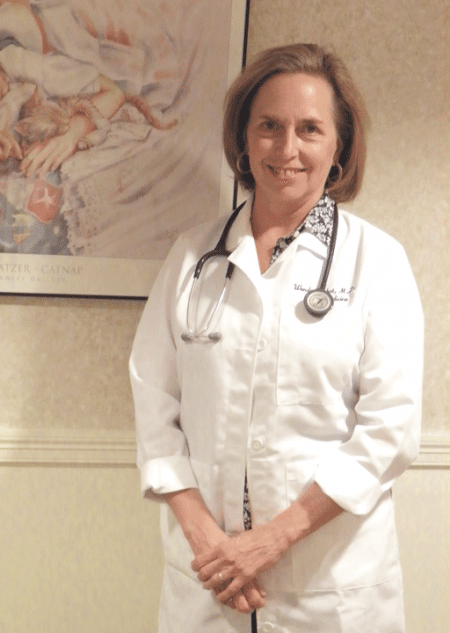
Skeletal System
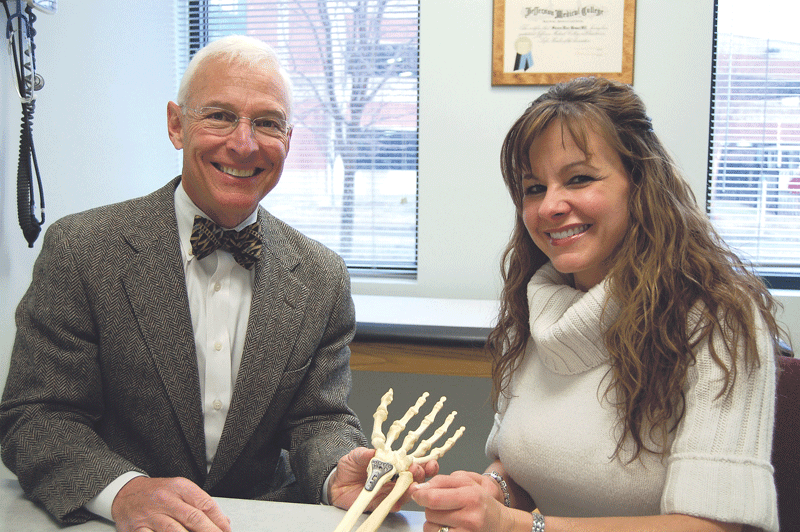
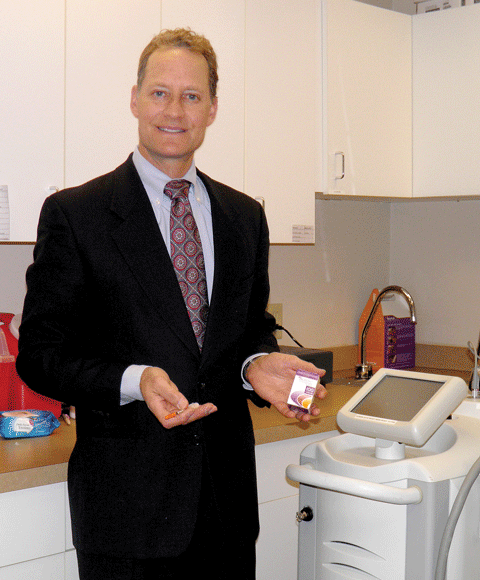
Dr. Steven Wenner, who specializes in hand surgery, and nurse practitioner Jessica Drenga show off a model of the bones beneath the skin.
Rehabilitation is a very broad term in the medical community, encompassing a range of services — ambulatory, cardiac, developmental, the list goes on — with one basic aim: to help patients achieve, or rediscover, the quality of life they desire. This story and the ones that follow demonstrate how area facilities are doing just that.
Thirty years ago, Dr. Joseph Sklar and Dr. Sumner Karas were among a group of physicians who gave birth to a medical practice that was ahead of its time: a place where every orthopedic surgeon had a subspecialty and only saw patients whose problems related to their area of expertise.
New England Orthopedic Surgeons (NEOS) was opened in 1987 by seven doctors and three physician assistants who made the decision to merge Mulberry Orthopedics and Chestnut Orthopedics, which were both in Springfield. The roster of physicians included Sklar and Karas, who met doing their residencies and fellowships at Mass General Hospital, liked the model they saw there that focused on subspecialties, and presented the idea to their partners, which became a central focus as they orchestrated the merger.
Over the past three decades, the practice has been highly successful. It has grown to 18 physicians and 22 physician assistants who see 700 patients a day in their Springfield office and two physical-therapy locations.
“We were a little ahead of the game, but thought this was the best way to deliver optimal patient care,” Sklar told BusinessWest, explaining that the idea stemmed from the belief that, if a doctor focused all of his or her energy on a subspecialty and did the same surgery frequently, their skill would improve, which would result in improved patient care and outcomes.
“We also believed if each doctor specialized in one area, the likelihood would increase that they would be able to recognize unusual problems and know the best way to treat them,” he added.
At the time, no studies had been done to substantiate these beliefs, but over the past several decades, a wide range of benefits from treatment by subspecialists have been documented; they range from accurate diagnoses to a low incidence of post-operative complications.
Today, NEOS is the largest surgical orthopedic practice in the Pioneer Valley. Patients range in age from infants to people in their 90s, although children who need reconstructive surgery for conditions such as congenital hip or spinal disorders or a club foot are usually treated at Shriners Hospitals for Children in Springfield.
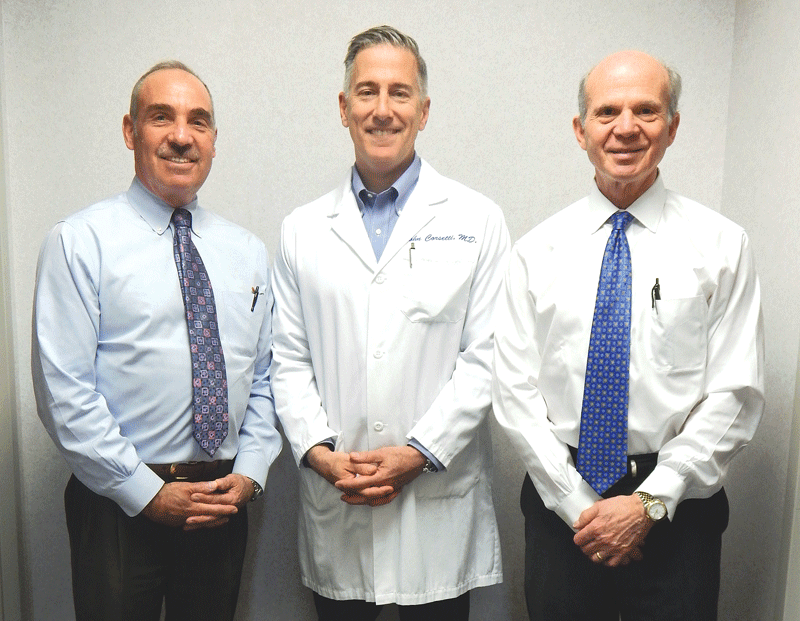
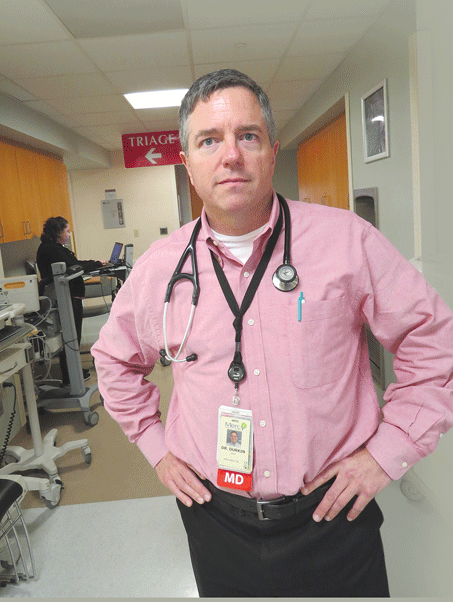
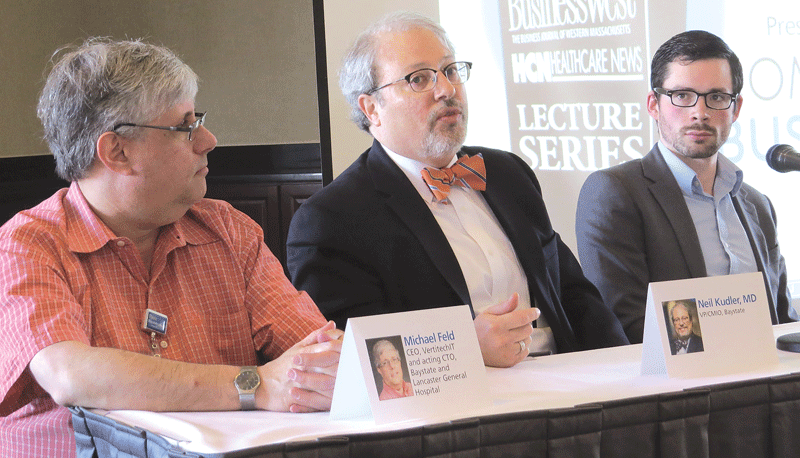
Dr. Sumner Karas, Dr. John Corsetti, and Dr. Joseph Sklar say New England Orthopedeic Surgeons has grown to be the largest subspecialty practice of its kind in Western Mass.
But NEOS does provide care for many young people with traumatic injuries that include broken bones, dislocated shoulders, meniscus tears, or other sports-related problems.
Dr. John Corsetti, who specializes in sports medicine, arthroscopy, and shoulder and knee surgery, joined NEOS in 1995. He was impressed by the practice and said the number of surgeries its physicians perform today is significantly higher than orthopedic groups in Boston.
“Orthopedic surgeons in private practice usually do about 300 to 400 surgeries a year, but our doctors can do as many as 1,300 every year,” he said, noting that many of their patients are referred by other doctors for diagnosis refinement and confirmation.
The practice continues to grow, and on June 5 a new location was opened on Benton Drive in East Longmeadow with the goal of making care more convenient for patients who live in that area or in Connecticut. To that end, the NEOS physical-therapy office in the Sixteen Acres area of Springfield also moved to East Longmeadow.
Two new jobs for physician assistants were created, and an aggressive growth plan is in place for the future, but in the meantime, changes have been put into place that have reduced the time it takes to get an appointment.
In the past the wait was often several months, but NEOS has established a waiting list, and as soon as an appointment is cancelled, a receptionist picks up the phone and begins calling people until someone is found to fill the slot. It has led to 80 additional appointments each week, due in part to a ripple effect: when a cancellation slot is filled, the appointment time the person originally scheduled opens up.
In addition, X-rays no longer need to be taken in advance of an appointment. They can be done while the patient is in the office, which makes it easier for people to get the care and treatment they need in an expedited manner.
For this issue and its focus on rehabilitation and sports medicine, BusinessWest examines the growth of NEOS, the types of problems its doctors treat, and its plans for the future.
Storied History
Karas and Sklar moved to Springfield from the Boston area after completing orthopedic fellowships, which requires an extra year of training in a specialized area after a surgeon fulfills his or her residency requirements.
Sklar joined Mulberry Orthopedics, while Karas joined the Chestnut practice, and although they knew each other, they never dreamed they would play a major role in developing the largest orthopedic practice in Western Mass.
Sklar told BusinessWest he had enjoyed working with children at Boston Children’s Hospital, and one of the things that attracted him to Mulberry Orthopedics was the fact that its doctors provided staffing for Shriners.
It turned out that surgeons from both Mulberry and Chestnut covered for each other on weekends there, and the relationship between Sklar and Karas deepened through their shared work ethics and similar beliefs.
When the decision to merge and form NEOS was made, the two practices had nine doctors between them, but one retired and another moved, leaving seven doctors when the group opened their doors at 300 Carew St. in Springfield.
But forming the new partnership was a complex endeavor. In addition to requiring complete trust and a willingness to send each other patients, there were also financial implications. Since the surgeons agreed to see only patients whose problems fell into their areas of specialized expertise, they had to find a way to share incomes, because limiting their work meant some were no longer doing routine procedures that accounted for a significant percentage of their earnings.
But NEOS quickly became known, and as referrals from other orthopedic surgeons with challenging cases as well as the general public mushroomed, it added a physical-therapy area to its medical office.
“It allowed us to work closely with the therapists, which was particularly important for post-operative patient care,” Karas said, adding that it also enhanced their goal of providing the highest quality of care possible.
Fifteen years ago, NEOS moved to a much larger location at 300 Birnie Ave. in Springfield, and today, it is the only subspecialized comprehensive orthopedic surgical practice in Western Mass. Its physicians are all board-certified and focus on sports medicine, knee and hip replacements, hand and wrist care, foot and ankle surgeries, total joint care, trauma and fracture care, spine care, and orthotic services.
Each surgeon has completed a fellowship in at least one of these areas, but the physician assistants and nurse practitioners are generalists.
“This is important because sometimes it is not clear what the problem is; the neck can cause shoulder pain, while a problem with the spine can result in pain in the hip or knee,” Sklar explained, adding that PAs often determine which doctor the patient should see.
Surgery accounts for only half of the services provided at NEOS because medications, different types of injections, and physical therapy are often the best way to treat muscular-skeletal problems. For example, frozen shoulders can be helped with injections, people with arthritis in their knees or shoulders can experience relief with the help of medication and physical therapy, tendinitis in the hands can improve with splints, and ankle pain can be relieved with a splint or brace, which patients often get before they leave the practice, thanks to the wide array of durable medical equipment that NEOS stocks in its office.
A large number of the surgeries undertaken by NEOS physicians are performed at Baystate Orthopedic Surgery Center, and the results are reviewed by Baystate Medical Center.
“We also keep up with technology,” Karas said, adding that NEOS adopted an electronic medical-records system, has digital X-ray machines, and does casting on site.
Patients also benefit from communication that takes place between the surgeons, especially when a case involves complex injuries. “We come up with a plan and help each other with surgery, which gives everyone a great deal of comfort,” Corsetti said.
Sklar says being able to focus on one aspect of orthopedic medicine gave him the time and experience to create tools and implants that would make a difference in knee surgery, which, coupled with sports medicine, has been his primary focus.
He designed and co-designed two fixation devices that anchor grafts to reconstruct torn ACL ligaments into the bones inside the knee, has developed tools to make arthroscopic surgery more successful, secured a grant from the National Institutes of Health to study the effect of a patient’s outlook on their recovery from ACL surgery, and is an advocate of preventive measures that athletes or anyone engaging in exercise can take to avoid injury.
Changing Landscape
Corsetti said NEOS treats every type of orthopedic problem, and has a large population of patients with degenerative disorders. It continues to specialize and keep current in its respective fields, but thanks to minimally invasive surgical procedures, the length of a hospital stay after surgery has been greatly reduced.
“People used to be in the hospital for five to seven days after a total knee replacement, but now are in for two or three days. In the past, a shoulder surgery could involve a five- to seven-day stay, but today people sometimes return home right after it,” Corsetti told BusinessWest, noting that 60% of the patients they operate on go home the same day and often return to work several days later.
It’s all part of staying ahead of the curve in an ever-changing field, which NEOS has done since its early beginnings when Sklar, Karas, and their partners imagined a new way of delivering orthopedic care in Western Mass. — and made it a reality.




 As the Baby Boom generation continues to hurtle into their retirement years, about 15% of all Americans today are over age 65, a percentage expected to soar to almost 22% by 2040. That demographic tide presents both challenges and opportunities for senior-living facilities, which more than ever are emphasizing a continuum of care and a resident-centric experience.
As the Baby Boom generation continues to hurtle into their retirement years, about 15% of all Americans today are over age 65, a percentage expected to soar to almost 22% by 2040. That demographic tide presents both challenges and opportunities for senior-living facilities, which more than ever are emphasizing a continuum of care and a resident-centric experience.


















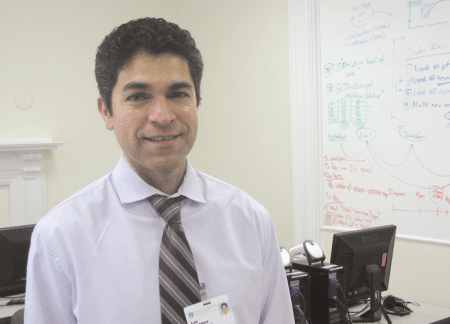
 Keroack is board-certified in internal medicine and bariatric (weight-management) medicine, and originally built his practice around weight loss, moving gradually into a broader wellness focus, where patients lose weight as just one benefit of a total lifestyle shift. But in addition to his formal training, he has certifications from the Institute of Functional Medicine and the Cenegenics Education and Research Foundation for Age Management Medicine.
Keroack is board-certified in internal medicine and bariatric (weight-management) medicine, and originally built his practice around weight loss, moving gradually into a broader wellness focus, where patients lose weight as just one benefit of a total lifestyle shift. But in addition to his formal training, he has certifications from the Institute of Functional Medicine and the Cenegenics Education and Research Foundation for Age Management Medicine.