1994, when Calgene introduced its Flavr Savr delayed-ripening tomato, which was genetically modified to slow the ripening process after picking. Since then, genetic modification has focused primarily on cash crops in high demand by farmers. As of last year, roughly 85% of corn, 91% of soybeans, and 88% of cotton produced in the U.S. are genetically modified.
Considering how many products contain corn and soybeans alone, it’s not difficult to comprehend the reach of GMO food.
“The only way to get food that does not have GMOs is to buy certified organic food,” said Eric Decker, who chairs the Department of Food Science at UMass Amherst. “Almost all soybean and corn is GMO, and a lot of byproducts come from those; it’s really hard to find non-GMO food. Also, all livestock is fed GMO, too.”
Another early GMO food is known as the Roundup Ready Soybean, which was designed to be resistant to herbicides (like the commonly used Roundup brand). “Roundup kills everything, so they genetically altered the soybean so it would not be susceptible to Roundup,” Decker said. “Farmers could use Roundup to kill everything on the field, then plant soybeans with no danger.”

Eric Decker says GMO foods have repeatedly proven to be safe, but he understands the qualms many people have over their potential health, environmental, and economic impact.
Margaret Smith, a plant breeder at Cornell University, acknowledged in an interview with grist.org that many concerns exist, but she remains confident in the potential benefits of GMO technology.
“I think we need to be thoughtful, and as we learn more, we need to continue to think about this carefully,” she said. “My message on this is that we shouldn’t just stop because there are unknowns. Every technology has unknowns. We just have to be as thoughtful as we can.”
Gut Check
Wood recently became director of Springfield College’s Center for Wellness Education and Research, and he’s long had a keen interest in the broad topic of what people eat and where their food comes from.
When discussing the potential effect of genetically modified food, he begins by discussing what’s known as the human microbiome.
“We have trillions of bacteria that live in our intestinal tract, and they all have their own genome — what makes up their genetic code — and we as people have the same thing,” he explained. “You take all these types of genomes interacting with each other, and there’s an ideal level at which they interact. What we’re starting to see, possibly, is that some of these GMO products are causing different interactions than what existed before. That’s where it’s getting interesting.”
Decker stressed that genetically modified organisms have never proven to be unsafe, although the potential is always there. “The DNA is different, but we don’t absorb the DNA; it’s all broken down in our gut. We don’t absorb it. So the risk to a human is pretty minimal.”
He puts more stock on risk to the environment, because as the modified genes spread, the agricultural world could end up with less diversity. Also, “there’s a lot of criticism in the farming model; even if the farmer next door doesn’t want to grow GMO, eventually he’ll see GMO genes in his crop as well.” Wood added that many anti-GMO advocates are concerned about the long-term impact of GMO agriculture on soil quality, cross-contamination, wildlife, and water sources.
The economic model has come in for criticism as well. Decker said Monsanto makes farmers sign a contract committing to buying new seed every year, where, in the past, farmers would hold over some of their crop every year to reseed from it. “That’s how Monsanto makes money — it sells them something every year. Even with all that, it’s still economically favorable for farmers to buy these seeds.”
Proponents say GMO crops offer the potential for greater yields, which could be a significant benefit for a planet whose population is constantly rising.
“The debate over genetically modified crops and food has been contaminated by political and aesthetic prejudices: hostility to U.S. corporations, fear of big science, and romanticism about local, organic production,” argues Paul Collier, professor of Economics at Oxford University, in the New York Times. “Refusing genetic modification makes a difficult problem more daunting. Food supply is too important to be the plaything of these prejudices. If there is not enough food, we know who will go hungry.”
As director of the Center for the Study of African Economies, he knows something about this issue.
“As Africa’s climate deteriorates, it will need to accelerate crop adaptation,” Collier notes. “As population grows, it will need to raise yields. Genetic modification offers both faster crop adaptation and a biological, rather than chemical, approach to yield increases. Opponents talk darkly of risks, but provide no scientific basis for their amorphous expressions of concern. Meanwhile, the true risks are mounting.”
In the same article, however, Vandana Shiva — founder of Navdanya, a movement of 500,000 seed keepers and organic farmers in India — rejects the idea that GMO crops are the best solution to overpopulation and drought.
“We need biodiversity intensification that works with nature’s nutrient and water cycles, not against them. Genetic engineering has not increased yields,” she notes, citing research by the Union of Concerned Scientists. “The study did not find significantly increased yields from crops engineered for herbicide tolerance or crops engineered to be insect-resistant.
“The International Assessment of Agricultural Science and Technology for Development carried out by 400 scientists over four years has also concluded that genetic engineering does not hold much promise,” she adds. “Instead, small farms based on principles of agri-ecology and sustainability produce more food.”
Meanwhile, the Non-GMO Project, which argues against genetically modified foods, emphasizes that most developed nations do not consider GMOs to be safe, and that, in more than 60 countries around the world — including Australia, Japan, and the entire European Union — there are significant restrictions or outright bans on the production and sale of GMOs.
“There’s a lot of hysteria out there, but in Europe it’s even worse,” Decker told BusinessWest, noting that GMO seed producers such as Monsanto and DuPont have been rebuffed by the European Union so often that they’ve stopped submitting products for approval there.
“But I think GMOs are here to stay,” he added. “Next-generation GMOs may offer greater yields and drought resistance, so you can plant in areas where you can’t plant crops now. And there are some good statistics saying pesticides are being taken out of the environment with GMOs.”
Pros and Cons
Wood acknowledged that many of the scientists behind GMO technology are acting with the world’s good in mind.
“We’ve been eating GMO products for 20 years, and I don’t think anyone ever intended negative consequences,” he said. “I think what we have are innovative folks trying to solve some real problems, and along with the solutions come some consequences. But the issue is, we don’t really know about some of those consequences yet. As I say in class, we’re kind of all human guinea pigs in this experiment.”
For example, “if climate change is a real thing, and let’s say more droughts are in front of us, what if a scientist can create a seed for crops that can resist drought? If climate change is a real problem that needs facing, that scientist has done a lot to help us. On the other hand, when you manipulate what that seed would normally do, you are manipulating the chemical composition of what’s going into the body, and that has a direct interaction with the human microbiome.”
One major issue for people concerned about GMO foods is clearer labeling of products in supermarkets. They are encouraged on that front by recent legislative developments, such as the decision of U.S. lawmakers last September not to renew a provision of agricultural law known colloquially as the ‘Monsanto protection act,’ which protected seed producers from liability if their products are found to be harmful.
“Labeling of this has become the new big issue,” Wood said, before asking rhetorically why Monsanto and others are spending so much money to prevent people from knowing what’s in their food. “They’d probably say they’re protecting their intellectual property, but I don’t know.”
Nathaniel Johnson, the grist.org writer who interviewed the Cornell plant breeder, takes a balanced approach to the GMO controversy.
“Those of us who are suspicious of genetically engineered foods need to be thoughtful, too,” he writes. “I still think that we have an important role to play in making sure the technology isn’t used inappropriately. But it’s not useful to flail blindly against something we don’t understand.”
Wood takes the same thoughtful approach. “It’s more about us being aware of what’s going on,” he told BusinessWest. “The way I look at it, these aren’t intended consequences. And if they exist, scientists aren’t looking to cause problems; they’re trying to solve them.”
But those good intentions do nothing to minimize the concerns he has with what Americans are — unknowingly, in many cases — sending into their collective gut.
“If you eat like crap now, it’s not like eating like crap 20 or 30 years ago,” he said. “People say, ‘I ate junk as a kid; it’s no different.’ But it’s not the same crap. The stuff it’s made up of is not the same.”
Joseph Bednar can be reached at [email protected]

Dr. Kevin Hinchey says a shortage of primary-care doctors is partly driven by a gap in pay and prestige compared to many specialists — but those factors may be improving.
Crisis Management
Hinchey said the issues of pay and professional respect in the primary-care world have improved slightly, but the problem of shortages extends into other areas as well.
“There has been an acknowledgement from all quarters that there will be a doctor shortage, so the medical schools have been asked to increase the size of their classes, and that has happened,” he said. “The problem is, after graduating from medical school, the training slots have not increased.”
As a result, he said, over the next three to five years, the international graduates who train in the U.S. and set up practices here, many in underserved areas, won’t stay here because they’ll be pushed out by U.S. graduates, and that displacement will do nothing to solve the doctor shortage. Meanwhile, the federal government has been decreasing funding for medical education.
“We seem to do better in crisis management, unfortunately,” Hinchey said, “so when this gets close to a crisis, I think it will be better addressed.”
A doctor shortage — at a time when Americans are living longer and more of them are receiving insurance coverage — could have several effects, writes Dr. Ronald Dunlap, president of the Mass. Medical Society, on the MMS blog.
One is a rise in retail clinics, many run by nurse practitioners (NPs), which are expanding beyond basic services into activities like lab services and managing chronic diseases.
“Research shows that patients like the convenience of retail clinics, particularly when they have difficulty getting to their primary-care provider,” Dunlap notes. “Given the limited resources and no on-site physicians, most patients may not regard them, at least for now, as a place for primary care. As they add more sites, services, alliances, and advertising, however, they are likely to play a bigger role in healthcare.”
However the idea that NPs can fill the physician gap falls short, because nursing shortages exist, too. A large percentage of nurses are expected to age out of the workforce soon, and nursing schools are having trouble recruiting faculty to train a new generation.
“Further, with an emphasis on cost containment, replacing high-salaried providers (physicians) with lower ones (NPs) with less training will likely not result in savings,” Dunlap argues. “We have seen that less-experienced providers tend to order more tests and procedures, raising costs. Cost control will result best from the team approach of coordinating care and avoiding unnecessary referrals, testing, and procedures.”
He added that a rise in NPs, who tend to work in urban settings, won’t ease the shortfall in rural environments and other underserved areas. Doctors also tend to flock to cities, Hinchey noted, but he said telemedicine might become a significant part of the solution in the coming decade.
“There is some of this telemedicine going on now. But what if you could actually Skype your doctor? He or she gets a look at you, gets your blood pressure through a USB port, gets some other data from you. You don’t have to go to the office when you feel miserable,” he told BusinessWest. “Is that technology coming? I think yes. And I think that would be a a benefit, and a lot of patients would like that. That could increase capacity. And if I’m sick and I want to be seen, I could be seen.
“For some aspects of what we do, the laying on of hands will never be replaced,” he continued, referring to trips to the doctor’s office. “For many issues, from an urgent-care perspective, I’m going to want to be seen. But I just think we can be a lot more creative about this.”
To Your Health
Much of that creativity will come on the preventive-health side, Ostrowski said, which is why Health New England has long promoted wellness initiatives in the workplace.
“Most people consume most of their calories at work, during the work day,” she told BusinessWest. They get to work and get coffee or breakfast, then a mid-morning treat, they eat lunch at their desk, then have a mid-afternoon snack. For many people, work is also the time when they’re the least active because they’re at a computer at their desk or sitting at the conference-room table.
“So we believe the workplace has a really unique position in assisting with creating healthy employees and families, and employers have a unique interest in that because they’re bearing the burden of healthcare costs for that population in many ways — they pay for insurance for employees and families, and they also lose productivity to sickness or disability. So it’s extremely important to have a culture of health, so to speak, and engage people throughout the day in healthy behavior and healthy activities.”
Through its Healthy Directions program, Health New England engages with companies through an assessment process, including health screenings and lifestyle-focused interviews, then helps employees set goals for healthier habits. “We’re concerned with small steps, not everything at one time. Most people won’t be a success if they try to do it all.”
For instance, HNE promotes a graduated ‘jump start’ concept to better health; participants are encouraged to increase their water intake the first week, walk 10,000 steps a day the second week, eat five servings of fruits and vegetables per day for the third week, then bring it all together in week four.
“It’s reinforcing healthy lifestyle habits, and hopefully some of it will stick,” Ostrowski said. “You spend eight hours of each day at work, so if you have a supportive health culture in the workplace, odds are your health will improve. That’s really the basis our program.”
A parallel trend in health insurance, she said, is a shift toward high-deductible health plans, which tend to work best for people who take preventive wellness seriously. “The healthier you are, the more appealing that is, because there’s less out-of-pocket expense from the monthly premium. If you couple that with health savings accounts, it’s a great benefit. But if you’re not healthy, that’s a difficult plan to manage.”
The full impact of the Affordable Care Act on the medical and insurance landscape has yet to be felt, but Hinchey expects changes in the way providers are paid as it relates to the ‘medical home’ concept, also known as accountable care, by which a team of providers — doctors, nurses, specialists, therapists, etc. — share in the treatment of a patient and also share in the reimbursement.
“People are starting to think in terms of a medical home,” he said. “What if I had a nutritionist? I don’t have diabetes or high blood pressure, but I’m a little bit overweight; can I talk to a nutritionist about it? Or maybe someone for exercise, or other things that could help me be a little bit healthier, that are not presently covered by insurance.”
Dunlap maintains that physician satisfaction with the profession — not necessarily the administrative stresses — remains high, especially as they grow comfortable with such innovations. “More physicians are becoming familiar with reform initiatives, such as global payments and accountable-care organizations, and more physicians indicated they are likely to move to global payments to reduce healthcare costs.”
Bridging the Gap
Hinchey said there’s a long way to go to rectify the conflict between cost and access, but it might take a “quasi-crisis” or two to really move the needle.
“We have to be creative to meet these needs,” he said, referring again to the promise of telemedicine versus the barriers posed by the current reimbursement structure. “I can Skype at people if I want to, or spend 100% of my time talking to people on the phone, but if I only got paid for when they come into my office, I wouldn’t last very long.
“But as payment reform starts to come around,” he added, “it will cause kind of a domino effect. None of these things happen in isolation.”
Clearly, the future is still being written.
Joseph Bednar can be reached at [email protected]
Sharon Adams says the professionals who staff the ‘hub’ are specially trained to monitor and enhance the efficiency of the patient experience.
Hub of Progress
The human element is as critical to Care Connect as the technology. When someone is admitted to Mercy, a C3 works directly with physicians and other providers to track the patient’s progress, plan a schedule of tests and procedures, and come up with an expected discharge time.
The focus is on using time wisely, Adams said. For example, the C3s use details such as when the patient is being transported or when rooms are being cleaned to arrange tests and other care around his or her schedule.
“We’re trying to eliminate the ‘white space’ in the patient stay, when people are waiting for things to happen,” Moen added. “That’s not useful for the patient, and it’s not good for us to be less efficient than we should be. So this was really a unifying point — what can we do to make this better? And having it all coordinated from this hub is important.”
Last spring, in preparation for bringing the Care Connect system online, more than 1,500 employees in dozens of departments were trained on using the new software to coordinate with the C3s.
As for the coordinators, “they were specially trained for eight weeks, full-time, in this patient-flow system and documentation,” Moen said. “The hub is open 24 hours a day, seven days a week. It used to be that things slowed down on weekends; we’re trying to make sure we’re an efficient operation seven days a week, to get patients the services they need all the time.”
Mercy also implemented a program called ‘operational rounding’ every Wednesday, where members of the SPHS senior leadership team join front-line providers in patient-care areas. From their observations, they work together to find ways to improve efficiency and quality of care.
“We’ve made more than 75 specific improvements in patient flow, many impacting quality, such as reducing falls and pressure ulcers and hospital-acquired infections,” Moen explained. “Again, it’s about having an understanding of where we are and where we’re trying to go. This has really been a transformational project for us, and we couldn’t be happier with the results at this point.”
As impressive as the patient-management technology is, Adams added, it doesn’t operate in a vacuum. “We’ve spent years working through what the current processes are, in every department, every place the patient touches. We went through 47 or 50 departments, working with them to ask, ‘this is what we currently do; what can we do in the future? What’s the best thing for patients?’ We’re no longer saying, ‘what’s best for our own schedules?’ It’s all patient-focused.”
It’s also a metrics-driven program, Moen said, and all that data is fed directly to the hub. “We’re taking a lot of different milestones, and we can see where the delays are in the process. This gives us sort of a dashboard to see where we can improve further and document where we’ve gotten better.”
Adams stressed that the C3s have a supervisory role in patient care, and they’re trained to be experts in care coordination. “They understand the resources in the community, what insurance will pay for, and they update the insurance company about why the patient needs to stay longer.”
Documentation is critical. “Clinical documentation supports why that patient should be an inpatient, making sure we are capturing the severity of that patient’s diagnosis. That’s where they work very closely with physicians … saying, ‘you probably need to be documenting why the patient is more complex than we thought.’ They make sure we’re being reimbursed at the level of care we’re providing.
“The physicians feel it’s a very good resource,” she added. “They are pleased when the clinical-care coordinators say to them, ‘you just need to document this.’ They don’t see it as a threat; they see it as a great resource, reflecting all the hard work we’re doing for patients.”
Accountable to Patients
Hospital leaders across the U.S. understand they’re facing a new era of cost consciousness, driven by a growing, aging population, health reform that’s pushing more patients into the system, and the burden of new, expensive technology.
Accountable care is a model by which a team of providers — doctors, nurses, specialists, and therapists — are paid a certain amount to collectively treat a patient. The concept, which Mercy began to pioneer in Western Mass. almost a decade ago, stresses efficiencies like limiting unnecessary tests, but demands quality as well, because preventing rehospitalization is a key goal. Moen said Care Connect goes to the heart of that model.
“We’ve made great strides in all areas. We wanted to reduce length of stay and still make it a better patient experience,” he told BusinessWest. “And because we’re freeing up capacity on the inpatient side, the ER has become much more efficient; there are fewer situations where a patient is held in the ER, waiting for an inpatient bed.”
Mercy has made changes in the emergency area as well, getting patients to a physician or physician’s assistant quicker than before and fast-tracking less serious situations to clear capacity for patients who are more ill. “We’ve taken an hour off the door-to-door time for patients in the emergency room,” Moen said.
Care Connect has also aided the discharge process, he noted, as C3s help coordinate care beyond the hospital, whether it’s skilled nursing, home care, or simply setting up primary-care appointments and following up — all with the goal of preventing readmissions.
“We want to bring these concepts out to providers in other parts of the system, particularly behavioral health at Providence in Holyoke,” he said. “People are working as a team, less silo-based. It’s a much more planned process. It helps us be more efficient and minimize wasted motion, and it frees up staff to spend as much time as possible with patients.”
Adams said the effort has spawned nothing short of a culture change. “Providers and staff have more time to communicate together, as a team, like physicians years ago. That’s what patients loved, seeing a nurse and provider sitting with them, talking.”
The process also helps reduce anxiety for patients and families, she said, by sharing as much information as possible about what tests, procedures, and treatments are coming up, and when.
“Now we’re all on the same page. Patients are already feeling vulnerable, but now they have more control over their own schedule. We can tell them exactly what time the CT scan is, rather than saying, ‘oh, just wait for the phone call.’”
The hub has also helped C3s and other providers identify backlogs in the system in real time, which makes it easier to prevent them. “In the past, some of this data wouldn’t be available until weeks later, making it difficult to recreate what happened,” Adams explained. “The idea is to get you out safely with good care, and not keep you here any longer than you’d like or we’d like.”
More information — for patients during their stay, and for hospital leaders — is a constant goal, Moen said.
“Especially for patients with no working knowledge of the healthcare system, this gives them a better idea about their condition, and we can take some of the anxiety out of the situation patients find themselves in,” he told BusinessWest. “If we can do that, it’s a major accomplishment. We want to be a navigator for them, along with their primary-care doctor.”
Ahead of the Curve
As he showed BusinessWest around the hub on the hospital’s third floor, Moen called Care Connect “a very important subset of the whole ACO process, where we’re getting patients to the right level of care as soon as possible, and helping them stay well despite the chronic conditions they may have.”
But he admitted Mercy still has much to do — namely, make its zero-defect philosophy a reality through this renewed emphasis on efficient, coordinated care.
“If we’re perfect 99% of the time, that means 1% of patients didn’t get the care they deserve, and that’s not acceptable,” he said. “It’s not easy — medical care is very complicated, and patients are very individualized.”
But modern healthcare is only going to become more complicated, and health systems that have not moved accountable care from a conceptual buzzword to reality — as Mercy has done with Care Connect — will be at a distinct disadvantage in a challenging future.
“A lot of hospitals will have trouble catching up,” Moen said. “We didn’t want to be in that position. We always want to be out ahead of the changes.”
Joseph Bednar can be reached at [email protected]
Dr. Stephen O’Connor says there must be a “healthy balance between diagnosis with imaging and more traditional means of diagnosis — and it has to be driven by evidence-based medicine.”
Film Reviews
Louis Pacilio looks to a future where diagnostic testing involves no stressful false positives, but only detection of diseases that may grow and become life-threatening.
Value Proposition
O’Connor told BusinessWest that the speed and accuracy of imaging has markedly improved in recent years, especially in emergency medicine. But, because of the cost, he said, “there’s got to be a healthy balance between diagnosis with imaging and more traditional means of diagnosis — and it has to be driven by evidence-based medicine.”
According to the Journal of the American Medical Assoc., evidence-based medicine integrates the best available evidence with clinical experience, allowing clinicians to recommend, and their patients to make, informed choices consistent with their values.
“Just because it’s a fancy new tool and it’s more expensive, should we be using it?” O’Connor asked. “The question is, are we adding value with the newer technology? Clearly, over time, CT scan has earned its spot.”
On the other hand, O’Connor is currently working in partnership with pediatric surgeons to develop an MRI (magnetic resonance imaging) urology program, replacing IVP, but the cost effectiveness has not yet proven to be acceptable for the Baystate practice.
Imaging technology has seen its share of advancements, he continued, and part of what drives the adoption of new breakthroughs is the habits of other physicians.
The newer, more advanced machines that physicians have found worthy boast two highly sought-after factors: less radiation use and more accurate results.
One advance is the colonization of the radiation beam itself, which offers a more finite, less fuzzy beam with less scattering of radiation to other areas of the body. Another is radiation dose-monitoring software called iterative tracking, which permits high-quality image reconstruction that eliminates the graininess typically caused by a lower radiation flow.
O’Conner compared that to a picture taken in a room with low light that offers poor image contrast. The newer imaging software is able to increase the contrast to improve image quality for a more precise detection of disease.
In the diagnosis of osteoporosis — a bone disorder resulting in diminished bone strength that predisposes a patient to increased risk fracture — Lori Stoudenmire, a certified bone-density technician at Women’s Health Associates in Westfield, deploys one of the most advanced forms of bone densitometry imaging in the region, using a GE Lunar scanner with a software program called FRAX.
The computer algorithm, which stands for ‘fracture risk assessment index,’ analyzes a patient’s important historical variables — genetics, lifestyle, trauma — alongside a full-body bone scan to calculate the 10-year probability of hip fracture or major osteoporotic fracture of the spine, forearm, hip, or shoulder. Dr. Robert Wool, physician and owner of Women’s Health Associates, bases patient treatment on that scan.
“We used to treat solely on bone density, but we know that fracture risk is not based solely on bone density; there are lots of other factors,” said Stoudenmire. Capturing those other variables is what has made the advancement of FRAX so significant for bone-density imaging. Screening every two years allows for bone-loss comparisons, she added, and further developments are on the way.
“The programs, which are meant for more elder patients, are changing now to open up to men who are showing early signs of osteoporosis, or cancer patients who are maybe in their 30s who are on chemo, because that will affect your bones,” she noted, adding that oncologists can now monitor cancer patients and properly medicate them for severe bone loss.
Stoudenmire feels that the imaging is very clear with the GE Lunar, but she would like to see more advancements in FRAX — specifically, questions that go beyond history and involve more lifestyle elements, giving doctors even more information about true bone health as they craft an appropriate diagnosis.
Image Is Everything
In just the past few years, Pacilio has been pleased to see increased accuracy in diagnosis, in not only 3-D mammography, but advanced ultrasound and breast MRI. Yet, he looks to a future where testing for breast cancer, or any other disease, involves no stressful false positives, and advanced imaging can help him detect only diseases that threaten to grow and potentially become life-threatening.
Those advanced imaging modalities, including a hybrid imaging technique called image fusion; PET/CT, which is transforming cancer care; and PET/MRI, a potential advancement in oncology, cardiology, and neurology, are in various stages of research. Just two months ago, the U.S. Food and Drug Administration approved a radiopharmaceutical for use with PET to image the brains of adults being evaluated for Alzheimer’s disease and dementia.
At this stage, many of the promising image-fusion modalities are exclusive to elite research facilities, but over time, they, too, will be adopted by regional health systems.
With every one of those advances, doctors will produce speedier, more precise, and often less stressful results — and patients will have a clearer picture of their path to good health.
Elizabeth Taras can be reached at [email protected]
Click here to download the PDF
 The casino age may be underway in Massachusetts, causing some to worry that large, flashy gaming resorts will introduce the scourge of gambling addiction in the Bay State.
The casino age may be underway in Massachusetts, causing some to worry that large, flashy gaming resorts will introduce the scourge of gambling addiction in the Bay State.
Too late, says Dr. Baxter Chandler. Compulsive gambling is already a widespread problem.
“Massachusetts has one of the most successful lotteries in the world, and we have keno, and two large casinos within easy driving distance,” said Chandler, director of Behavioral Health Services at Holyoke Medical Center (HMC). “So problem gambling is not a new problem, but it is more recognized now as an issue.
“It’s a really tricky thing,” he continued. “A lot of people out there do scratch tickets or keno, and they don’t have the finances to do that. It’s easy to say, ‘Uncle John? All he does is scratch tickets.’ But if Uncle John is spending $400 a week on scratch tickets and only gets $600 in Social Security, then it’s a problem.”
But with the prospect of a casino resort in Springfield’s South End — the state’s Gaming Commission will choose one Western Mass. site for a casino early in 2014, and the $800 million MGM Springfield proposal is the only one on the table after voters in West Springfield and Palmer rejected casino bids — the issue of gambling addiction is certainly taking on a higher profile.
It’s timely, then, that the entire outpatient behavioral-health staffs of HMC and one of its affiliates, River Valley Counseling Center, recently earned the MA-PGS (Massachusetts Problem Gambling Specialist) certificate administered by the Mass. Council on Compulsive Gambling (MCCG).
Dr. Baxter Chandler says health professionals typically don’t consider gambling a vice in itself, but are concerned about its effect on people’s lives when it spins out of control.
Risk and Reward
Still, Chandler and Russell were quick to clarify that gambling addiction is no mere loss of control, but has physiological similarities to substance abuse.
“Many times, people, depending on their background, feel like it’s a control thing; they think they just don’t know how to control themselves,” Russell said. “But people don’t realize the effect that gambling has. They don’t realize that, when you gamble, it releases the same dopamine in the brain as if you did drugs — as if you did cocaine.”
Although a gambler isn’t actually putting a chemical into his body, Chandler added, “according to the brain studies they’ve done on compulsive gamblers, similar areas of the brain light up, as if someone is using a substance.”
Science author and blogger Steven Kotler breaks down some of this research in an article titled “High as Hell: the Evolution of Our Gambling Addiction.”
“Scientists long believed that dopamine was pure pleasure,” he notes. “It was thought of as the reward portion of the body’s need/reward system. You wanted something fundamental to survival — like a next meal or a sexual partner — and when you got that thing, the brain released a little dopamine, so the next time you were faced with a similar situation (like being hungry), you would remember that feeding yourself felt damn good.”
But Kotler cites the work of several scientists, including Greg Berns, associate professor of Psychiatry and Behavioral Sciences at Emory University, suggesting that dopamine is actually released not when one receives the desired reward, but when one takes the risk to do the thing that leads to the reward.
In other words, a gambler doesn’t have to win at slots to get the dopamine ‘hit’; simply pulling the lever will do that. “And associating risk with reward is a gambler’s bread and butter,” Kotler writes.
The initial consequences of compulsive gambling are different than substance abuse, in that they’re largely financial, Chandler said. But physical and psychological effects tend to follow — as well as a proclivity toward other addictions.
“Problem gamblers are prone to having suicidal thoughts; their suicide rates are higher,” he explained. “If they feel trapped, that can trigger a higher rate of substance abuse. We fully expect to be treating a lot of people with dual diagnoses here, people with depression, anxiety, co-morbid anxiety disorders, all associated with problem gambling.
“For some people, once they get their problem gambling under control, maybe the other symptoms go away. For others, there may be biological depression. Either way, we focus on treating it all at once, not compartmentalizing it.”
According to the MCCG, between 2% and 3% of the population has experienced ‘disordered gambling’ in their lifetimes, a loose umbrella term for gambling behaviors that disrupt an individual’s family, social, or vocational life in some way. By that estimation, up to 185,000 Massachusetts residents have likely engaged in disordered gambling at some point.
“When they come in for treatment, you’re asking them to abstain from gambling. For most people, it’s not about cutting back, but ceasing gambling, similar to someone coming in for alcohol,” Chandler said. “We support groups like Gamblers Anonymous and encourage a lot of people to check that out.”
HMC offers a three-week partial-hospitalization program for more serious cases, typically those involving dual diagnoses, such as severe depression or other addictions. Chandler said the hospital works closely with River Valley to match each patient with the appropriate type of care, from group counseling to individualized work.
“For many years, gambling has been sort of lumped in with all addiction,” Chandler said. “When someone comes in for treatment, we’ve always asked, ‘do you have an issue with gambling?’ Now we’re paying even more attention, making sure we’re asking the right questions.”
Upping the Ante
Gambling addiction accounts for some $7 billion a year in added healthcare and criminal-justice costs, according to the National Council on Problem Gambling, and a significant portion of that has nothing to do with casinos. But the issue certainly has taken on a higher profile in Massachusetts over the past two years.
“Casino gambling has been legalized, so now it’s much more in the forefront in Western Mass.,” Chandler said of his dealings with the MCCG. “For many years, we had contact with them. But now that Western Mass. is looking to get a casino, everyone is sort of scrambling to respond to that.”
Russell described the council as largely a referral service. “When people call our helpline, we try to connect them to an outpatient service in their area or a Gamblers Anonymous meeting. We have packets of information we send to support them and get them on a path to recovery.”
The MCCG also hosts an annual weekend retreat for people in recovery, offering various workshops on how to stay on track. And, of course, it has ramped up efforts to bring behavioral-health professionals into its certificate program.
“One thing I’m really proud of is, prior to us doing this training, there were probably three or four people with this certificate in Western Mass.,” Chandler said. “We were able to train nearly 25 people.”
He was quick to note that gambling in itself is not necessarily a vice. “One thing I respect about the Mass. Council on Compulsive Gambling is that they’re neutral on the issue of gambling itself. And as treatment providers, we’re not pro or against gambling, but we’re concerned with the impact it has on people’s lives.
“The same is true of alcohol,” he continued. “Alcohol by itself is not an evil thing. But if it impairs a person’s life, there are consequences. We can say the same about food, exercise, anything.”
Russell agreed. “It’s just like with any sort of drug or alcohol,” she said. “Some people can take a drug or drink alcohol and be fine and cut themselves off. Same thing with gambling — some people do it just to be social, and it’s not a cause for concern.”
One challenge is for people to recognize they have a problem, Chandler said, and the first signs are always the financial repercussions.
“If someone has to borrow money or obtain money in a way that gets them into trouble, just to cover gambling debts or continue gambling, that’s a big sign,” he told BusinessWest. “If people lie about their gambling, where they were, or how much they won or lost, withholding that information from people, that’s a sign, too. In a lot of cases, other people recognize the problem long before the individual does.”
Theoretically, Western Mass. could see a rise in problem gambling from locals who join the ranks of casino addicts — typically, 10% of a casino’s patrons account for 90% of its revenue — but Russell stressed that the lure of gambling is as close as the nearest convenience store, and has been for decades.
“A lot of people don’t think about it because gambling is such a big part of society in general,” she said. “It’s even in the everyday vernacular — like when people say, ‘wanna make a bet?’ So they don’t realize how many people can’t control themselves. They just don’t understand it.”
Joseph Bednar can be reached at [email protected]

Unlike the well-documented research into cigarettes, Lynn Ostrowski says, no one really knows what’s in e-cigs or what the long-term risks are.
Elizabeth Taras can be reached at [email protected]

Dr. Frank Gallo says trauma can paralyze people by causing them to constantly re-experience those negative thoughts and images, as if the event is happening again.
Living with the Pain
The center opened its doors on Birnie Avenue on Sept. 30 with a number of programs available to both emergency personnel and the public, with more being developed down the road, Gallo said.
The intensive outpatient treatment program, for example, is available weekdays, four hours a day, and features group-focused treatment to help patients recover from trauma, as well as one-on-one work with a therapist to craft a specialized treatment plan.
“People can get stuck in their traumas. People may feel numb inside, or they no longer feel safe,” he said, saying people are familiar with the concept of being swept off one’s feet in love, but an emotional trauma can make them feel knocked off their feet. “We get people reconnected with their bodies. We get them grounded, so they feel like they’re not easily knocked off their feet by trauma-related thoughts and feelings.”
A concept called ACT, or acceptance and commitment therapy, is at the heart of all the center’s programs. It helps individuals learn to be present with their trauma and open up to their experience, but choose to focus on what’s important to them.
One 10-week therapy group focuses on the idea of mindfulness, or what Gallo calls “healthy living through being present.” Mindfulness, he said, is essentially paying attention to each experience and thought without judgment, being aware of thoughts and feelings without getting swept up in them, and being awake to the positive things life has to offer each moment.
“We get people engaging in life, with what matters to them, while they carry their traumas with them,” he explained. “These are stories they hold, and it’s part of their experience, but it’s not the whole of who they are. We get people living life beyond the trauma.”
After all, he said, the goal isn’t to deny the trauma, but simply to assimilate the memory and its impact into a life of healthy, mindful choices.
“What people see is that the volume of that stuff goes down all by itself,” he added. “We help people develop new relationships with those trauma-related thoughts, memories, and emotions, and that frees them up to engage in ways that matter to them, even as they carry their trauma with them.”
As a continuation of his work in Brattleboro, Gallo has also instituted a specialized treatment program for first responders, including police officers, firefighters, correctional officers, military personnel and veterans, EMTs and paramedics, and trauma nurses and doctors.
Beyond trauma recovery, though, the center has begun working with emergency personnel on preventing programs to develop resiliency skills so they quickly recover from traumatic events in their work environments.
“They’re at much higher risk, so we’re trying to do some skill building and prevention work,” he explained. “We want to give them a skill set they can take throughout their career. My goal, in terms of community outreach, is to create a continuity of healthcare, and to give them the essential skill sets to do their jobs well and be able to bounce back more easily from exposure to trauma.”
The Traumatic Stress Recovery Center is also working to institute a series of services promoting ‘whole-person care,’ including yoga, aikido, acupuncture, and biofeedback, to give clients additional tools to boost their emotional health.
“We recognize that there are other types of programs we can offer to help in the recovery process,” Gallo said. “These are adjunctive groups people can participate in so that, once they finish treatment, they can continue in that recovery process.”
Giving Back
Gallo was quick to note that the center shouldn’t be the only entity in the region providing trauma-related services. He’s working with other organizations to develop their own trauma-resiliency training programs, and has also launched a teaching program for Ph.D.-level psychology students.
“Pychology interns have an opportunity to do practicum experiences here — professional development in becoming psychologists,” he explained. “We also have a research-based program where, in all our programs, we collect data on treatment progress — how well people are doing, and how well they’re doing once they leave here.”
This information, he said, will help the center understand what some of the trends are and where patients are struggling the most — data that could be used to expand or change the center’s services in the future.
Gallo’s career experiences, both as a police officer and a psychologist, have lent him a keen understanding of how emotional trauma affects lives, and he said his latest chapter is a way to give back to the community.
“I know what it’s like. You know the saying — ‘been there, done that, got the T-shirt.’ I know what it’s like to be in those situations,” he told BusinessWest. “These experiences can be so overwhelming for people; traumatic events can have such an impact on people’s lives. After retiring from the police department, I wanted to have an opportunity to give back — not just for uniformed services and first responders, but for the general population, people struggling wherever they are. I asked, ‘how can I do something meaningful for them?’ That’s why I’m doing this.
“We want people to see us as a resource,” Gallo continued. “Nobody does what we’re doing; we’re really unique in this way. I’m really excited about that. I’m excited to have an opportunity to lead a program and have a great staff of clinicians who really understand what people are struggling with and are excited about the opportunity to give back.”
Joseph Bednar can be reached at [email protected]
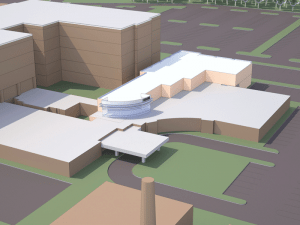
This planned 20,000-square-foot expansion to the Sr. Caritas Cancer Center will allow Mercy Medical Center to offer more comprehensive cancer treatment.
Dr. Philip Glynn serves as the cancer center’s new director of Medical Oncology, and has helped expand Mercy’s chemotherapy services.
Supply and Demand
As he talked about the changes and developments that put the Caritas Center expansion plans on the drawing board, Mark Fulco, senior vice president of Strategy and Marketing for SPHS, started with some rather sobering statistics regarding cancer in this country.
He said that analysis of data provided by the state Department of Health, national statistics, and interviews with consumers and community leaders reveals that the demand for medical oncology services is expected to increase by 11% over the next 10 years.
The aging of the nation’s population is a big factor in these estimates, but there are other factors that point to heightened demand both nationally and especially in this region, he went on, citing a smoking rate of 23.8% in Greater Springfield, nearly double the national average of 14.7%.
While these numbers indicate that Mercy was likely to eventually need more space and facilities at the Caritas Center, the recent merger with Glynn’s practice certainly accelerated that process, Fulco noted.
Wolf concurred, noting that this consolidation more than doubled the number of medical oncology treatments at Mercy, from roughly 3,000 per year to more than 7,000. And the expansion is designed to accommodate 30,000 annually.
“Phil is an incredibly gifted physician, and due to his presence in this community, he has an extremely loyal following,” said Wolf. “Oncologists as a whole are a special group of physicians, just because of the nature of their business, but Phil takes it to another level.”
The planed expansion will feature two floors of medical oncology services adjacent to the current single-story facility on the eastern side of the Mercy Medical Center campus that houses radiation oncology.
But there is much more to the expansion than additional square footage and infusion bays, said Fulco.
“What we’re putting together to meet greater demand for services is a truly comprehensive cancer center with cancer diagnosis, treatment, and other modalities, like support and our spiritual-care team, all in one place,” said Fulco. “The physicians will be in close proximity to each other so that it will further enhance collaboration efforts, with cancer being treated through a team approach.”
Elaborating, he said the new, enlarged Caritas Center will bring together what he called a talented team of clinicians.
Glynn is now responsible for all aspects of the medical oncology program and its activities, such as cancer prevention, screening, diagnosis, state-of-the-art treatment, counseling, and rehabilitation.
Glynn and his seven-member oncology team will be joined by Dr. Neal Chuang, the new chief of thoracic surgery, who is trained on the da Vinci S Surgical System, the latest in minimally invasive robotic-assisted surgery; Dr. Mark Sherman, also a thoracic surgeon and a new surgical oncologist; and Dr. Julia Donovan, a specialist in female reproductive cancers. Within the existing radiation department are Dr. Catherine Carton, the full-time director of radiation oncology; and radiation oncologist Dr. Mary Ann Lowen.
“Dr. Glynn has a very clear and progressive vision for where cancer care and interventions are going,” said Fulco, adding that Glynn’s keen interest in pursuing new interventions that aren’t currently available at Mercy, or anywhere else, for that matter, will see those new modalities being developed and eventually in use at the center.
For example, 10 years ago, when the current center opened, two linear accelerators (used for external beam radiation treatments) and intensity-modulated radiation therapy (IMRT) were hyped in the press as advanced technology; today, the team is proud of the two Elekta Infinity intensity-guided radiation-therapy machines, which are advanced linear accelerators (see sidebar, page 17), and are the only two of their kind in Western Mass.
Casting the net even wider, the business plan written 18 months ago by Daniel Moen, president and CEO of SPHS, with Wolf, Glynn and others, demands that the team be consistently aggressive in seeking new technology, new treatment modalities, and new relationships.
To that end, Wolf said the team is in the early stages of identifying a tertiary partner, one that would offer access to clinical trials, second-opinion expertise, genetic profiling, and many other services that will be demanded of a truly comprehensive cancer-care facility.
Fulco said this represents the type of forward thinking that is a very important motivation for Glynn, who also assists with the development and implementation of new program initiatives, such as cancer survivorship, navigation, community outreach, and clinical research/clinical trial participation.
Progressive Vision
Fulco told BusinessWest that, when plans were first put on the drawing board for what would become the Sr. Caritas Cancer Center, the overarching philosophy was to create a facility that would drive home the point that area residents did not have to drive to Hartford, Boston, New York, or anywhere else to receive quality cancer treatment.
Over the past decade, the facility has gone a long way toward proving that point, and the planned expansion of the center will only make it easier to make that argument.
“Except for the esoteric type of cancer that requires specialists who are just as rare and requires experimental therapies, the modalities that we have available to treat patients here are equivalent to the very best in the world,” said Fulco. “You don’t need to go to Boston or New York to get a leading-edge treatment.”
Elizabeth Taras can be reached at [email protected]
Delicate Subject
Massachusetts has been trying to get children — and parents — thinking about obesity for some time, including a controversial, recently ended program that measured children’s body-mass index (BMI) at school and sent notes home to the parents of kids classified as obese. Detractors of the program cited privacy issues and also argued that the notes could lead to bullying.
Specifically, schools said it was too expensive to mail the letters, so they often sent them home in students’ backpacks, which sometimes resulted in disclosure of the information to other students — and, often, teasing.
“There has been a lot of controversy about taking away these letters going out to parents or caregivers, saying, ‘your child is obese; please seek guidance or help from your physician,’” Conroy said, noting that other states had conducted similar programs and determined they were ineffective.
But despite such reports, and the understandable risk of teasing, she has mixed feelings about the decision to stop the letters, “because I do feel it’s important to have that awareness coming from the schools, and not just a medical professional.”
The state’s Public Health Council, an appointed body of academics and health advocates, called for an end to the letters, but still requires schools to conduct weight and height screenings in grades 1, 4, 7, and 10 to help officials gather data about obesity trends and identify possible solutions — a practice in place in 20 other states. Parents may request their children’s BMI information in writing if they wish.
And parents do seem to be more aware of the obesity problem, as evidenced by the declining rates among all age groups across the U.S. “As far as the nation goes, we’re overall more aware of what’s happening and what we as adults can do for our children,” Conroy said.
She noted that, while the medical community has always stressed lifestyle choices to prevent obesity, the alternatives for helping people rein in their weight have broadened significantly.
“From a treatment standpoint, there are more options available,” she said. “Lifestyle modification will always be the first line of defense, but now bariatric surgery and medications offer more options.”
Weight loss from lifestyle modification generally results in a loss of about 10% of total weight in a year, she noted, often not enough to combat the serious medical conditions that afflict many obese individuals. And the side effects of some weight-loss medications can be a deterrent to their taking those prescriptions. That leaves bariatric surgery as an effective last resort.
For example, Baystate Children’s Hospital now offers bariatric surgery to younger patients than ever before, in the form of sleeve gastrectomy, an increasingly common form of gastric surgery that removes all but a narrow ‘sleeve’ of the stomach, forcing patients to eat much less than before.
“Despite the fact that obesity has declined somewhat in the country, there are still many children whose weight remains dangerously high,” Conroy said. “For some of these adolescents whose weight exceeds 200 or 300 pounds, many are at risk for or already suffering from serious health problems such as diabetes, hypertension, heart disease, depression, sleep apnea, and liver disease, which can make it harder for them to lose weight.”
Studies on adolescents having bariatric surgery suggest the operation is as safe for them as for adults, but not enough teens have been followed after the sleeve gastrectomy to know if there are any long-term effects on their future growth or development. But Baystate has begun admitting 17-year-olds into the bariatric pre-op process, so they’re ready for the surgery at age 18 — with the potential to operate on younger teens down the road as more data emerges.
Go Outside
Of course, encouraging young people to eat right and exercise is still job number one, and that can be difficult, especially in an era when kids simply don’t play outside as much as they did decades ago.
“Parents say, ‘my neighborhood is not a very safe one; I wouldn’t want my children outside,’ or ‘I can’t afford a gym membership or a YMCA membership,’ or ‘I don’t have transportation to take them,’” Conroy told BusinessWest. “There are lots of different reasons why people to find it difficult to be active.”
One positive development, she noted, has been the popularity of video-game systems, like the Wii, that incorporate full-body movement. “Another thing we talk about is families doing chores around the house. That counts as exercise, too — helping mom with the sweeping or laundry, for instance.”
She also said both young people and adults should find ways to include more physical exertion in their daily routine, whether it’s walking to school (if possible) or not searching for the nearest parking spot when out shopping. “If you’re going to the mall, park farther away; instead of spending 15 minutes finding a spot closer to the entrance, park at the back and walk. These are ways of getting activity in.”
She understands, of course, that in an increasingly wired world, kids are going to spend time in front of their devices. So she suggests setting rules for their use. “Say, ‘you can spend an hour playing video games, but you have to spend an hour doing exercise first.’ The challenge is getting parents to enforce that rule, because we’re not going to be there to do it for them.”
Joseph Bednar can be reached at [email protected]

Dr. Richard Wait says surgery can be effective in extending life for pancreatic-cancer patients, but detecting the disease in time is often difficult.
The Only Option
Once a tumor is found, the only possible cure is still surgery, Wait said. “The surgery is aimed at taking out that portion of the pancreas that contains cancer.”
For tumors in the pancreatic tail and body, a surgeon will remove the tail and a small portion of the body — and possibly the spleen — in a procedure called distal pancreatectomy. For cancer located in the head of the pancreas, the surgeon will remove the head as well as a portion of the small intestine, the gallbladder, and part of the bile duct. Part of the stomach may be removed as well.
This surgery is known as the ‘Whipple procedure,’ named after Dr. Allen Whipple, who first developed it in 1935. “It’s still basically the same procedure, although the results are better,” Wait said. “It has been shown that the results for the Whipple procedure and other pancreatic-surgery procedures are better in those institutions that do large numbers, so we always encourage patients to go to high-volume centers, of which Baystate is one.”
Surgical treatment is usually reinforced by both chemotherapy and radiation therapy after the procedure, he added. “On occasion, we’ll use chemotherapy first, before the surgery, if the tumor is large.”
Because removing part of the pancreas decreases its endocrine function, blood sugar is typically higher after surgery, he explained. “If you were diabetic before, you’ll be more diabetic after and maybe need stronger medicine. If you were not diabetic before surgery, oftentimes you are after surgery, but you may not require insulin — just diet modifications or oral medications.”
When pancreatic cancer is diagnosed and the doctor determines it’s operable, Wait said, “the average survival time is 11 months if we don’t do surgery, and the average time if patients receive full treatment is 22 to 24 months — about double the life expectancy.” Most people who make it to five years can consider themselves cancer-free, he added.
Seeking Answers
To demonstrate the disease’s harsh mortality rate, Wait noted that 1 in 78 people contract pancreatic cancer, as opposed to 1 in 6 women who are diagnosed with breast cancer at some point — yet, because breast cancer is far more manageable, the total annual deaths from the two are very similar.
“There are no screening tests for pancreatic cancer,” he reiterated. “Some things are being developed in an attempt to screen for it, but nothing yet has been proven useful. In fact, a high-school student in Maryland did some work at Johns Hopkins and came up with a urine test, which they’re testing right now.”
Historically, however, answers have been frustratingly elusive.
“Our hope is that we find some way to screen patients and develop some new DNA testing that may show which people are most vulnerable to developing pancreatic cancer,” Wait said, “and also develop therapies that will really improve survival, because it’s clear that surgery alone almost always only extends survival, but doesn’t cure the patient.”
Because, even if pancreatic cancer remains a death sentence, every month of life counts.
Joseph Bednar can be reached at [email protected]
Todd C. Ratner is an estate-planning, elder-law, business, and real-estate attorney with the regional law firm Bacon Wilson, P.C. He serves as the co-chair for the Alzheimer’s Assoc. Tri-County (Hampden, Hampshire, and Franklin) Partnership and is a member of the National Academy of Elder Law Attorneys and the Estate Planning Council of Hampden County. He is also a recipient of Boston Magazine’s Super Lawyers Rising Stars distinction from 2007 to 2011; (413) 781-0560; baconwilson.com/attorneys/ratner_2
By Dr. BARRY SARVET
It practically goes without saying that human beings need to eat.
Eating is not only necessary for survival, but what we eat and how we eat is often a fundamental aspect of one’s personal and cultural identity. For the newborn infant, feeding serves as one of the primary foundations of the relationship with his or her parent or caregiver, and a positive feeding experience in infancy and early childhood is vital to healthy physical and psychological development.
Continuing throughout the lifespan, eating together with family, friends, and co-workers strengthens relationships and builds community. Some even consider eating to be one of the most pleasurable activities of life.
Although difficult for many to understand, there are those among us for whom eating is associated with a terrible inner struggle. Individuals with anorexia believe themselves to be overweight and deny themselves food even when they are literally dying of starvation. Others diagnosed with bulimia are trapped in endless cycles of uncontrollable eating alternating with dangerous efforts to purge themselves of the food they’ve eaten. According to the National Institute of Mental Health, an estimated 6% of the adult population in the U.S. suffers from anorexia, 1% from bulimia, and 2.8% from a binge-eating disorder. Women are much more likely than males to develop an eating disorder and are three times as likely to experience anorexia and bulimia.
For many patients with eating disorders, the onset of symptoms occurs during adolescence. Without treatment, patients may develop chronic symptoms that cause significant medical and psychological disability throughout their adult lives. Some experience a particularly malignant course that may result in death if left unchecked.
Although numerous physiological, psychological, and environmental factors are thought to be associated with the development of eating disorders, it is very common for these disorders to be triggered by intensive weight- management regimens, including severe dietary restriction and rigorous exercise regimens. It is thought that the experience of starvation caused by intensive dieting may trigger physiological changes in the brain that contribute to some of the highly compulsive patterns of behavior, irrational thoughts, and distorted perceptions of the body associated with anorexia.
Many experts believe that another important factor contributing to the relatively high prevalence of eating disorders is the influence of popular culture and advertising media in contemporary society. Advertising and entertainment media seem to promote superficial and unrealistic norms of beauty and associate unnatural thinness with glamour and success. At the very same time, young people are encouraged by the same media to instantly gratify their desires and purchase and consume high-calorie fast foods and snacks.
There are numerous approaches to the treatment of anorexia and bulimia. One of the first priorities in the care of patients with eating disorders is a careful medical assessment. The primary-care provider is an important starting point for this assessment, although, depending upon the degree of starvation, patients may need to be monitored in the hospital setting in order for their weight to be safely restored. Beyond the immediate safety of the patient, medical stabilization and weight restoration is a necessary part of the psychological recovery of the patient. Patients with severe metabolic abnormalities associated with the state of starvation are usually not able to benefit from psychotherapy.
As soon as patients with eating disorders are medically stable, psychotherapy should be provided. In the Greater Springfield area, there are numerous psychotherapists who are experienced in the treatment of patients with eating disorders. Therapy must be customized to the needs of the patient and should involve the family whenever possible. Some approaches to therapy focus on helping the patient understand and fight against the irrational thoughts and behaviors associated with the eating disorder. Others focus on improvement in self-esteem and coping with negative emotions and conflictual relationships.
A particularly promising form of treatment for adolescent patients is family-based therapy for eating disorders, also known as the Maudsley approach. In this form of treatment, parents initially receive a great deal of support and coaching in order to leverage the power of their parental relationship in overcoming the child’s resistance to eating. As treatment progresses, the therapy shifts toward gradually promoting the teenager’s independence and autonomy in the family. Although this type of therapy is not suitable for all patients, the outpatient Child Behavioral Health Associates at Baystate Medical Center has seen excellent results with the use of family-based therapy.
Eating disorders are notoriously challenging conditions to treat. In the throes of their illness, patients often are in a battle for control with doctors, therapists, and loved ones who are trying to get them to change. Researchers are constantly looking for new therapeutic treatments that could help motivate patients to get treatment and develop a more accepting and comfortable relationship with their bodies.
There have been preliminary studies suggesting that the practice of yoga may have such an impact, and may therefore be a valuable part of the treatment plan. At Baystate, we are conducting a research study investigating the impact of a 12-week program of gentle yoga practice on some of the core symptoms of eating disorders. The study is supported through the generosity of the Calabrese family, who established the Lisa’s Light of Hope Fund at the Baystate Health Foundation in memory of their beloved daughter Lisa Calabrese, whose life was tragically lost after a long battle with an eating disorder.
The program, designed for teenage girls and young women ages 16 to 21 who have been diagnosed with an eating disorder, meets twice weekly at Yoga Sanctuary in Northampton. Sessions are conducted by a certified yoga instructor in collaboration with a clinical psychologist, and include gentle yoga practice along with brief group discussions. Participants are asked to complete questionnaires before and after the program to assess the severity of symptoms of their eating disorder and other associated symptoms. Those interested in participating in the program, or learning more about it, can contact Jennifer McCaffrey at (413) 794-6628.
For more information about research at Baystate Medical Center, visit baystatehealth.org/research, and for more information about Baystate Children’s Hospital, visit baystatehealth.org/bch.
Dr. Barry Sarvet is vice chair of the Department of Psychiatry for Baystate Health, and chief of Child and Adolescent Psychiatry at Baystate Medical Center.
Jolene Lambert (right) says HMC’s patient-navigation program has helped increase the hospital’s breast-cancer survival rate.
Breaking Down Barriers
The concept of patient navigation was first developed by Dr. Harold Freeman in Harlem, N.Y., as an effort to reduce disparities in access to diagnosis and treatment of cancer, particularly among poor and uninsured people.
“During his practice, he realized he was seeing a lot of women who presented to him with stage 3 breast cancer,” Lambert said. “He felt there should be some way to get to these people because there is a cure for breast cancer if it’s detected early enough.
“So he devised a whole navigator program — not only following people through the disease, but getting out there in the community, getting people to their scheduled mammograms, offering them rides, and preventing barriers to getting mammograms, whether they don’t have insurance, they’re afraid, they don’t have transportation, or they don’t want to pay the co-pay, but would rather spend the money to feed their families. He helped them overcome the barriers to get the care they need.”
Community Minded
Lambert said no navigator program is complete without a public-outreach component that aims to identify cancers before they’ve advanced. She has distributed booklets throughout Holyoke, given several talks in the community, and recruited four physicians and two nurse practitioners for a free breast-cancer screening in March.
“We’re trying to reach all those people,” she said of such efforts. “In October, we’ll be at Stop & Shop booking mammograms on laptops.”
Once they’re in the system — particularly if a doctor detects early-stage breast cancer — she said patients are grateful that someone gave them the nudge to get checked. But she also deals with cultural barriers to care. “A lot of patients have certain religious beliefs, and think they have cancer because they’ve done something bad in their lives.”
Whatever the barrier, Lambert said, her job is to help break through it to get locals the help they need. After all, the mortality rate from all cancers combined has fallen to one-third what it was 40 years ago, and “immediate care and follow-up care are a big plus for these people.”
Patients are grateful for these targeted efforts to treat their cancer and keep them healthy, Mertens said. “They really appreciate the relationship. They spend a fair amount of time contacting the nurses, and the amount of information they receive is very robust.
“I think that it’s a great comfort for them,” he added, “and it’s a comfort for us on the physician side to know they have another healthcare professional with a deep, profound knowledge of what the patient is going through and can get the appropriate services they need.”
One challenge for the future, Mertens noted, is the still-unclear effect of healthcare reform, and new models of treatment like accountable-care organizations, on patient navigation. “There’s no specific payment for navigation, even though we think it’s critical and needs to be provided,” he said. “We’re not sure exactly what it’s going to look like.”
Still, the trend in oncology has been toward more navigation services, not fewer. And that’s bringing a measure of comfort to patients during some of the most difficult times in their lives.
“I had someone say to me the other day, ‘I don’t want to go to Holyoke; I had a bad experience there,’” Lambert said. “I said, ‘try it again; I’ll go with you.’ She said, ‘you would?’”
And she did just that, relieving the anxiety for one more woman in need. “If you don’t have a medical background nowadays,” she said, “you are lost — very lost.”
And when you’re lost, a navigator sure comes in handy.
Joseph Bednar can be reached at [email protected]
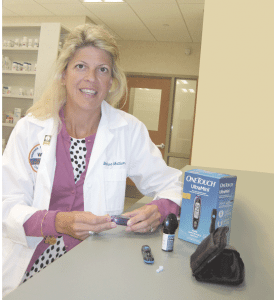
Melissa Mattison, clinical assistant professor at the Western New England University College of Pharmacy.
It’s Weighing on Them
When it comes to obesity, diabetes, and the collective impact on the role pharmacists play, the numbers tell the story — or a big part of it, anyway.
The most recent statistics from the Centers for Disease Control and Prevention show that more than 23 million Americans, or close to 8% of the population, have diabetes, and more than one-third of the adults in this country (35.7%) are clinically obese. These numbers have doubled in just the past two decades, and current projections show that the number of people with diabetes in the U.S. will rise to 48 million by 2050.
And this dangerous trend is quite visible in Western Mass. and especially its largest city. According to the Mass. Behaviorial Risk Factor Surveillance System, Springfield has the highest percentage of adults diagnosed with diabetes in the Commonwealth (13.1%) and the highest percentage of adults being told they have pre-diabetes (10.2%).
The impact of all this on pharmacies is made clear by statistics compiled by the Pharmacy Times which show that, while the average consumer spends $300 annually on retail pharmacy purchases, a consumer diagnosed with diabetes will spend $2,500 on average each year in medication, insulin, blood-glucose-monitoring products, and other over-the-counter supplies.
These alarming statistics help explain everything from the rising numbers of health screenings in pharmacies (especially the larger chains) to the fact that many different types of medical equipment have been altered and recalibrated to reflect a much heavier America.
“It really sticks out on the medical-equipment side,” said Matthews, noting that the walkers, canes, hospital beds, bath-transfer seats and commodes that his stores sell, which once were ‘200-pound rated’ (to support patients up to that weight), now come rated at 250, 300, or 350 and higher for the morbidly obese. “The manufacturers have changed what they make, and we’ve had to change our product mix accordingly.”
But perhaps the biggest change that can be traced to those statistics has been the emergence of the pharmacist as educator and counselor, said Mattison.
Elaborating, she said that, in many respects, the pharmacist acts as a liaison between the patient and the primary-care physician.
“In pharmacy school, our focus is not just on the disease state and what the medications are used for,” she noted. “Now, the pharmacist has the responsibility, and the privilege, to spend time with the patient and say, ‘look, Mrs. Jones, we did your screening, and your body-mass index is in the obesity range; what do you know about that? Can I talk to you about that?’”
Matthews agreed.
“There is a greater recognition of the role of pharmacists, even by insurance companies and doctors, in just the past five years, and that wasn’t always the case,” he told BusinessWest. “That’s because the pharmacist brings a lot of value, due to his or her position in healthcare between the doctor and the patient.”
Dispensing Information
This larger, more prominent role takes many forms, said those we spoke with, who noted, for starters, that pharmacists are doing much more, historically speaking, to hold patients accountable for adhering to their medication and recommended lifestyle changes.
“Typically, diabetic patient-adherence rates are somewhere around 50%, so they don’t take their medication every day, and for numerous reasons,” Mattison told BusinessWest. “Adherence is a big push now with pharmacist intervention.”
There’s also that educational component, she went on, adding quickly that, while pharmacists have always welcomed and answered questions, they’re doing much more of that today.
“Now, they [pharmacists] are on the ground floor, and many of the new pharmacists are out on the floor with an iPad and helping customers,” she explained. “They are the first person that the patient sees [after a doctor’s visit], and they can be a continuing point of contact.”
This ongoing evolution in the pharmacist’s role brings with it both opportunities and challenges, said Matthews and Mattison.
In that first category, they place the prospects for growth that come with quality customer service, which takes on new meaning in the expanded role. In other words, pharmacies and individual pharmacists can stand out as a result of how well they accept — and carry out — their new responsibilities.
Mattison added that pharmacies have an advantage over other retail outlets in that they have the opportunity to sell the self-management items diabetic patients need, and also the experience and knowledge needed to offer positive medical support. For this reason, retail pharmacists may choose to place their diabetes-care display near the pharmacist’s counter, or place weight-control and nutritional foods, vitamins, and dietary supplements near the diabetes-care section. The marketing-savvy pharmacists will offer more and more product demonstrations, educational sessions, nutritional advice, blood-pressure screenings, coupons, and store sales.
As for challenges, perhaps the biggest stems from the fact that, in simple terms, pharmacists are not paid to dispense information and be that liaison between patient and physician, said Mattison, adding that doing so takes time, which in this business (or any other, for that matter) is money.
“The expanding role of the pharmacist now involves much more than counting pills,” she explained. “But the problem becomes, who’s going to pay for it, or make it reimbursable, and create a profitable model for the pharmacy?”
Another challenge, Mattison continued, stems from the fact that this broader, pharmacist-as-educator role requires a skill set that for many must be acquired.
And the university is responding accordingly, she said, adding that, in addition to a year-long class focused on the business skills needed for setting up and then operating a successful pharmacy, the school also includes a customer-service component within its healthcare communications class.
It teaches students how to talk compassionately with patients, adherence to a doctor’s plan, and how to navigate customers’ financial, socio-economic, and language issues.
One of the more hands-on aspects of healthcare communications is the process of physically putting the student in the patient’s position, she noted, by making them wear heavy gloves and macular-degeneration goggles that mimic deteriorating eyesight. They’re then asked to read a prescription or open a bottle of pills.
“And they find they can’t do it,” she went on. “So now this 22-year old student gets the perspective of a 78-year old patient, and it teaches them empathy.”
Counting on Them
Empathy is just one of many skills pharmacists now need to do their jobs effectively.
Indeed, where once being able to count was the most visible skill set, now, those in this profession must be able to listen, consult, and help lead their customers to healthier lifestyes.
The epidemic of obesity has much to do with this phenomenon, and all indications are that it will continue to be a large problem — in every sense of that phrase — for a long time to come.
Elizabeth Taras can be reached at [email protected]

Dr. Stephanie Carlin says a belief that vaccines cause autism persists in some pockets of the community.
Joseph Bednar can be reached at [email protected]
Avoiding the Court Process
Fortunately, with proper planning, it is possible to avoid the court process. If a durable power of attorney and healthcare proxy have been signed, the individual has named someone who can make all financial and/or medical decisions on their behalf. A durable power of attorney is a legal document that names someone to make financial decisions in the event of incapacity. A healthcare proxy is a legal document that names someone to make medical decisions in the event of incapacity. You must be competent to execute these documents, and thereafter, upon incapacity, there is no need for a guardian or conservator because individuals are already in place to make those decisions. Having both a durable power of attorney and a healthcare proxy is absolutely crucial to avoiding guardianship.
While you are competent, you have the ability to name the people that you would want to make decisions for you if you could not make them for yourself. By doing so, you will eliminate the loss of privacy, money, and time that is associated with the guardianship and conservatorship process. Establish proper documents now, and keep the court out of your personal decisions.
Gina M. Barry is a partner with the regional law firm of Bacon Wilson, P.C., Attorneys at Law. She is a member of the National Association of Elder Law Attorneys, the Estate Planning Council, and the Western Mass. Elder Care Professionals Association. She concentrates her practice in the areas of estate and asset protection planning, probate administration and litigation, guardianships, conservatorships and residential real estate; (413) 781-0560; [email protected].

Spiros Hatiras is slated to take the helm at Holyoke Medical Center in September, succeeding long-time president and CEO Hank Porten.
That’s how he chose to describe his mindset during what would become the latter stages of his tenure as chief executive officer of NIT Health in New York, a health-informatics company that specializes in the implementation of electronic medical records for hospitals and healthcare systems.
He enjoyed the work and found it rewarding in some respects, but the more he was in that position, the more he realized just how much he missed what he would later describe as his passion — leading a small community hospital.
“I really missed hospital administration,” said Hatiras, who joined NIT after a two-year stint as president and CEO of Hoboken University Medical Center (HUMC), where he also served as chief operating officer, vice president of Administration, and many other positions during a 19-year tenure. “I missed that sense of community, that relationship building that goes on when you’re part of a team.”
So Hatiras eventually put the word out to executive search firms that he would be interested in returning to that realm. But there were some caveats, or conditions under which he would like to do so, he told BusinessWest, adding that he set out what he called a “profile.”
The institution in question had to be in a good location, preferably the Northeast, he explained, adding that he preferred a community hospital with 200 to 300 beds in a small to mid-sized community (the situation at HUMC), and one with a good staff and a reputation for quality. The facility also had to be in “good shape,” which in this case meant the soundness of both the physical plant and the fiscal bottom line.
“I didn’t want to walk into a dire situation — I’ve been involved in those, and while it’s rewarding when you can pull out of one, I didn’t want to get back in a situation where, from day one, you’re struggling to keep your head above water,” he said, adding that one institution he was asked to consider could check all those boxes and thus fit that profile — Holyoke Medical Center, which was seeking a successor to Hank Porten, who announced he was stepping down after nearly 30 years at the helm of that facility.
Fast-forwarding a little, Hatiras eventually prevailed in a nationwide search for HMC’s new director; he is slated to start in early September. He spoke with BusinessWest late last month about why he chose to accept this challenge at this stage of his career, while also touching on the challenges moving forward — for all community hospitals, and especially HMC.
At the top of that list is fiscal stability, he said, noting that ‘survival’ is too strong a word for a facility that is in decent condition financially, but still must fight for every dollar in reimbursements from payers and aid from the Commonwealth.
“This is simply a hospital that needs to keep its eye on the ball,” said Hatiras, noting that HMC is what’s called a “safety-net hospital” in Massachusetts, one that receives a combination of state and federal assistance to offset the large amount of free care that such facilities provide; Mercy Medical Center is also one. “We need to make sure we don’t miss an opportunity when it comes to grant money and other programs.”
There are other matters to contend with, such as updating a long-term strategic plan for the facility, and also improving visibility and awareness of a medical center that has a solid reputation and many quality programs, but remains too much of an unknown quantity in this region.
“What I’ve heard loud and clear from everybody is that we do a lot of great things here — we’re the number-one stroke center in the state of Massachusetts for performance, and we have a lot of other great programs — but folks here think we don’t put it out to the community enough, and people don’t know about them,” he explained. “We need to figure out a way to get the message out, because if you do wonderful things and no one knows about them, you can’t get the recognition and the patients you need.”
Background — Check
Hatiras told BusinessWest that, unlike many hospital administrators today, he started out in direct patient care, as a physical therapist.
“I remember my first day on the job at St. Mary, which is what the hospital was called before it became University of Hoboken Medical School,” he said. “I got yelled at by the head nurse because, after I was finished with a patient, I left the bed rail down, and she was concerned about the patient falling out of bed.
“This gives me a good perspective; I’ve treated patients, I know what pain is like, especially in physical therapy, and know from a staff’s perspective what it takes every day to take care of patients,” he continued, referring to the many career stops he’s made and titles he’s held, ranging from corporate director of Rehabilitative Services to vice president of Post-Acute, Ancillary, and Support Services. “I started with patient care at the bedside, I’ve done home care, I’ve done nursing care and rehab — and my management style reflects all this. I’m easygoing, I can establish a rapport with patients and staff easily, and I’m personable. I like to walk around and talk to people, eat in the cafeteria, and chat with people; my door is always open.”
And at HMC, that door will be in the hospital, he went on, noting that Porten moved to what was supposed to be a temporary office in another building on the medical center’s campus during an extensive renovation and expansion project undertaken in the late ’90s, but that move turned out to be permanent.
“I’ll find space — I don’t care if it’s in a closet,” he explained. “For me, it’s very important for physicians, employees, and managers to easily access me, and for me to be close to patient-care areas.”
This is how it was at HUMC, which Hatiras led through a situation that could only be described as dire. Indeed, during his tenure, and while transitioning the hospital from municipal to private ownership, he implemented fiscal controls that resulted in a 50% reduction in operating losses, from a $22 million loss in FY 2008 to $11 million in FY 2009. He also achieved a balanced budget the next year, without a reduction in force, by negotiating concessions with employees, physicians, and vendors, which resulted in savings of more than $15 million for two years.
Other accomplishments at HUMC include implementation of an electronic-medical-records system, creation of a hospitalist program, and the securing of a number of grants for operational and infrastructure improvements.
The challenges at HMC will be different, as most all of the above, including financial stability, has been achieved. Looking ahead, he said, beyond finding space for his office, the immediate priorities are to meet with a host of constituencies — physicians, employees, the board of directors, business leaders, and Holyoke city officials — to get a better feel for how well the facility is serving the community, and where change and improvement is needed.
Hatiras said he’s already met with a number of employees and physicians during a few visits to the medical center for interviews, and a few others after he was hired. He came away impressed with the long tenures of many of those he met, but also somewhat intimidated by the notion that many will be retiring within the next decade or two.
“The longevity here is amazing,” he noted. “It seemed like everyone I met said they’d been here 30 years or more. That’s fantastic, but it’s also a challenge; we have to make sure we have good people to follow. That’s something we have to plan for.”
Let’s Get Fiscal
While he won’t have to contend with mass retirements any time soon, there are some matters that will need more immediate attention.
At or near the top of that list is being ready as a community hospital for what is still in many respects an uncertain future in the healthcare industry.
“This is a big unknown — I think healthcare reform is not done with us yet, not by a longshot,” he said, referring to payment reform — specifically, paying providers to keep people healthy, not just for treating them when they’re sick — and other issues. “Is there a formula under which community hospitals can survive? I think there is. I’m not of the opinion that you have to merge with someone or be affiliated with someone to survive, but it’s not an easy road, either.
“If you work with your community, if you work with your physicians, and if we’re heading in the direction of payment reform and population health, then I believe community hospitals have a better chance of leveling the playing field,” he continued. “If it continues to be simply a volume game in the future and a rates game, then that’s a harder game to win; the bigger hospitals get the bigger volumes, and they get the higher rates from private payers.”
Another issue moving forward is raising HMC’s profile in the region, he said, adding that this is a big part of the challenge of changing the perceptions, and habits, of people who believe they can get better care in Springfield, Hartford, or Boston than they can in Holyoke.
It’s a situation Hatiras said he faced in New Jersey, when he assumed management of the rehabilitation hospital within St. Francis Hospital (part of the Franciscan Health System of New Jersey), which operated in the shadow, figuratively and almost literally, of the Kessler Institute for Rehabilitation, known for treating Christopher Reeve, among countless others.
“When they needed rehab, people automatically assumed that the best place to go, and the only place to go, was Kessler,” he said. “Here we were, the new kid on the block trying to attract those patients, and they would literally travel from our community 15 or 20 miles to the Kessler facility.
“Changing people’s perceptions is a lot of hard work,” he continued. “It’s relationship building, word-of-mouth referrals, and you have to make sure that people have a good experience and people feel good enough about it to tell others.”
At St. Francis, administration and staff did a lot of what Hatiras called “legwork,” which included everything from providing high-quality care to making sure that physicians in that area were aware of the outcomes, and that they were comparable, or better, than Kessler’s.
“That’s really the only way you can do it,” he went on. “Yes, you can put up a billboard, and you can put an ad in the paper — and those are necessary too — but the best advertisement, and the best marketing, is when people say, ‘I had a great outcome, the people were nice, I was in and out, I had a great experience.’”
Moving forward, HMC will try to use similar legwork, and perhaps some of those advertising vehicles, to make it known that it has a lot going for it, said Hatiras, from a location right off I-91 to a strong track record with regard to outcomes.
“We want to be the place for the immediate community, the neighborhoods right around the hospital,” he said, “but we also want to be the place for the people who choose to come here, because they’ve seen something good about it or heard something good about it, not just because they live next door. There is a lot to build on here.”
At Home with the Idea
In a month or so, Hatiras will no longer be homesick.
Instead, he’ll be home, in hospital administration, and presumably in an office in the main building at HMC not carved out of a closet.
As he talked with BusinessWest about the type of scenario he desired as he returned to hospital management, he said he didn’t want a dire situation, but certainly did covet a challenge.
“I get easily bored with routine,” he said with a laugh. “I need spice in my life. Healthcare in general provides enough of that, but if you’re in a small place that needs to fight for every dollar, that usually provides a little more spice.”
And that’s one more reason why HMC fit his ‘profile,’ and is now the next line on his résumé.
George O’Brien can be reached at [email protected]

Dr. Adam Kasper, who recently moved back into his childhood bedroom, says Baystate was his first preference when ranking hospitals for his residency.

Dr. Elizabeth Langmore-Avila says she finds work in behavioral health, and especially with those battling substance abuse, to be professionally rewarding.
Meeting Their Match
As Dr. Laura Koenigs, director of the Pediatric Residency Program at Baystate, talked about Match Day, she referenced what she called the “computer in the sky.”
Others we spoke with used similar language, calling it simply “a computer” or “the computer,” or “a very complicated logarithm.” What it is, where it is, and what it’s called, no one seemed to know.
What they did know is that the software program in this computer would somehow determine their fate — for the next four years and possibly for the duration of their careers in medicine.
It’s called Match Day, because that’s when thousands of matches are announced, said Koenigs, adding that both medical students and teaching hospitals that interview them send their preferences for various specialties to that aforementioned computer, which ultimately analyzes a host of factors and determines where each medical-school graduate will go next.
“You rank programs, and the programs rank you, and you get matches — that’s what the computer does,” said Langmore-Avila, adding that med school students first learn if they’ve been matched (and more than 80% are), then must wait five agonizing days to find out which hospital they’ve been matched with.
Teaching hospitals like Baystate will weigh everything from academic performance to Springfield’s climate — “the cold and the dark can really impact some people,” said Koenigs, referring to the region’s long winters — when they submit their preferences. Meanwhile, medical-school students, some of whom will apply to a few dozen hospitals, will have their own criteria and priorities.
This year, the pediatric program took on 12 new residents, with half of them calling Massachusetts home, and four from the Pioneer Valley.
Dr. Shannon Rindone is among them.

Dr. Shannon Rindone says she gravitated toward pediatrics because she finds the work challenging and rewarding.
Close Calls
Kasper can relate.
He said he was drawn to pediatrics while moving through the core clerkships during his third year of medical school at Temple. These also included internal medicine, surgery, family medicine, ob/gyn, and others, with pediatrics somewhere in the middle.
“I just found that I was more interested in the material,” he said of his chosen specialty. “I actually didn’t mind going home and reading about the topics as much as I did some of the other rotations. I just found that I enjoyed going to the hospital a little more each day — I knew this was where I was supposed to be.”
Elaborating, he said he liked the “patient population,” found his personality is better suited for that field than others, and, overall, considered it both more challenging and more rewarding than other areas of practice.
“The potential impact that you have,” he explained, “is much greater than when you’re treating a 70-year-old who’s been smoking for the past 50 years and has no intention of changing anything he does no matter what you say.”
Currently on the genetics rotation, Kasper said behavioral development is next, and as he looks ahead, he’s eyeing each of the segments with equal amounts of anxious anticipation and “dread about how well I’ll perform in them, because I’m still getting my feet under me and getting used to working at this hospital.
“They’re equally exciting to me right now because I’m entering residency the same way I while I was in medical school,” he continued. “I don’t know exactly where I want to go in pediatrics, so each thing is a possibility.”
Rockwell said she’s in a similar state, one where the options are many and most have yet to be explored in depth.
She segued into medicine while majoring in geology and comparative literature at Hamilton College in New York. “You could write about rocks, I guess,” she said with a laugh when asked what one could do with those degrees, adding quickly that she always had medicine in the back of her mind, did pre-med work at Hamilton, and was an EMT on campus.
She enrolled at the University of New England Medical School in Maine, where, like Kasper, she zeroed in on pediatrics rather late in the game — it was her last rotation, and she found she enjoyed working with children and families.
On Match Day, she was in surgery at a hospital in New York City when the clock struck noon and the results are posted. “The surgeon let me scrub out,” she recalled. “I opened my phone, and it was there in an e-mail: ‘Margo Rockwell; Baystate Medical Center; Pediatrics.’
“You were waiting all year for that e-mail, so it was pretty exciting,” Rockwell went on, adding that pediatric endocrinology was her first rotation, and that two months in the NICU, November and May, lie ahead.
She said she might get to work with her father, although they will likely be on different teams. And in the meantime, he’s been a great resource. “I certainly ask him a lot of questions.”
Meanwhile, Langmore-Avila is working with much older patients in Baystate’s Adult Psychiatric Treatment Unit, the adult inpatient facility at the hospital, one of many rotations she’ll experience this year.
Many of those she sees each day as part of a team of professionals have substance-abuse issues, she said, adding that it was work in this realm several years ago at the Riverbend Medical Group that inspired her to go to medical school and pursue work in that field.
“We admit patients, evaluate them, treat them as necessary, and monitor their progress,” she explained, adding that such individuals are then released either into the community or to a treatment facility.
This is work she finds rewarding on a number of levels, especially when she and other members of a team can change the course of someone’s life.
“I did a lot of substance-abuse treatment before medical school, and found it’s a field that I really like,” she said of her chosen path in healthcare. “It’s very much on the front lines, and it’s an opportunity to help someone who may have hit rock bottom. That’s a tragic state of being for a person, and if I can be there in the moment and try to help someone come out of that, get through that … that’s very important to me; it’s very meaningful.”
Local Flavor
As she walked with BusinessWest to the NICU for a few photos, Rockwell pointed to a small courtyard area where staffers can enjoy a meal or a quiet moment.
“That’s where I used to bring pizza for my dad,” she said, adding that she would often deliver him snacks when he was on call for stints that could last 24 hours or more.
Soon, the two might be sharing lunch or dinner there again, only this time they’ll both be wearing white coats and badges identifying them as doctors.
That journal entry logged all those years ago hasn’t officially come to fruition yet, but the younger Rockwell is a giant step closer to making it all reality.
For now, though, she’s another of Baystate’s local residents, and one of many happy to be back home.
George O’Brien can be reached at [email protected]