While She Manages People and Programs, Her Job Is About Changing Lives

Katherine Wilson
It’s probably fair to say that the discussions had at the dining room table when Katherine Wilson was in high school were not like those going on in most households in the mid’-60s.
Indeed, Wilson’s father was a physician, specializing in family medicine. Beyond the work at his practice, he was one of the pioneers of a sort when it came to the broad subject of healthcare management.
“From having a solo private practice, he got into the development of systems of delivery of healthcare,” she recalled. “He started an HMO, he was the first medical director of Community Health Center … my father was a big part of the systems that are now in place.
“We had discussions around the kitchen table about healthcare,” she went on. “His interest was in healthcare management, and he was progressive in his thinking at a time when they didn’t have community health centers and they didn’t have HMOs; he did a lot of work with the community physicians and community hospitals.”
One might say that Wilson, certainly inspired by not only those dinnertime talks, but later work at her father’s practice and in one of the first community health centers, has a made a career — a long and very successful career — of working innovatively and in partnership with others to find new and better ways to manage healthcare, and especially mental and behavioral healthcare, in this region and across the Commonwealth.
She’s done this in a variety of settings, most notably, for the past 30 years, as president and CEO of Behavioral Health Network Inc.
Created in 1992 through the merger of four entities — the Child Guidance Clinic of Springfield, Agawam Counseling Center, Community Care Mental Health Center, and the Hampden District Mental Health Clinic — BHN now serves more than 40,000 individuals annually in a service area that stretches across the four western counties.
There are 40 locations in all and more than 2,000 employees. Together, they provide and manage services that come in a variety of forms, from detox centers and ‘step-down’ facilities to a wide variety of counseling services for adults, youth, children, couples, and families; from a 24-hour crisis-intervention service to a host of developmental and intellectual disability services.
“In a society where, even today, stigma may still surround mental illness and those it affects, Kathy not only keenly understands, but goes to every length to help others understand as well. Kathy Wilson has changed innumerable lives for the better, and she’d be the first to say her work is far from finished.”
Wilson has spent the past three decades building and shaping BHN into a $115 million network that continues to expand and find new ways to provide care and a support network to those in need. In recent years, she has been at the forefront of efforts to better integrate general healthcare with behavioral healthcare, particularly in the Medicaid population, with the goal of driving down the ballooning cost of care nationally (more on that later).
And certainly this work to build and manage BHN goes a long way toward explaining why Wilson was chosen as a Healthcare Hero for 2019 in the Lifetime Achievement category. Actually, she is one of two who tied for the high score. The other winner is Frank Robinson, vice president of Public Health at Baystate Health (see story, page 19). Suffice it to say, these two won’t have to introduce themselves when they meet at the Healthcare Heroes gala on Oct. 17. They both worked for the Department of Mental Health in the late ’70s, and both worked to create community programs for residents of Northampton State Hospital and Belchertown State School after those institutions were ordered closed. And they’ve been working in concert on many initiatives ever since.
But there is more to this honor than the vast portfolio of programs and initiatives that is today’s BHN. Indeed, it’s also about a lifetime spent advocating for those with mental illness, substance-abuse issues, or developmental disabilities, anticipating and then meeting their needs, and then asking the difficult but necessary question, ‘what else can be done?’
It’s a philosophy, or mindset, perhaps best summed up with these words from her nomination form, submitted by her daughter, Amy Greeley, formerly a nurse manager at BHN:
“Kathy exemplifies a unique combination of innate compassion and fervent determination that’s led to the helm of a regionally renowned institution. It’s from a position from which she never stops working for greater, more advanced, and even more accessible services for all who need them.”
“In a society where, even today, stigma may still surround mental illness and those it affects, Kathy not only keenly understands, but goes to every length to help others understand as well. Kathy Wilson has changed innumerable lives for the better, and she’d be the first to say her work is far from finished.”
Care Package
It’s called the ‘Living Room.’
As that name suggests, this is a warm, home-like place where anyone age 18 or older can come to “regroup and get help,” said Wilson.
Elaborating, she said the facility, one of many that BHN has carved out of old, mostly unused or underutilized manufacturing buildings in the Liberty Street area, is one of the latest additions to the agency’s portfolio. It was designed for people in a developing crisis, a current crisis, or a post-crisis situation, and is a place where people “can find help from others who have had similar experiences and who can provide support, encouragement, and guidance,” according to a brochure on the facility.
The Living Room, as noted, is just one of dozens of facilities under the BHN umbrella, and its creation speaks to Wilson’s ongoing work — and mission — to continually find new and different ways to meet unmet needs and build support networks for those who desperately need them.
And, as mentioned, this has been her career’s work — going all the way back, in some ways, to those discussions at the dining-room table.
Retracing her route to the corner office at BHN, Wilson said that, after working at her father’s practice and other health settings while in high school and college, she eventually decided that psychology, not healthcare, would be her chosen field; she earned a bachelor’s degree in that field at Denison University and a master’s in clinical psychology at SUNY Plattsburgh.
After a very short stint as a psychotherapist, she applied for a job with the Department of Mental Health, and was hired as a planner during that critical time when Northampton State Hospital and Belchertown State School were ordered to close.
“It was my responsibility to identify individuals from both institutions, look at what their needs were, and see what we could create in the community,” she recalled, adding that she worked to develop some of the group homes that are in use today. “I also worked with agencies that began to adopt the agenda of creating community programs to support people, such as the Community Care Mental Health Center in Springfield, which created day programs so individuals could get some of their rehabilitation in a clinical setting.”
The consent decrees that shuttered the institutions in Northampton and Belchertown coincided with national initiatives imbedded within the Community Mental Health Act, established by President John F. Kennedy. It made federal funds available to create more community systems of care, said Wilson, adding that, locally, a consortium of agencies was created to administer this flow of federal money.
“We got together and said, ‘survival means you have to get bigger, you need to have a stronger base at the bottom to support what we do, and this will give us a platform for growth.”
Called the Springfield Community Mental Health Consortium, it administered a number of initiatives, including hospital supports, group-living environments, outpatient systems of care, emergency services, and more, said Wilson, who transitioned from working for the state to being employed with the consortium as a planner.
“It was my responsibility to help establish the Community Mental Health Center range of services,” she explained. “Now that we had more people in the community living with mental illness, we needed to create the system of healthcare support.”
When the Reagan administration closed the tap on federal money for these services, with funding to be secured through state-administered block grants instead, the agencies that were part of the consortium broke apart and continued to do their own work, said Wilson, who then went to work with Child Guidance Clinic of Springfield, first as Business and Finance director and then executive director of the Child Guidance Clinic of Springfield.
As funding for mental-health programs became more scarce, Wilson said, she and the directors of three other agencies — Agawam Counseling Center, Community Care Mental Health Center, and the Hampden District Mental Health Clinic — decided that the best strategy was to merge those entities into one corporation.
“We got together and said, ‘survival means you have to get bigger, you need to have a stronger base at the bottom to support what we do, and this will give us a platform for growth,’” she recalled, adding that this new entity would become BHN.
And over the years, it would continue to get bigger and widen that base of support, as those administrators knew it had to, through additional mergers and the addition of many new programs.
Room to Grow
As president and CEO of BHN, Wilson wears a number of hats and logs tens of thousands of miles each year traveling back and forth to Boston for meetings on a range of topics and with a host of groups and individuals.
As for those hats, Wilson said she is the face of BHN and, for many, a first point of contact. She also considers herself a problem solver and a “convener,” a strategist, a mentor for many, and even an interior designer.
“I’m often the one that picks the colors for the walls,” she said, referring to the seemingly constant work to open and renovate new facilities, not only at what has become a ‘BHN campus’ off Liberty Street in Springfield, but across the region, while also noting that much goes into to picking those colors.
All those skills have been put to use over the past 30 years, an intriguing time of growth and evolution for BHN as it responds to emerging needs within the community, said Wilson, who cited, as one example, profound expansion into addiction services.
“One of the areas we identified maybe 10 years ago is that we were seeing many more of the parents of the children we were seeing at the Child Guidance Clinic, and many more adults coming in to adult outpatient clinics having mental-health issues co-occurring with substance use,” she explained. “And we said, ‘we can’t just treat mental-health problems without acknowledging the fact that there is a substance-use disorder concurrently, and that we really need to think about building a system of care that serves that population.’”
As a result, BHN collaborated with Baystate Health, which had a community-based system of care that included a detox and some community group-living environments for post-detox care, said Wilson, adding that Baystate asked BHN to manage those facilities and eventually transfer them into its system of care.
“We inherited Baystate’s system of community services for those with addiction,” she said. “And once we did that, we got established with the Department of Public Health and its Bureau of Substance Abuse Services, and we became known as an agency that could handle co-occurring treatments as well as individuals whose primary diagnosis was addiction, and from there, they helped us grow a system of treatment for people with substance-abuse disorder, and that really took off because the state was making significant investments in that world.”
That system now includes two detox operations, two step-down facilities, and a number of beds in what are called ‘residential recovery,’ or group-living facilities, she told BusinessWest, adding that this is just one example of how BHN continues to grow and evolve.
And it’s also just one example of how Wilson has led efforts to improve access to a wide array of care at a time when more people need access. The creation of the Northern Hope Center and Recovery Services in Greenfield, blueprinted in response to needs created by the opioid crisis in Franklin County, is still another case in point.
And these initiatives provide ample evidence of the additional emphasis placed on integrated healthcare and behavioral healthcare with the twin goals of improving population health and bringing down the cost of care, said Wilson, adding that BHN has been at the forefront of these efforts.
“This is what the federal government wants its funding to support, particularly for the Medicaid population,” she explained. “This is the population whose behavioral health — addictions or mental health — really interfere with their managing health.
“You have this small group of people that is driving high costs to Medicaid and both commercial and private insurance,” she went on. “So the move these days is for physicians and healthcare systems to work with behavioral-health systems of care and provide wrap-around services for individuals to see if you can manage the behavioral health, because that will help bring the cost of healthcare down.”
BHN adopted this rather profound operational shift several years ago, said Wilson, adding that, overall, it is part of her job description to keep the agency on the cutting edge of trends and developments in healthcare, while also making sure it remains viable and able to function properly in the years to decades to come.
That means continuing to find more ways to grow the network (the ‘N’ in BHN), building upon its base of support, and developing new methods for providing all-important access to care.
When asked about her most significant accomplishment, she quickly changed the subject of that question to ‘we,’ meaning BHN, but in doing so still managed to sum up her career’s work.
“I think we’ve created excellent, value-based, top-of-the-line service delivery for people who need access, sometimes very quickly, to good treatment,” she noted. “I have excellent medical leadership on both the addiction and behavioral healthcare side, and we hire really good, skilled, competent people. So I think people who are not used to getting good access to care now get it.
“Also, we’ve hired so many people that we have helped come from an addiction to sobriety, reunification, and now they’re BHN employees,” she went on. “To me, that warms my heart to know that people have been able to turn their lives around with the help of BHN.”
Change Agent
Which brings us back to that passage from Wilson’s nomination form. There are a number of key phrases within it that explain why she will be at the podium on Oct. 17 to receive her Lifetime Achievement award.
There’s the part about battling the stigma attached to mental illness, something she’s been doing for more than four decades. There’s also that point about how she would be the first to acknowledge that her work isn’t finished — because it never is.
But perhaps the words to remember most are those concerning ‘changing thousands of lives for the better.’
Indeed, while Wilson manages people, programs, and facilities for BHN, changing lives is what she does for a living.
And that’s why she’s a Healthcare Hero.
George O’Brien can be reached at [email protected]
 This past year was one that saw a number of landscape-changing developments in the broad realm of employment law. From paid family leave to cannabis to overtime-threshold changes, there were a number of changes to existing laws, new measures to keep track of, and new challenges for employers.
This past year was one that saw a number of landscape-changing developments in the broad realm of employment law. From paid family leave to cannabis to overtime-threshold changes, there were a number of changes to existing laws, new measures to keep track of, and new challenges for employers.

















































 Lisa Tanzer, president of Life is Good, has over 25 years of consumer brand experience. Prior to becoming president, Lisa served as the company’s head of Marketing after spending over 20 years on the board of directors of the Life is Good Kids Foundation. She’s held executive positions in the entertainment, ecommerce, and education sectors. Earlier in her career, Lisa held marketing and strategy roles at Hasbro, Staples, The Gillette Company, and PricewaterhouseCoopers. She received her BA from Tufts University and an MBA from Harvard Business School.
Lisa Tanzer, president of Life is Good, has over 25 years of consumer brand experience. Prior to becoming president, Lisa served as the company’s head of Marketing after spending over 20 years on the board of directors of the Life is Good Kids Foundation. She’s held executive positions in the entertainment, ecommerce, and education sectors. Earlier in her career, Lisa held marketing and strategy roles at Hasbro, Staples, The Gillette Company, and PricewaterhouseCoopers. She received her BA from Tufts University and an MBA from Harvard Business School. Taylor Knight joined 22News in July of 2018 as a multimedia journalist. Currently, Taylor is the co-anchor of the 22News weekday morning newscasts and a reporter for the 22News I-Team. Before arriving in Springfield, Taylor was a reporter for FiOS1 News in New Jersey. Taylor began her career as a multimedia journalist in Connecticut, covering news and sports in Fairfield County. Taylor earned her B.A. in broadcast journalism at Temple University in Philadelphia. During college, she interned at WFSB in Connecticut and NBC Sports Philadelphia. In her free time, Taylor enjoys spending time with her dog, running, and watching the Philadelphia Eagles. She is excited to now be “Working for You!”
Taylor Knight joined 22News in July of 2018 as a multimedia journalist. Currently, Taylor is the co-anchor of the 22News weekday morning newscasts and a reporter for the 22News I-Team. Before arriving in Springfield, Taylor was a reporter for FiOS1 News in New Jersey. Taylor began her career as a multimedia journalist in Connecticut, covering news and sports in Fairfield County. Taylor earned her B.A. in broadcast journalism at Temple University in Philadelphia. During college, she interned at WFSB in Connecticut and NBC Sports Philadelphia. In her free time, Taylor enjoys spending time with her dog, running, and watching the Philadelphia Eagles. She is excited to now be “Working for You!”




 Tricia Canavan spent much of her early career as an educator. Today, in a much different role, education is never far from her mind.
Tricia Canavan spent much of her early career as an educator. Today, in a much different role, education is never far from her mind.

 This Radio Pioneer Has Overcome Obstacles to Better Her Community
This Radio Pioneer Has Overcome Obstacles to Better Her Community

 Jean Deliso likes to say she is part financial advisor, part therapist.
Jean Deliso likes to say she is part financial advisor, part therapist.

 ‘Hi, Ellen. I hope all is well. I can’t wait to see you soon and hear all about your trip! My colleague Erica is very interested in getting even more deeply connected to the philanthropic life of the Greater Springfield area. Your name immediately came to mind, and I thought you both would have a lot to discuss.
‘Hi, Ellen. I hope all is well. I can’t wait to see you soon and hear all about your trip! My colleague Erica is very interested in getting even more deeply connected to the philanthropic life of the Greater Springfield area. Your name immediately came to mind, and I thought you both would have a lot to discuss.

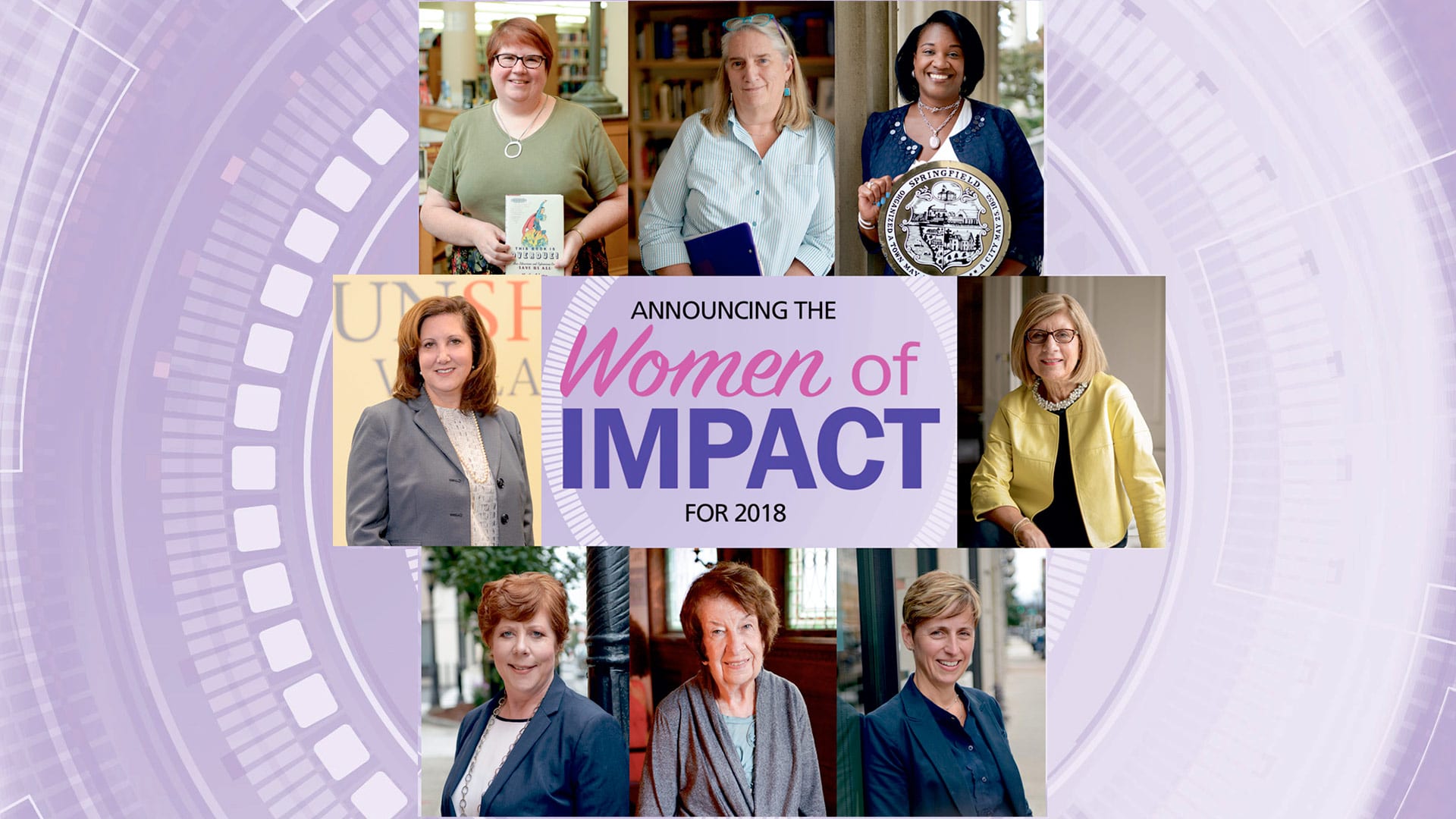
 Former Mayor Says Making an Impact Recharges Her Batteries
Former Mayor Says Making an Impact Recharges Her Batteries




 Girls Inc. Leader Is an Innovator, Role Model, and Inspiration
Girls Inc. Leader Is an Innovator, Role Model, and Inspiration

 This Investor and Mentor Is Making a Difference within the Entrepreneurship Ecosystem
This Investor and Mentor Is Making a Difference within the Entrepreneurship Ecosystem






































 The
The 































































 Rothschild, then development and marketing manager for the Food Bank of Western Mass., was named to the 40 Under Forty class of 2011 mainly for her tireless work in melanoma awareness. A survivor herself, she began organizing local events to raise funds for the fight against this common killer, and launched a website, SurvivingSkin.org, and TV show, Skin Talk, that brought wider attention to her work.
Rothschild, then development and marketing manager for the Food Bank of Western Mass., was named to the 40 Under Forty class of 2011 mainly for her tireless work in melanoma awareness. A survivor herself, she began organizing local events to raise funds for the fight against this common killer, and launched a website, SurvivingSkin.org, and TV show, Skin Talk, that brought wider attention to her work.





























 According to the 2019 Dodge Construction Outlook released by Dodge Data & Analytics, a leader in construction-industry forecasting and business planning, total U.S. construction starts for 2019 will be $808 billion, staying essentially even with the $807 billion recorded in 2018.
According to the 2019 Dodge Construction Outlook released by Dodge Data & Analytics, a leader in construction-industry forecasting and business planning, total U.S. construction starts for 2019 will be $808 billion, staying essentially even with the $807 billion recorded in 2018.




 BusinessWest is now accepting nominations for the 40 Under Forty Class of 2019, a celebration of young business and civic leaders in the Western Mass., and an undertaking in which our readership will play a pivotal role. Indeed, the process of selecting this region’s 40 Under Forty begins with nominations. And we urge you be thorough, because 40 Under Forty is a nomination-driven process; the background material submitted on a given individual is the primary source of information to be weighed by the judges who will score the candidates.
BusinessWest is now accepting nominations for the 40 Under Forty Class of 2019, a celebration of young business and civic leaders in the Western Mass., and an undertaking in which our readership will play a pivotal role. Indeed, the process of selecting this region’s 40 Under Forty begins with nominations. And we urge you be thorough, because 40 Under Forty is a nomination-driven process; the background material submitted on a given individual is the primary source of information to be weighed by the judges who will score the candidates.