This Critical Team Provides Hope — and a Roadmap to Recovery

Team members of the Addiction Consult Service at Holyoke Medical Center, from left: Eddie Rodriguez, John Martinez, Lauren Carpenter, Maria Quinn, Kelly Jean Deming, Em Moulton, and Jose Ramos.
Patrick Hamel remained calm and collected as he chronicled his quarter-century-long battle against addiction.
In telling that story, he recalled more relapses than he could count; how he lost jobs, alienated family and friends, and had run-ins with the law (including some B&Es to support his drug and alcohol use); getting thrown out of the house by his wife on a few occasions; the awkwardness of having his daughter visit him in a halfway house; and even that night a little more than two years ago when he decided that enough was enough and tried to end his life.
He didn’t become emotional — though he did have to stop and collect himself a few times — until he started talking about the Addiction Consult Service (ACS), or the Recovery Support Team, as members call it, at Holyoke Medical Center’s Comprehensive Care Center (CCC) and, especially, Maria Quinn, the charismatic psychiatric mental-health nurse practitioner and leader of that unit.
That’s because Quinn, those who work with her, and those to whom she has referred Hamel have enabled him to move beyond all that has happened to him and now lead a much better life.
“She just listened, and we came up with a plan. She got me hooked up with an amazing therapist. We saw each other every week — she was there for me; she was my support.”
“She is so amazing; she’s like my knight in shining armor,” said Hamel, who would then concisely and effectively sum up what Quinn and other members of this team do. “She just listened, and we came up with a plan. She got me hooked up with an amazing therapist. We saw each other every week — she was there for me; she was my support.
“Mind you, I’ve been in other types of medical treatment facilities and other programs,” he went on. “And I always felt like I was a number, or I was there to meet a quota; it was just a job. You can see with Maria that it’s not just a job; it’s something she’s passionate about.”

Patrick Hamel says those at the Addiction Consult Service listened and helped him come up with a game plan for recovery.
Hamel didn’t nominate the ACS for the Healthcare Heroes award, but his words, and the emotion attached to them, help explain why this special unit is being honored this year in the Community Health category.
In short, there are now hundreds, if not thousands, of people, who would say the same things if they were asked — about not just what the ACS does, but how it goes about its difficult and critically important work.
“We’re essentially ever-present — we like to make jokes that we stalk our patients while they’re here, even if we’re not fully involved,” she explained, adding that this is her way of saying that Recovery Support Team members make sure that those patients with addiction issues, either from the Emergency Department or inpatient units at the hospital — many of whom don’t have anyone to visit them while they are in the hospital, for many of the reasons Hamel listed above — have someone to talk to. And, far more importantly, someone to listen, someone who can help them determine what comes next for them, whatever that might be, including ongoing support at the CCC.
“That connection needs to happen so that people can stay and continue to get the treatment that they need,” said Quinn, adding that one of the goals of the program is to build trust among those touched by the ACS, because such trust has often been missing, and it is a key ingredient in their success.
“Historically, people with addiction haven’t been treated well in the healthcare system, so there’s a lot of mistrust, and we see that,” she noted. “We talk about it often and sense that the wall may be coming down and people are starting to bloom because we see our patients become a little more trusting.”
“One thing I’ve learned in this process is that everyone’s recovery is different. You have to listen to the patient to understand what they’re looking for in their recovery. By listening to them, I’ll know what kind of direction I can give them.”
Lauren Carpenter, a certified addictions nurse, agreed. When asked how she got into this specific line of work and what she likes about her work with this constituency, she said simply, “being able to help and care for people who aren’t used to being helped and cared for — building that connection and that rapport and making sure they know there is someone there who cares.”
The ACS is comprised of a nurse practitioner, a certified addictions nurse, a recovery-support coordinator, and recovery coaches. And, as noted, it is a collaborative effort, involving partners such as Tapestry Health, the Gándara Center (which employs the recovery coaches), River Valley Counseling Center, Hope for Holyoke, and the Holyoke Health Center. Together, these agencies are working to reduce opioid overdoses and help people like Hamel find a path to a better life.
The positive results of their efforts can be seen — and heard — with people like Patrick Hamel and countless others like him.
The Power of Hope
John Martinez’s battle against addiction was and is very similar to Hamel’s.
He described several stints of incarceration, homelessness, and, by his count, four suicide attempts.
He’s been sober now for 13 years and has spent the last several as a certified recovery coach, helping others find the strength and conviction to change their lives, as well as needed referrals and direction. The process starts simply with providing hope that life can get better, he said, adding that this isn’t all that coaches provide, but it may well be the most important thing.
“I remember being hopeless — I know what that’s like,” he recalled. “One thing I’ve learned in this process is that everyone’s recovery is different. You have to listen to the patient to understand what they’re looking for in their recovery. By listening to them, I’ll know what kind of direction I can give them.”

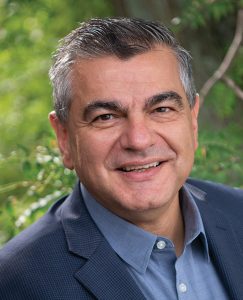
Recovery coach John Martinez says that, among other things, he provides those he counsels with the hope that life can get better.
As noted, recovery coaches are part of the team at the Comprehensive Care Center, and part of a broad, collaborative effort that has come together at a critical time for the Greater Holyoke area.
Indeed, while much of the focus the past few years has been on the pandemic, and understandably so, addiction has only become a bigger, more dangerous, and more deadly problem for the region.
The number of opioid-related overdose deaths increased 9% in Massachusetts in 2021 over 2020. Meanwhile, there are significant disparities in overdose rates, particularly among Black and Latino individuals in Massachusetts; from 2019 to 2020, there was a 70% increase in overdose deaths among Black/non-Hispanic individuals and a 10% increase in Hispanic/Latinx individuals. From 2020 to 2021, there was a 6% decrease in Black/non-Hispanic deaths and an increase of more than 7% for Hispanic/Latinx individuals, according to the Massachusetts Department of Public Health.
Steadily rising numbers over the past several years prompted the HEALing Communities Study, whereby scientists from the nation’s leading health agencies and four major academic institutions are partnering with communities in four states, including Massachusetts, to test a set of interventions designed to reduce overdose deaths by 40% over three years in participating communities.
Through a grant awarded to Boston Medical Center, a collaborative was created involving several agencies in Greater Holyoke, with Quinn taking the lead as the appointed addiction expert for the Holyoke community. The goal is to address opioid use, with a specific focus on overdoses, she said, adding that the linchpin of the initiative was creation of the ACS and the CCC.
“Prior to that, it was just me trying to do it all — start people on medication, get referrals out, try to make appointments, trying to get people to stay here [the hospital] — and it was challenging.”
“Our goal is not to cure them; our goal is to treat them with dignity and respect, and that includes treating their withdrawal. It includes giving education and resources. Some people decide that they no longer want to use and want to work toward abstaining and not using, and some don’t.”
With the grant funds, Quinn was able to hire Carpenter as well as a recovery-support coordinator and other team members.
Together, they have put together a system to “find patients,” said Quinn, noting that, before creation of the ACS, many would essentially fall through the cracks.
“Lauren became really good at figuring out which patients we should look at, and we started finding our patients and going to them, often intervening even before a consult was sent,” she told BusinessWest. “And that’s important because people would be leaving the hospital; if you were using opioids or were addicted to opioids, in particular, and didn’t get that, you would feel really, really sick, and if your withdrawal wasn’t being treated, you would probably be leaving.
“So we’d introduce ourselves and let people know why were there,” she went on, adding that, by and large, patients were not used to such a “proactive and impactive” approach to their care, and would have questions about what they could do for them.
What they can do is listen and begin a discussion about what happens next, said Carpenter, who walked through what might be a typical case.
“Someone will come into the ED, and I’ll get notified that this person is there and that they are in withdrawal,” she explained. “At that point, I will meet with the person, gather a history, assess their withdrawal, and then I’ll get Maria involved. I’ll talk with the ED provider, Maria, the addiction consult … Maria will meet with the patient, give recommendations, and order appropriate medications to treat their withdrawal. And when someone is actually on the med floor, we’d start the discussion of ‘what do you want to do from here?’”
As Quinn noted, the course varies with the patient. Often, those at the ACS will connect them to opioid-treatment programs, including two in Holyoke, if they are not already in a program, or connect them with a recovery coach while they are in the hospital.
“Not everyone’s goal is abstinence,” she said. “Our goal is not to cure them; our goal is to treat them with dignity and respect, and that includes treating their withdrawal. It includes giving education and resources. Some people decide that they no longer want to use and want to work toward abstaining and not using, and some don’t.”
When asked how those at the ACS measure success, Quinn said it depends on what how the patient would define that term.
“For some people, having air in their lungs is successful,” she told BusinessWest. “Anyone who leaves here feeling that they’ve been treated well … that’s a big success for me.”
Impact Statement
As he talked about Quinn and those she works beside at the CCC, Hamel stressed the present tense.
He is still working with these individuals at the CCC, and they are still making a huge impact on his recovery. He’s not sure they, and especially Quinn, understand just how much of an impact. So, he made it clear.
“I wouldn’t be where I am without them,” he said, adding that these individuals are more than healthcare providers, but are, in many respects, friends and even family.
“They want to make a difference — it’s not just about an f-ing paycheck,” he said in conclusion. “That’s where I get a little passionate and emotional; two years ago, I wanted to kill myself, and now…”
He didn’t finish the sentence, but didn’t really have to. The pause explained not only the journey from where he was to where he is now, but why the Addiction Consult Service is truly a Healthcare Hero.
George O’Brien can be reached at [email protected]