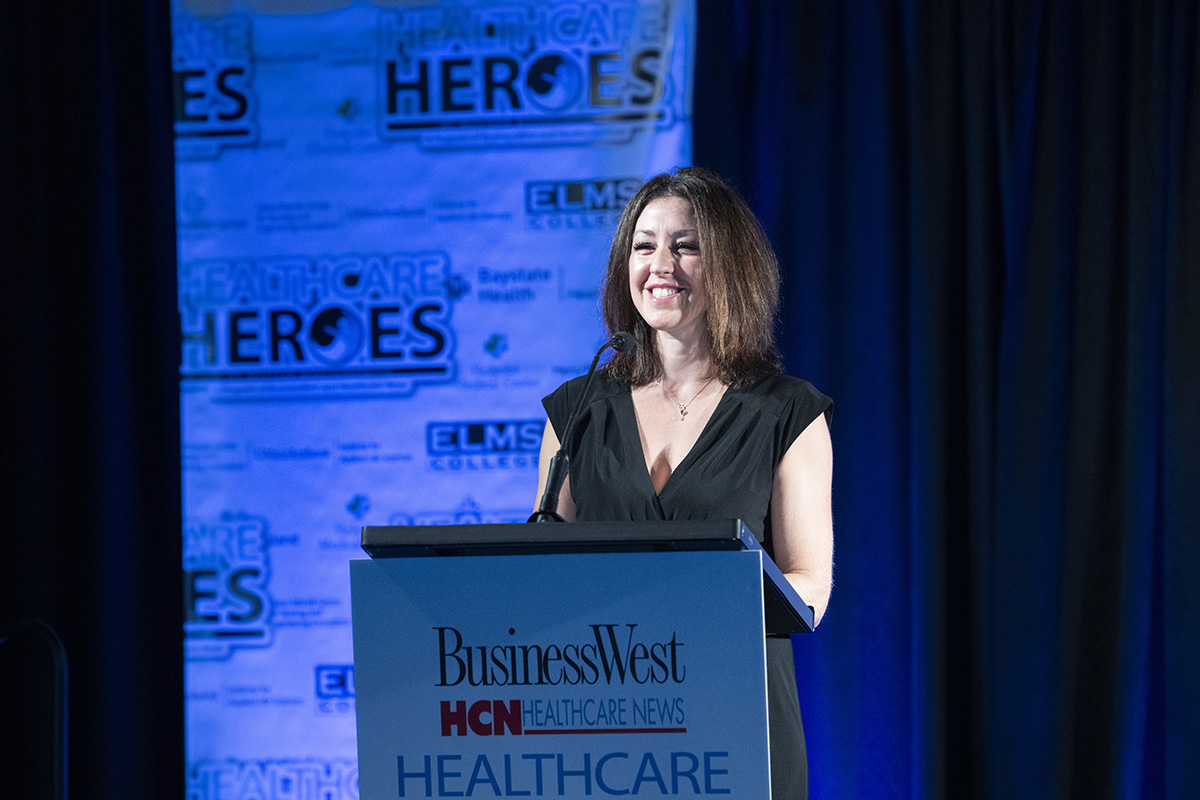
Practice Manager of Thoracic Surgery, Nursing Director of the Lung Screening Program, Mercy Medical Center
She Has a Proven Ability to Take the Bull by the Horns

It’s been seven years now, but Ashley LeBlanc clearly remembers the day Dr. Laki Rousou and Dr. Neal Chuang asked her to consider becoming the nurse navigator for their thoracic surgery practice at Mercy Medical Center.
She also clearly remembers her initial response to their invite: “absolutely not.”
She was working days in critical care at the hospital at the time, and liked both the work and the schedule: three days on, four days off, she told BusinessWest, adding that it takes a while for a new position like this to get approved and posted, for interviews to take place, and more — and the doctors used the following weeks to make additional entreaties, with reminders that she wouldn’t have to work any weekends or holidays.
But the answer was still ‘no’ until roughly six months after that initial invite, when she had one particularly challenging day on the floor with a very sick patient. Challenging enough that, when Rousou tried one more time that afternoon, ‘no’ became “I’ll update my résumé and hear you out.”
“He got me at a weak moment, and it was the best decision I ever made, because they have been amazing mentors, and they’ve opened my mind up to this whole other world,” she said, adding that her career underwent a profound and meaningful course change, one that led her to being named a Healthcare Hero for 2023 in the Emerging Leader category.
Indeed, during those seven years, LeBlanc has emerged as a true leader, both in that thoracic surgery practice, which she now manages, and in efforts to promote awareness and screening for lung cancer — one of the deadliest cancers, and one she can certainly relate to personally. Indeed, she has lost several family members to the disease, many of whom would have qualified for screening had it been available at the time of their diagnosis.
“He got me at a weak moment, and it was the best decision I ever made, because they have been amazing mentors, and they’ve opened my mind up to this whole other world.”
In many respects, and in many ways, she has become a fierce advocate for patients related to lung cancer screening, treatment, and research, and concentrates her efforts on ways to decrease the mortality rate of lung cancer and break down the stigma of that disease by educating the community, connecting them to resources, and, in many respects, guiding them on their journey as they fight lung cancer.
When the screening program was launched, those involved didn’t really know what to expect, LeBlanc said, adding that, in the beginning, maybe a handful of people were being screened each month. Now, that number exceeds 250 a month, and while only a small percentage of those who are screened have lung cancer, she said, each detected case is important because, while this cancer is deadly, early detection often leads to a better outcome.
This is turning out to be a big year for LeBlanc, at least when it comes to awards from BusinessWest. In the spring, she suitably impressed a panel of judges and became part of the 40 Under Forty Class of 2023. And in late October, she’ll accept the Healthcare Heroes award for Emerging Leader.
The plaques on her desk — or soon to be on it — speak to many qualities, but especially an ability to work with others to set, achieve, and, in many cases, exceed goals, not only with lung cancer screening, but other initiatives as well.

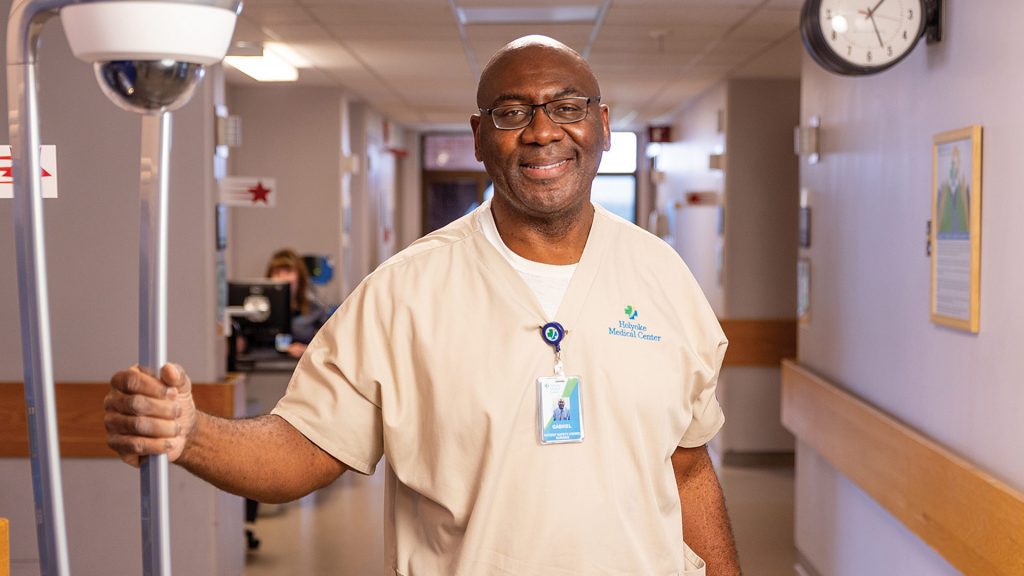
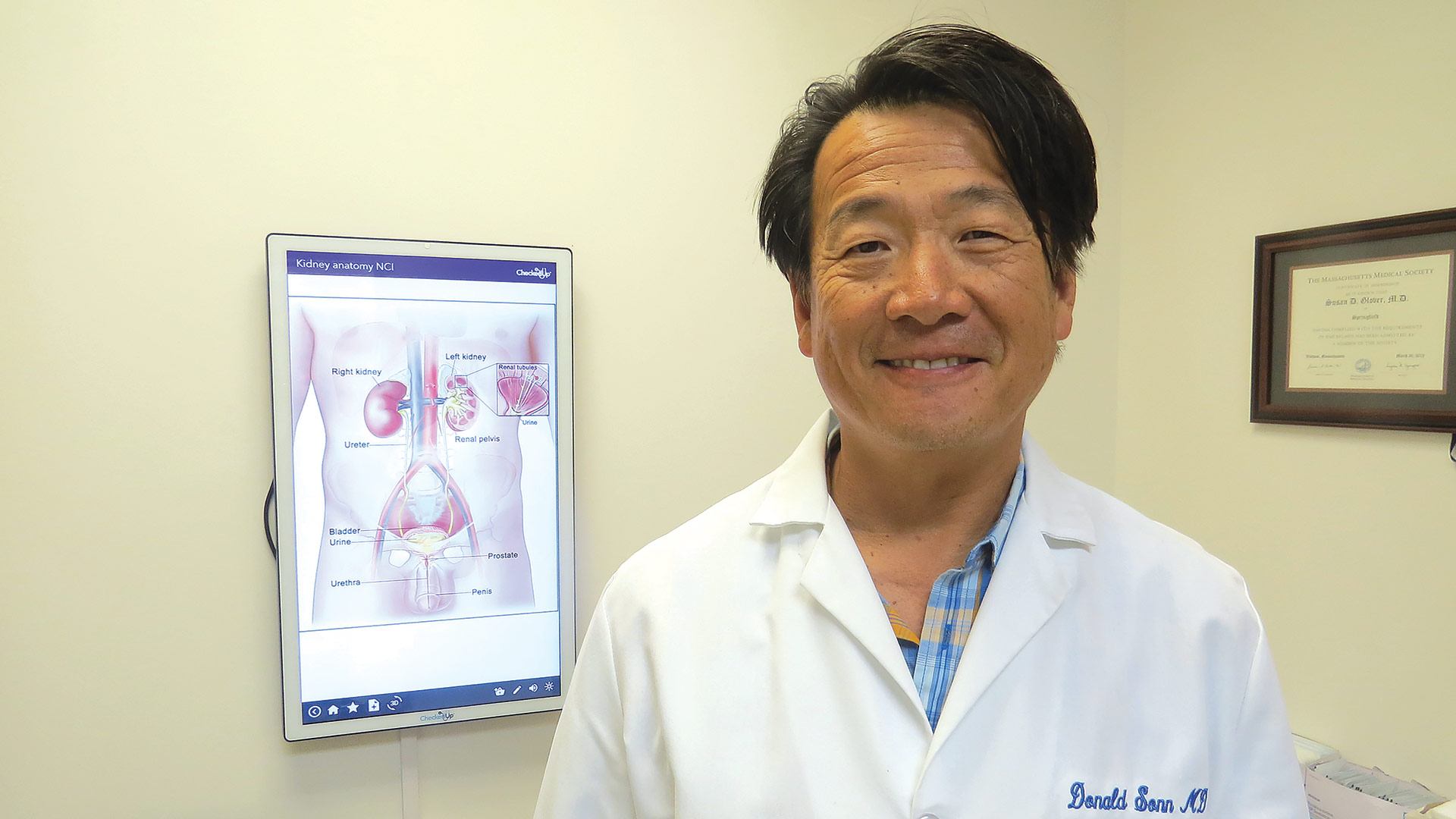
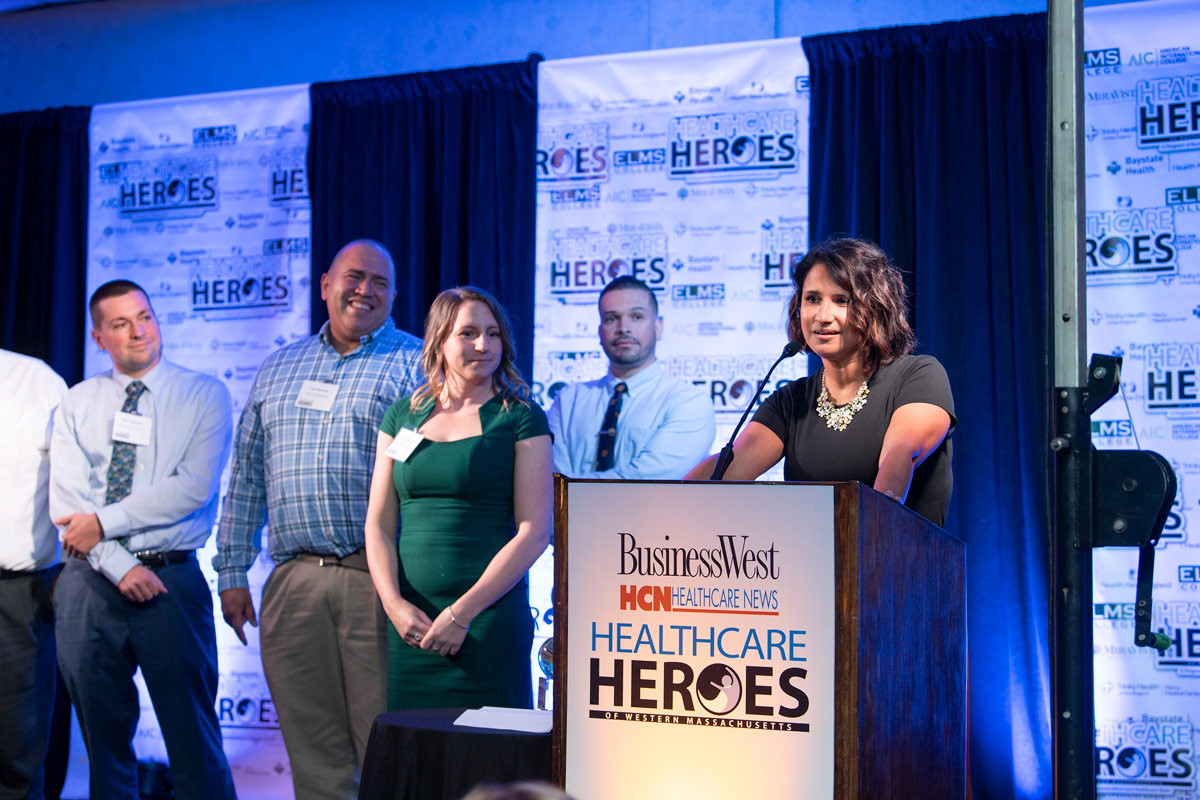
Dr. Laki Rousou never stopped trying to recruit Ashely LeBlanc to manage the thoracic-surgery practice at Mercy Medical Center, and he — and many others — are glad he didn’t.
Staff Photo
Rousou put LeBlanc’s many talents in their proper perspective.
“Before we even had the formal program, I would say something sort of off the cuff, like, ‘I wish we could do this’ … and the next week, I would have the answer, or it would be done,” he said. “Then it turned into ‘OK, let’s try and do this,’ and in the next week or two weeks, it would be done. And then it turned into a situation where she would have an idea and we would talk periodically, but she would take the bull by the horns and just do things that were best for thoracic surgery, but also the screening program.”
This ability to take the bull by the horns, and many other endearing and enduring qualities, explains why LeBlanc is a true Healthcare Hero.
The Big Screen
There’s a small whiteboard to the right of LeBlanc’s desk. Written at the top are the words ‘World Conquering Plans.’
This is an ambitious to-do list, or work-in-progress board, with lines referencing everything from a cancer screening program for firefighters to something called a Center for Healthy Lungs, which would be … well, just what it sounds like. “That’s a bit of a pipe dream,” she said. “We’re going to need our own building.”
While it might seem like a pipe dream, if it’s on LeBlanc’s list of things to get done … it will probably get done. That has been her MO since joining the thoracic surgery practice, and long before that, going back, for example, to the days when she worked the overnight shift as a unit extender at Mercy until 7, then drive to Springfield Technical Community College for nursing classes that began at 8.
“Sometimes, I would snooze in the car for 15 or 20 minutes,” she recalled, adding that she wasn’t getting much sleep at that time in her life. “You just do what you have to do to make it happen.”
Initially, she thought what she wanted to make happen was a career in law enforcement — her father was a police officer in Northampton — but her first stint as a unit extender at Mercy, while she was attending Holyoke Community College, convinced her she was more suited to healthcare.
But plans to enter that field were put on ice (sort of, and pun intended) when her fiancé, a Coast Guardsman, was stationed in Sitka, Alaska.
She spent three years there, taking in winters not as bad as most people would think, and summers not as warm as they are here, but still quite nice. And also working for the Department of Homeland Security as a federal security agent for National Transportation Safety Board at Sitka’s tiny airport.
“The evidence is staggering concerning the number of people who have a scan done, and they have an incidental finding, and there is no follow-up for that incidental finding.”
LeBlanc and her husband eventually returned to Western Mass. after a stint on the Cape, and she essentially picked up where she left off, working as a unit extender at Mercy.
“It was five years later, and it felt like I never left,” she said, adding that she soon enrolled in the Nursing program at STCC and, upon graduation, took a job on the Intermediate Care floor, which brings us back to the point where she kept saying ‘no’ and eventually said ‘yes’ to Rousou and Chuang (who is no longer with the practice).
Rousou told BusinessWest they recruited her heavily because they knew she would be perfect for the role they had carved out — and they were right.
Over the past seven years, LeBlanc has put a number of line items on the ‘World Conquering Plans’ list, and made most of them reality, especially a lung cancer screening program, which wasn’t even on her radar screen when she finally agreed to interview for the job.
Indeed, she was prepared to talk about patient education and how to improve it and make it more comprehensive when Rousou and Chuang changed things up and focused on a screening program.
Thinking Big
Once she got the job, she focused on both, with some dramatic and far-reaching results.
As for the screening program, she said such initiatives were new at the time because the Centers for Medicare Services had only recently approved insurance coverage for such screenings. At Mercy, with Rousou, Chuang, and, increasingly, LeBlanc charting a course, extensive research was undertaken with the goal of incorporating best practices from existing programs into Mercy’s initiative.
“We had no idea what our expectations should be or how it would be received in the community — it was a very new thing,” she recalled. “That first month in 2017, we did seven scans; then we did 29, and by the end of the year, it was over 50 scans a month. A year after we started, it was over 100.”
Now, that number is more than 250, she said, adding that such screenings are important because, while lung cancer is the deadliest of cancers, there are usually no visible signs of it — such as unexplained weight loss, coughing up blood, or pneumonia — until its later stages.
“When patients are diagnosed with stage 4 lung cancer, the treatment is, by and large, palliative, not curative,” she explained, “which makes it extra important to try to diagnose these people with lung cancer at an earlier stage.”
In addition to her work coordinating the screening program, LeBlanc also handles work implied by her initial title — nurse navigator.
This is work to help the patient understand and prepare for the procedure they are facing, such as removal of a portion of their lung, and answer any questions they may have.
“When the surgeon leaves the room … that’s when a patient will take that deep breath and say, ‘I have so many questions,’” she told BusinessWest. “It can be overwhelming, and this gives me an opportunity to answer those questions, which can involve anything from the seriousness of the procedure to where to park or what to bring to the hospital with them.”
Meanwhile, she has taken a lead role in efforts to build a strong culture within the thoracic surgery and cancer screening programs, where 14 people now work, and make it an enjoyable workplace, where birthdays and National Popcorn Day are celebrated, and teamwork is fostered.
“I think it’s important to enjoy where you work, and when we’re happy, I think that carries over to patients, and they feel that,” she said. “At Easter, we have an Easter egg hunt, with grown, professional adults running around the office looking for Easter eggs. It seems silly, but it’s wonderful at the same time.”
Then, there’s that ‘World Conquering Plans’ board next to her desk. LeBlanc said she and the team at the practice have made considerable progress with many of the items on that list, including plans to expand the office into vacated space next door with an interventional pulmonary department and an ‘incidental nodule’ program.
The interventional pulmonary program is a relatively new specialty that focuses on diagnosis of lung disease, she said, adding that an interventional pulmonologist has been hired, facilities have been created, and patients have been scheduled starting early this month.
Progress is also being made on the incidental nodule program, which, as that name implies, is a safety-net initiative focused on following up on the small, incidental nodules on the lungs that show up on scans other than lung cancer screenings and are often overlooked.
“The evidence is staggering concerning the number of people who have a scan done, and they have an incidental finding, and there is no follow-up for that incidental finding,” she explained, adding that such findings often get buried or lost in reports. “When patients come to Dr. Rousou, they’ll often say, ‘I’ve had a scan every year for the last so many years; how come no one saw this until now?’”
Breathing Easier
As for the Center for Healthy Lungs … that is a very ambitious plan, she said, one that exists mainly in dreams right now.
But, as noted earlier, LeBlanc has become proficient in making dreams reality and in drawing lines through items on her whiteboard.
That’s what Rousou and Chuang saw when they recruited LeBlanc — and kept on recruiting her after she kept saying ‘no.’
They could see that she was an emerging leader — and a Healthcare Hero. n


















































































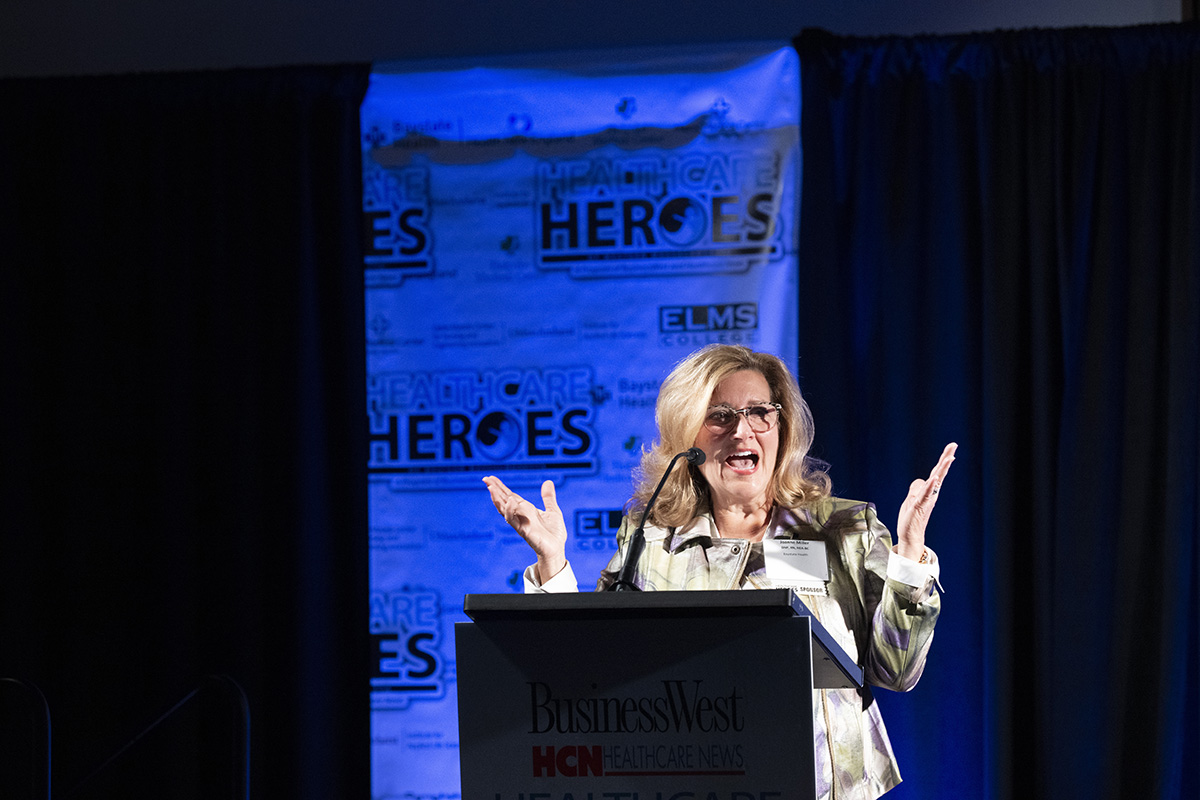















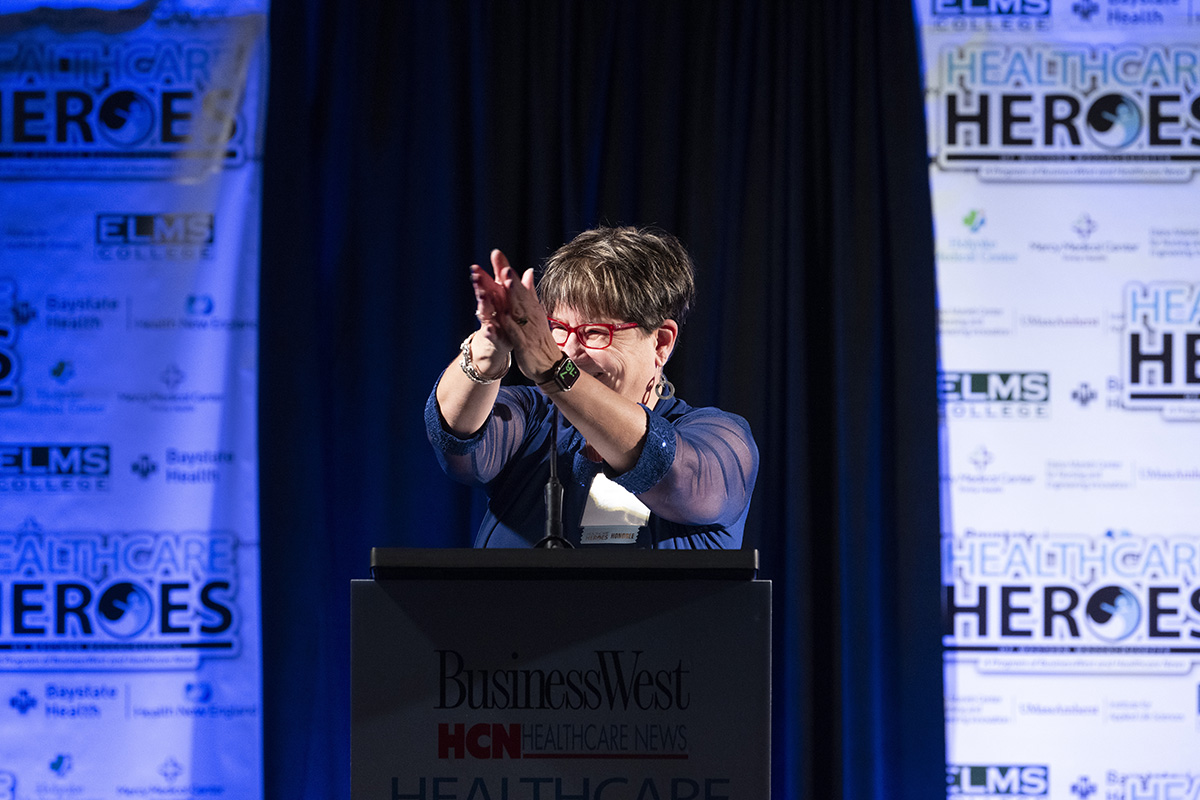













































































































































































































































































































 Since BusinessWest and its sister publication, the Healthcare News, launched the recognition program known as Healthcare Heroes in 2017, the initiative has more than succeeded in its quest to identify true leaders — not to mention inspiring stories — within this region’s large and very important healthcare sector.
Since BusinessWest and its sister publication, the Healthcare News, launched the recognition program known as Healthcare Heroes in 2017, the initiative has more than succeeded in its quest to identify true leaders — not to mention inspiring stories — within this region’s large and very important healthcare sector.